Chapter TEN
Nuclear Medicine
R. EDWARD COLEMAN  CHAPTER EDITOR
CHAPTER EDITOR
R. EDWARD COLEMAN
HISTORY
A 54-year-old woman with left knee pain.

 FIGURE 10-1A Anteroposterior view of the left knee obtained at the time of presentation. There is no evidence of a fracture on this radiograph.
FIGURE 10-1A Anteroposterior view of the left knee obtained at the time of presentation. There is no evidence of a fracture on this radiograph.

 FIGURE 10-1B Anterior whole body image of a bone scan obtained 2 hours after the intravenous administration of Tc-99m methylene diphosphate. A focal area of abnormal accumulation is present in the proximal left tibia.
FIGURE 10-1B Anterior whole body image of a bone scan obtained 2 hours after the intravenous administration of Tc-99m methylene diphosphate. A focal area of abnormal accumulation is present in the proximal left tibia.
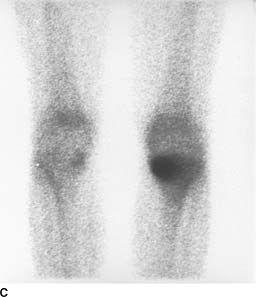
 FIGURE 10-1C Anterior image of the knees. A region of increased radiotracer activity is present in the left tibial plateau, with greater accumulation medially than laterally.
FIGURE 10-1C Anterior image of the knees. A region of increased radiotracer activity is present in the left tibial plateau, with greater accumulation medially than laterally.

 FIGURE 10-1D Anteroposterior view of the left knee obtained 1 month after the initial radiograph and bone scan. A linear region of sclerosis has developed in the medial left tibial metaphysis.
FIGURE 10-1D Anteroposterior view of the left knee obtained 1 month after the initial radiograph and bone scan. A linear region of sclerosis has developed in the medial left tibial metaphysis.
 Metastatic disease: This is an unlikely diagnosis because of the absence of a primary malignancy and because only a single abnormality is present. Multiple abnormalities would be expected with metastatic disease.
Metastatic disease: This is an unlikely diagnosis because of the absence of a primary malignancy and because only a single abnormality is present. Multiple abnormalities would be expected with metastatic disease.
 Osteosarcoma: This diagnosis is unlikely because the tumor usually occurs in the 10- to 25-year age range and is apparent radiographically at the time of presentation.
Osteosarcoma: This diagnosis is unlikely because the tumor usually occurs in the 10- to 25-year age range and is apparent radiographically at the time of presentation.
 Insufficiency fracture: This is the best diagnosis because initial radiographs commonly are normal in the face of an abnormal bone scan, with development of sclerosis at the fracture site demonstrable on radiographs a few weeks later.
Insufficiency fracture: This is the best diagnosis because initial radiographs commonly are normal in the face of an abnormal bone scan, with development of sclerosis at the fracture site demonstrable on radiographs a few weeks later.
 Osteomyelitis: This diagnosis is unlikely because the patient is older than most patients with osteomyelitis and because of the absence of a predisposing factor. Furthermore, at least some radiographic abnormality would be expected in osteomyelitis.
Osteomyelitis: This diagnosis is unlikely because the patient is older than most patients with osteomyelitis and because of the absence of a predisposing factor. Furthermore, at least some radiographic abnormality would be expected in osteomyelitis.
 Degenerative joint disease: This diagnosis is unlikely because the bone scan abnormality is not in the joint space but in the tibial metaphysis. Furthermore, the radiograph does not demonstrate changes of degenerative joint disease.
Degenerative joint disease: This diagnosis is unlikely because the bone scan abnormality is not in the joint space but in the tibial metaphysis. Furthermore, the radiograph does not demonstrate changes of degenerative joint disease.
DIAGNOSIS
Insufficiency fracture
KEY FACTS
Clinical
 Musculoskeletal injury accounts for 15% to 20% of patient visits to emergency departments and 30% of routine orthopedic visits.
Musculoskeletal injury accounts for 15% to 20% of patient visits to emergency departments and 30% of routine orthopedic visits.
 Physical examination and plain film radiography of the site of injury are typically performed at the time of presentation.
Physical examination and plain film radiography of the site of injury are typically performed at the time of presentation.
 Insufficiency fractures occur when bones that are weakened by osteoporosis or other metabolic bone diseases are placed under normal stress.
Insufficiency fractures occur when bones that are weakened by osteoporosis or other metabolic bone diseases are placed under normal stress.
 Stress fractures occur when normal bones are exposed to abnormal stress of a repetitive type.
Stress fractures occur when normal bones are exposed to abnormal stress of a repetitive type.
 Pathologic fractures occur when bones that are weakened by tumor involvement are exposed to normal stress.
Pathologic fractures occur when bones that are weakened by tumor involvement are exposed to normal stress.
Radiologic
 Radiographic studies are often initially normal at the time of development of an insufficiency fracture or a stress fracture. In fact, abnormalities may not be present until 1 to 2 weeks later.
Radiographic studies are often initially normal at the time of development of an insufficiency fracture or a stress fracture. In fact, abnormalities may not be present until 1 to 2 weeks later.
 If pain is considered to be of osseous origin and the plain radiographs are normal, a radionuclide bone scan is the next imaging modality that is generally used to evaluate for a possible fracture. The bone scan will typically be abnormal at that time.
If pain is considered to be of osseous origin and the plain radiographs are normal, a radionuclide bone scan is the next imaging modality that is generally used to evaluate for a possible fracture. The bone scan will typically be abnormal at that time.
 On a three-phase bone scan, acute fractures demonstrate increased perfusion on the dynamic phase, poorly defined abnormal radiotracer accumulation on the blood pool images, and focal abnormal accumulation on delayed images.
On a three-phase bone scan, acute fractures demonstrate increased perfusion on the dynamic phase, poorly defined abnormal radiotracer accumulation on the blood pool images, and focal abnormal accumulation on delayed images.
 Magnetic resonance imaging (MRI) can demonstrate cortical and marrow changes associated with the fracture.
Magnetic resonance imaging (MRI) can demonstrate cortical and marrow changes associated with the fracture.
 Insufficiency fractures in elderly patients with osteoporosis can mimic metastatic disease on plain films.
Insufficiency fractures in elderly patients with osteoporosis can mimic metastatic disease on plain films.
SUGGESTED READING
de Castro SM, Joosse P, Unlii C, Steller EP. Images in emergency medicine. Pain in the leg after jogging. Emerg Med J 2009;26:806.
Holder LE. Clinical radionuclide bone imaging. Radiology 1990;176:607–614.
Holder LE. Bone scintigraphy in skeletal trauma. Radiol Clin North Am 1993;31:739–781.
Krestan C, Hojreh A. Imaging of insufficiency fractures. Eur J Radiol 2009;71:398–405.
Martin P. Basic principles of nuclear medicine techniques for detection and evaluation of trauma and sports medicine injuries. Semin Nucl Med 1988;18:90–112.
SALVADORE BORGES-NETO
HISTORY
A 76-year-old woman with a history of coronary artery disease, hypertension, elevated serum lipids, and atrial fibrillation presents with increasing shortness of breath.
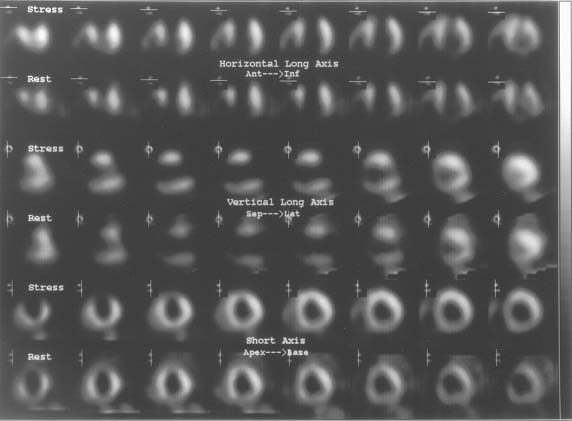
 FIGURE 10-2 Stress (Tc-99m sestamibi) and rest (Tl-201) SPECT myocardial perfusion images displayed in the horizontal long axis (top 2 rows), vertical long axis (middle 2 rows), and short axis views (bottom 2 rows). The stress perfusion images show an area of markedly decreased perfusion involving the low anterior, anteroapical, anteroseptal, and inferoapical regions. The rest perfusion images also show decreased activity in the same areas. The extent and severity of the perfusion defects are essentially the same on the stress and rest perfusion images.
FIGURE 10-2 Stress (Tc-99m sestamibi) and rest (Tl-201) SPECT myocardial perfusion images displayed in the horizontal long axis (top 2 rows), vertical long axis (middle 2 rows), and short axis views (bottom 2 rows). The stress perfusion images show an area of markedly decreased perfusion involving the low anterior, anteroapical, anteroseptal, and inferoapical regions. The rest perfusion images also show decreased activity in the same areas. The extent and severity of the perfusion defects are essentially the same on the stress and rest perfusion images.
 Myocardial infarction without stress-induced ischemia: This is the best diagnosis based on the presence of a fixed perfusion defect with essentially no change in the extent and severity of the perfusion abnormalities between the rest and stress studies.
Myocardial infarction without stress-induced ischemia: This is the best diagnosis based on the presence of a fixed perfusion defect with essentially no change in the extent and severity of the perfusion abnormalities between the rest and stress studies.
 Myocardial ischemia without infarction: This diagnosis is made when a perfusion defect induced by stress is not present on the rest study. This is not the situation in the case illustrated.
Myocardial ischemia without infarction: This diagnosis is made when a perfusion defect induced by stress is not present on the rest study. This is not the situation in the case illustrated.
 Myocardial infarction and stress-induced ischemia: This diagnosis is made when a stress-induced perfusion abnormality incompletely or only partially normalizes on the rest images.
Myocardial infarction and stress-induced ischemia: This diagnosis is made when a stress-induced perfusion abnormality incompletely or only partially normalizes on the rest images.
 Nonischemic cardiomyopathy: Large perfusion defects while at rest, during stress, or during both rest and stress are typically absent in nonischemic cardiomy-opathy. The large defects that are present in this study make this diagnosis unlikely. Furthermore, left ventricular dilatation is a prominent feature of nonischemic cardiomyopathy, a finding that is not present in this patient.
Nonischemic cardiomyopathy: Large perfusion defects while at rest, during stress, or during both rest and stress are typically absent in nonischemic cardiomy-opathy. The large defects that are present in this study make this diagnosis unlikely. Furthermore, left ventricular dilatation is a prominent feature of nonischemic cardiomyopathy, a finding that is not present in this patient.
DIAGNOSIS
Myocardial infarction without stress-induced ischemia
KEY FACTS
Clinical
 Several risk factors are known to predispose to coronary artery disease, including age, family history, hypertension, smoking, and diabetes.
Several risk factors are known to predispose to coronary artery disease, including age, family history, hypertension, smoking, and diabetes.
 Patients with coronary artery disease may present with symptoms of either angina, shortness of breath, or both. However, silent ischemia is a well-recognized entity, particularly in diabetic patients. Such patients can have arterial occlusion and infarction in the absence of symptoms.
Patients with coronary artery disease may present with symptoms of either angina, shortness of breath, or both. However, silent ischemia is a well-recognized entity, particularly in diabetic patients. Such patients can have arterial occlusion and infarction in the absence of symptoms.
 Myocardial infarction with coexistent low left-ventricular ejection fraction (LVEF) is associated with a poor prognosis.
Myocardial infarction with coexistent low left-ventricular ejection fraction (LVEF) is associated with a poor prognosis.
Radiologic
 Myocardial perfusion studies are performed to determine the severity and extent of myocardial ischemia and infarction and to assess prognosis.
Myocardial perfusion studies are performed to determine the severity and extent of myocardial ischemia and infarction and to assess prognosis.
 Tl-201 and Tc-99m sestamibi are myocardial perfusion radiotracers that distribute in proportion to blood flow. There is good correlation between the myocardial per-fusion defect size and the actual infarct size.
Tl-201 and Tc-99m sestamibi are myocardial perfusion radiotracers that distribute in proportion to blood flow. There is good correlation between the myocardial per-fusion defect size and the actual infarct size.
 Tc-99m pyrophosphate and In-111 antimyosin are myocardial infarct imaging radiotracers. These radiotracers are infarct-avid, localizing in infarcted myocardium. However, these radiotracers are used infrequently because the information provided by these agents can be obtained from other tests.
Tc-99m pyrophosphate and In-111 antimyosin are myocardial infarct imaging radiotracers. These radiotracers are infarct-avid, localizing in infarcted myocardium. However, these radiotracers are used infrequently because the information provided by these agents can be obtained from other tests.
 On perfusion imaging, myocardial infarction is typically seen as one or more persistent defects on both rest and exercise studies. However, areas of persistent defects at 4 hours on the redistribution Tl-201 study can decrease or resolve (indicating myocardial viability) after rein-jection or on 24-hour redistribution images.
On perfusion imaging, myocardial infarction is typically seen as one or more persistent defects on both rest and exercise studies. However, areas of persistent defects at 4 hours on the redistribution Tl-201 study can decrease or resolve (indicating myocardial viability) after rein-jection or on 24-hour redistribution images.
 Large perfusion defects are associated with poor left ventricular function and a poor prognosis.
Large perfusion defects are associated with poor left ventricular function and a poor prognosis.
 The term hibernating myocardium refers to regions of wall motion abnormality or ventricular dysfunction that improve on perfusion images at 24-hour redistribution or reinjection Tl-201 studies. Foci of hibernating myocardium are thought to result from chronic reduction in coronary artery blood flow and represent areas of impaired function with reversible myocardial damage.
The term hibernating myocardium refers to regions of wall motion abnormality or ventricular dysfunction that improve on perfusion images at 24-hour redistribution or reinjection Tl-201 studies. Foci of hibernating myocardium are thought to result from chronic reduction in coronary artery blood flow and represent areas of impaired function with reversible myocardial damage.
 The gold standard study for myocardial viability is positron emission tomography (PET) imaging with F-18 fluorodeoxyglucose (FDG) and N-13 ammonia. Approximately 25% of areas with fixed perfusion defects on Tl-201 studies are found to be viable on FDG studies.
The gold standard study for myocardial viability is positron emission tomography (PET) imaging with F-18 fluorodeoxyglucose (FDG) and N-13 ammonia. Approximately 25% of areas with fixed perfusion defects on Tl-201 studies are found to be viable on FDG studies.
SUGGESTED READING
Bonow RO, Dilsizian V. Thallium-201 for assessment of myocardial viability. Semin Nucl Med 1991;21:230–241.
Druz RS. Current advances in vasodilator pharmacological stress perfusion imaging. Semin Nucl Med 2009;39:204–209.
Palmer EL, Scott JA, Strauss HW. Practical Nuclear Medicine. Philadelphia, PA: Saunders, 1992;71–120.
Verani MS. Tl-201 myocardial perfusion imaging. Curr Opin Radiol 1991;3:797–809.
SALVADORE BORGES-NETO
HISTORY
This is a 49-year-old woman who underwent complete thyroidectomy for papillary carcinoma of the thyroid. A metastasis to a left superior jugular node was found at surgery but not resected. An I-131 whole body scan was performed to evaluate for residual thyroid tissue and metastases after the patient developed hypothyroidism.

 FIGURE 10-3A I-131 total body scans in the anterior (left image) and posterior (right image) projections obtained at 48 hours after the oral administration of 5 mCi of I-131 sodium iodide. A prominent region of radiotracer accumulation is seen within the neck. The star pattern that is seen in the neck region is caused by septal penetration of the collimator by the high-energy photons (364 keV). Normal activity is present in the salivary glands, stomach, bladder, and bowel.
FIGURE 10-3A I-131 total body scans in the anterior (left image) and posterior (right image) projections obtained at 48 hours after the oral administration of 5 mCi of I-131 sodium iodide. A prominent region of radiotracer accumulation is seen within the neck. The star pattern that is seen in the neck region is caused by septal penetration of the collimator by the high-energy photons (364 keV). Normal activity is present in the salivary glands, stomach, bladder, and bowel.
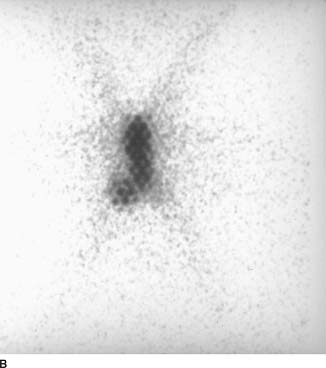
 FIGURE 10-3B Anterior magnification view of the neck. The region of radiotracer accumulation in the neck is actually seen to consist of two foci. The larger focus is in the midline. Another smaller focus is present along the right lower border of the larger focus. The very small photopenic regions within each focus of radiotracer accumulation are due to attenuation of activity by the lead collimator. The star pattern mentioned in Figure 10-4A is seen again.
FIGURE 10-3B Anterior magnification view of the neck. The region of radiotracer accumulation in the neck is actually seen to consist of two foci. The larger focus is in the midline. Another smaller focus is present along the right lower border of the larger focus. The very small photopenic regions within each focus of radiotracer accumulation are due to attenuation of activity by the lead collimator. The star pattern mentioned in Figure 10-4A is seen again.
 Solely residual thyroid tissue: The presence of residual thyroid tissue alone could produce the larger, mid-line focus of radiotracer accumulation but would not account for the smaller focus to the right of midline. Furthermore, it is known that residual metastatic disease was left at the time of surgery. Therefore, this diagnosis is incorrect.
Solely residual thyroid tissue: The presence of residual thyroid tissue alone could produce the larger, mid-line focus of radiotracer accumulation but would not account for the smaller focus to the right of midline. Furthermore, it is known that residual metastatic disease was left at the time of surgery. Therefore, this diagnosis is incorrect.
 Functioning thyroid metastatic disease alone: This diagnosis is incorrect because it would not account for the large midline focus, which is at the expected site of the thyroid gland. In addition, it is quite unusual to have no residual thyroid tissue remaining after attempted total thyroidectomy.
Functioning thyroid metastatic disease alone: This diagnosis is incorrect because it would not account for the large midline focus, which is at the expected site of the thyroid gland. In addition, it is quite unusual to have no residual thyroid tissue remaining after attempted total thyroidectomy.
 Residual thyroid tissue and functioning metastasis: This diagnosis would account for both foci of radio-tracer accumulation and is the most likely consideration.
Residual thyroid tissue and functioning metastasis: This diagnosis would account for both foci of radio-tracer accumulation and is the most likely consideration.
 Swallowed radioiodine: Radioiodine that is swallowed can often be seen in the esophagus. This artifact is prevented by having the patient ingest small amounts of food and fluids. However, the radiotracer activity would be expected to be seen only in the midline. This diagnosis is incorrect because it would not account for the small focus of radiotracer accumulation to the right of midline.
Swallowed radioiodine: Radioiodine that is swallowed can often be seen in the esophagus. This artifact is prevented by having the patient ingest small amounts of food and fluids. However, the radiotracer activity would be expected to be seen only in the midline. This diagnosis is incorrect because it would not account for the small focus of radiotracer accumulation to the right of midline.
 Residual thyroid tissue in the neck with metastatic spread to the abdomen and pelvis: The radiotracer activity in the abdomen and pelvis in the case illustrated is that which is normally seen on I-131 total body scans, due to excretion into the stomach, colon, and bladder. This radiotracer activity does not represent metastatic disease.
Residual thyroid tissue in the neck with metastatic spread to the abdomen and pelvis: The radiotracer activity in the abdomen and pelvis in the case illustrated is that which is normally seen on I-131 total body scans, due to excretion into the stomach, colon, and bladder. This radiotracer activity does not represent metastatic disease.
DIAGNOSIS
Residual functioning thyroid tissue and functioning metastasis
KEY FACTS
Clinical
 Thyroid cancers are rarely of a single cell type and are designated by the predominant histologic type.
Thyroid cancers are rarely of a single cell type and are designated by the predominant histologic type.
 Three types of carcinoma: (1) well-differentiated papillary carcinoma, (2) follicular carcinoma, and (3) mixed papillary-follicular carcinoma, comprise about 75% of all primary thyroid malignancies.
Three types of carcinoma: (1) well-differentiated papillary carcinoma, (2) follicular carcinoma, and (3) mixed papillary-follicular carcinoma, comprise about 75% of all primary thyroid malignancies.
 Anaplastic and poorly differentiated thyroid carcinomas comprise 20% of all thyroid malignancies and occur primarily in elderly patients.
Anaplastic and poorly differentiated thyroid carcinomas comprise 20% of all thyroid malignancies and occur primarily in elderly patients.
 Medullary thyroid carcinoma constitutes approximately 5% of all primary thyroid cancers and can be associated with other endocrine lesions such as pheochromocy-toma as part of a multiple endocrine neoplasia (MEN) syndrome.
Medullary thyroid carcinoma constitutes approximately 5% of all primary thyroid cancers and can be associated with other endocrine lesions such as pheochromocy-toma as part of a multiple endocrine neoplasia (MEN) syndrome.
 In well-differentiated thyroid cancers, the overall prognosis is good, with a 5-year survival rate of >95% in properly treated patients.
In well-differentiated thyroid cancers, the overall prognosis is good, with a 5-year survival rate of >95% in properly treated patients.
 Well-differentiated papillary carcinoma tends to metas-tasize to local lymph nodes in the neck, whereas fol-licular carcinoma tends to spread hematogenously, producing metastases to the lungs and bones.
Well-differentiated papillary carcinoma tends to metas-tasize to local lymph nodes in the neck, whereas fol-licular carcinoma tends to spread hematogenously, producing metastases to the lungs and bones.
 When evaluating patients with well-differentiated thyroid cancer using I-131 sodium iodide, it is important to stop thyroid replacement therapy and allow thyroid-stimulating hormone (TSH) levels to elevate before administration of radiotracer for a total body scan. The resultant high TSH levels stimulate any remaining thyroid tissue or functioning metastases and increase detection of these sites on imaging studies.
When evaluating patients with well-differentiated thyroid cancer using I-131 sodium iodide, it is important to stop thyroid replacement therapy and allow thyroid-stimulating hormone (TSH) levels to elevate before administration of radiotracer for a total body scan. The resultant high TSH levels stimulate any remaining thyroid tissue or functioning metastases and increase detection of these sites on imaging studies.
 Elevation of endogenous TSH takes approximately 4 to 6 weeks to occur after a total thyroidectomy or after cessation of exogenous thyroxin.
Elevation of endogenous TSH takes approximately 4 to 6 weeks to occur after a total thyroidectomy or after cessation of exogenous thyroxin.
Radiologic
 Normal radiotracer accumulation of I-131 occurs within the salivary glands, stomach, bladder, and bowel.
Normal radiotracer accumulation of I-131 occurs within the salivary glands, stomach, bladder, and bowel.
 To optimize the tumor-to-background ratio, imaging should be performed 48 or 72 hours after administration of I-131.
To optimize the tumor-to-background ratio, imaging should be performed 48 or 72 hours after administration of I-131.
 The usual dose of I-131 administered for whole body imaging for the detection of metastatic differentiated thyroid cancer is 5 to 10 mCi.
The usual dose of I-131 administered for whole body imaging for the detection of metastatic differentiated thyroid cancer is 5 to 10 mCi.
 Tl-201 can be used to differentiate functioning metas-tases from well-differentiated thyroid carcinoma. An advantage of Tl-201 over I-131 is that the patients do not need to be in a hypothyroid state for the Tl-201 to detect metastatic foci.
Tl-201 can be used to differentiate functioning metas-tases from well-differentiated thyroid carcinoma. An advantage of Tl-201 over I-131 is that the patients do not need to be in a hypothyroid state for the Tl-201 to detect metastatic foci.
 Medullary and anaplastic thyroid cancers rarely, if ever, concentrate I-131.
Medullary and anaplastic thyroid cancers rarely, if ever, concentrate I-131.
 Significant residual thyroid tissue can produce a star pattern that is caused by septal penetration of the col-limator by the high-energy photons. The star pattern is less likely to result from accumulation in thyroid cancer because the accumulation in functioning thyroid cancer is usually less than in normal thyroid gland.
Significant residual thyroid tissue can produce a star pattern that is caused by septal penetration of the col-limator by the high-energy photons. The star pattern is less likely to result from accumulation in thyroid cancer because the accumulation in functioning thyroid cancer is usually less than in normal thyroid gland.
SUGGESTED READING
Hurley JR, Becker DV. Treatment of thyroid carcinoma with radioiodine. In A Gottschalk, PB Hoffer, EJ Potchen (eds), Diagnostic Nuclear Medicine. Baltimore, MD: Williams & Wilkins, 1988;792–814.
KüÇük NO, Külak HA, Aras G. Clinical importance of technetium-99m-methoxyisobutylisonitrile (MIBI) scintigraphy in differentiated thyroid carcinoma patients with elevated thyroglobulin levels and negative I-131 scanning results. Ann Nucl Med 2006;20:393–397.
Lind P, Kohlfurst S. Respective roles of thyroglobulin, radioiodine imaging, and positron emission tomography in the assessment of thyroid cancer. Semin Nucl Med 2006;36:194–205.
Mettler FA, Guiberteau MJ. Essentials of Nuclear Medicine Imaging. Philadelphia, PA: Saunders, 1991;87–93.
ROBERT H.
WILKINSON, JR.
HISTORY
A 77-year-old Englishman with progressive swelling and deformity of his legs and right arm has noted an increasing frequency of headaches and an increase in hat size over the past several years. Laboratory studies include an elevated alkaline phosphatase level and normal acid phosphatase and prostate-specific antigen (PSA) values.

 FIGURE 10-4A Anterior (left) and posterior (right) images of a whole body bone scan obtained after the intravenous administration of Tc-99m MDP. Markedly abnormal regions of increased radiotracer bone uptake are noted within the axial and appendicular skeleton.
FIGURE 10-4A Anterior (left) and posterior (right) images of a whole body bone scan obtained after the intravenous administration of Tc-99m MDP. Markedly abnormal regions of increased radiotracer bone uptake are noted within the axial and appendicular skeleton.

 FIGURE 10-4B Anteroposterior radiograph of the pelvis revealing bony expansion, sclerosis, and cortical thickening.
FIGURE 10-4B Anteroposterior radiograph of the pelvis revealing bony expansion, sclerosis, and cortical thickening.
 Paget’s disease of bone: The pattern seen on the radionuclide bone scan is that of regions of markedly increased bone tracer accumulation with an expanded appearance to the entire bone. These features are typical of Paget’s disease, the most likely diagnosis.
Paget’s disease of bone: The pattern seen on the radionuclide bone scan is that of regions of markedly increased bone tracer accumulation with an expanded appearance to the entire bone. These features are typical of Paget’s disease, the most likely diagnosis.
 Metastases: Metastases can simulate lesions of Paget’s bone disease. The advanced degree of tracer accumulation and expanded bone appearance seen in this case, however, are atypical even for advanced prostate, breast, or lung carcinoma. This diagnosis is an unlikely consideration.
Metastases: Metastases can simulate lesions of Paget’s bone disease. The advanced degree of tracer accumulation and expanded bone appearance seen in this case, however, are atypical even for advanced prostate, breast, or lung carcinoma. This diagnosis is an unlikely consideration.
 Fractures: The expanded bone and diffuse tracer accumulation make fractures unlikely considerations.
Fractures: The expanded bone and diffuse tracer accumulation make fractures unlikely considerations.
 Osteomyelitis: Regions of intense tracer accumulation can be seen in osteomyelitis, but the clinical setting, the diffuse nature of the abnormalities, and the expansile changes seen on the radiograph make this diagnosis highly unlikely.
Osteomyelitis: Regions of intense tracer accumulation can be seen in osteomyelitis, but the clinical setting, the diffuse nature of the abnormalities, and the expansile changes seen on the radiograph make this diagnosis highly unlikely.
 Fibrous dysplasia: Polyostotic fibrous dysplasia can produce increased tracer accumulation in multiple bones, as is seen in this case. However, the history of progressive bony expansion late in life and the radio-graphic findings make this diagnosis unlikely.
Fibrous dysplasia: Polyostotic fibrous dysplasia can produce increased tracer accumulation in multiple bones, as is seen in this case. However, the history of progressive bony expansion late in life and the radio-graphic findings make this diagnosis unlikely.
DIAGNOSIS
Paget’s disease of bone
KEY FACTS
Clinical
 Paget’s disease is most commonly encountered in Eastern and Western Europe (with the exception of Scandinavia), with a prevalence of 3.5% to 4.5% and with a 3 to 2 male-to-female predominance.
Paget’s disease is most commonly encountered in Eastern and Western Europe (with the exception of Scandinavia), with a prevalence of 3.5% to 4.5% and with a 3 to 2 male-to-female predominance.
 The etiology of Paget’s disease is not known definitively. Slow virus inoculation early in life is one hypothesis that has been strongly considered.
The etiology of Paget’s disease is not known definitively. Slow virus inoculation early in life is one hypothesis that has been strongly considered.
 Progression of Paget’s disease can be classified into three stages: (1) bone resorption, (2) mixed bone resorp-tion and deformation, and (3) decline in resorption accompanied by a decrease in irregularity and fibrosis.
Progression of Paget’s disease can be classified into three stages: (1) bone resorption, (2) mixed bone resorp-tion and deformation, and (3) decline in resorption accompanied by a decrease in irregularity and fibrosis.
 The prevalence of fractures in Paget’s disease is reported to be 8% to 18%, based on retrospective series.
The prevalence of fractures in Paget’s disease is reported to be 8% to 18%, based on retrospective series.
 Sarcomatous degeneration of pagetoid bone can occur and can be solitary or multicentric.
Sarcomatous degeneration of pagetoid bone can occur and can be solitary or multicentric.
 Elevated cardiac output is seen in some patients with Paget’s disease due to the increased vascularity of acute pagetoid bone.
Elevated cardiac output is seen in some patients with Paget’s disease due to the increased vascularity of acute pagetoid bone.
Radiologic
 On radiographs, vertebrae appear enlarged and deformed; the scapulae and pelvic bones appear expanded and thickened; the skull enlarges with basi-lar flattening and cortical thickening; and the long bones bow and develop cortical thickening.
On radiographs, vertebrae appear enlarged and deformed; the scapulae and pelvic bones appear expanded and thickened; the skull enlarges with basi-lar flattening and cortical thickening; and the long bones bow and develop cortical thickening.
 The degree of radiotracer accumulation in pagetoid bone is variable.
The degree of radiotracer accumulation in pagetoid bone is variable.
 The radionuclide study is reported to be more sensitive than radiographs: 5% to 20% of patients have abnormal bone scans and normal radiographs, compared to 1% with abnormal radiographs and normal radionuclide bone scan.
The radionuclide study is reported to be more sensitive than radiographs: 5% to 20% of patients have abnormal bone scans and normal radiographs, compared to 1% with abnormal radiographs and normal radionuclide bone scan.
 Bone scan findings do not correlate well with the severity of bone pain in Paget’s disease.
Bone scan findings do not correlate well with the severity of bone pain in Paget’s disease.
 Reduced accumulation of In-111-labeled leukocytes and of Tc-99m sulfur colloid has been reported to occur in Paget’s disease.
Reduced accumulation of In-111-labeled leukocytes and of Tc-99m sulfur colloid has been reported to occur in Paget’s disease.
 Photopenic regions can be seen in pagetoid bone in instances of sarcomatous degeneration, most likely due to proliferation of nonosteoblastic tissue.
Photopenic regions can be seen in pagetoid bone in instances of sarcomatous degeneration, most likely due to proliferation of nonosteoblastic tissue.
 A photopenic area in a bone scan that occurs in a radio-graphically evident region of Paget’s disease can represent either early disease or sarcomatous degeneration.
A photopenic area in a bone scan that occurs in a radio-graphically evident region of Paget’s disease can represent either early disease or sarcomatous degeneration.
 Ga-67 may be useful for sarcoma detection. In one small study, slightly more than half of Paget’s disease patients with sarcomas and a focal photopenic area on bone scan were found to have increased Ga-67 accumulation at the site of the sarcoma. Another small series found the Ga-67 scan to be less sensitive.
Ga-67 may be useful for sarcoma detection. In one small study, slightly more than half of Paget’s disease patients with sarcomas and a focal photopenic area on bone scan were found to have increased Ga-67 accumulation at the site of the sarcoma. Another small series found the Ga-67 scan to be less sensitive.
SUGGESTED READING
Altman RD. Paget’s disease of bone. In FL Coe, MJ Favus (eds), Disorders of Bone and Mineral Metabolism. New York, NY: Raven, 1992;1027–1061.
Boudreau RJ, Lisbona R, Hadjipavtou A. Observations on serial radionuclide blood flow studies in Paget’s disease. J Nucl Med 1983;24:880–885.
Hain SF, Fogelman I. Nuclear medicine studies in metabolic bone disease. Semin Musculoskelet Radiol 2002;6:323–329.
Ryan PJ. Orthopaedic manifestations of systemic disease. Semin Nucl Med 1998;28:124–131.
Smith J, Bitet JF, Yeh SJ. Bone sarcomas in Paget’s disease: a study of 85 patients. Radiology 1984;152:583–590.
ROBERT H.
WILKINSON, Jr.
HISTORY
The bone scans of three patients are presented. Patient A is a 67-year-old man with an elevated prostate-specific antigen (PSA) value of 86 ng/mL and biopsy-proven prostate carcinoma. Patient B is a 69-year-old man with a history of prostate carcinoma and a borderline normal PSA value of 6 ng/mL. Patient C is a 71-year-old woman with a history of stage IV breast carcinoma. A different diagnosis is possible in each of the cases.

 FIGURE 10-5A Patient A: Posterior image from a total body bone imaging study. Multiple foci of abnormally increased bone radiotracer accumulation are seen in the axial and proximal appen-dicular skeleton.
FIGURE 10-5A Patient A: Posterior image from a total body bone imaging study. Multiple foci of abnormally increased bone radiotracer accumulation are seen in the axial and proximal appen-dicular skeleton.

 FIGURE 10-5B Patient B: Right posterior oblique view of the chest shows foci of increased radiotracer accumulation in adjacent ribs in a “string-of-pearls” pattern.
FIGURE 10-5B Patient B: Right posterior oblique view of the chest shows foci of increased radiotracer accumulation in adjacent ribs in a “string-of-pearls” pattern.
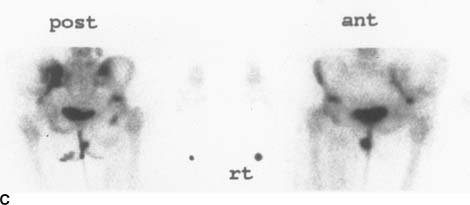
 FIGURE 10-5C Patient C: Anterior and posterior pelvic images. A mixed pattern of abnormal foci of abnormally increased and decreased radiotracer accumulation is seen in the left ilium.
FIGURE 10-5C Patient C: Anterior and posterior pelvic images. A mixed pattern of abnormal foci of abnormally increased and decreased radiotracer accumulation is seen in the left ilium.
 Metastases: Bone metastases can appear on bone scans as any or all of the following: multiple foci of increased radiotracer accumulation (Figure 10-7A), increased or decreased radiotracer accumulation (Figure 10-7C), and normal bone radiotracer accumulation. The pattern and location of the abnormalities in Figures 10-7A and 10-7C make bone metastases the most likely consideration.
Metastases: Bone metastases can appear on bone scans as any or all of the following: multiple foci of increased radiotracer accumulation (Figure 10-7A), increased or decreased radiotracer accumulation (Figure 10-7C), and normal bone radiotracer accumulation. The pattern and location of the abnormalities in Figures 10-7A and 10-7C make bone metastases the most likely consideration.
 Pathologic fractures: Pathologic fractures can be solitary or multiple and usually occur in metastatic bone lesions that are subject to stress or trauma. Bone metastases in weight-bearing regions are particularly susceptible to fracture.
Pathologic fractures: Pathologic fractures can be solitary or multiple and usually occur in metastatic bone lesions that are subject to stress or trauma. Bone metastases in weight-bearing regions are particularly susceptible to fracture.
 Multiple benign fractures: The pattern, location, and clinical history are important in distinguishing benign fractures from metastatic disease. Some patterns of fractures (e.g., the string-of-pearls appearance in Figure 10-7B) are typical of benign fractures. This is the diagnosis in patient B.
Multiple benign fractures: The pattern, location, and clinical history are important in distinguishing benign fractures from metastatic disease. Some patterns of fractures (e.g., the string-of-pearls appearance in Figure 10-7B) are typical of benign fractures. This is the diagnosis in patient B.
 Degenerative joint disease/arthritides: These processes occur at joints and can be difficult to distinguish from metastases. Concomitant benign arthropathic disease can occur in patients with metastatic disease, but the pattern of nonarticular bone abnormalities in all three patients shown above makes benign arthropathic disease alone unlikely.
Degenerative joint disease/arthritides: These processes occur at joints and can be difficult to distinguish from metastases. Concomitant benign arthropathic disease can occur in patients with metastatic disease, but the pattern of nonarticular bone abnormalities in all three patients shown above makes benign arthropathic disease alone unlikely.
DIAGNOSIS
Patients A and C: multiple bone metastases; Patient B: benign rib fractures
KEY FACTS
Clinical
 The likelihood of bone metastases depends on the primary tumor (e.g., most primary bone tumors rarely metastasize) and the stage of disease.
The likelihood of bone metastases depends on the primary tumor (e.g., most primary bone tumors rarely metastasize) and the stage of disease.
 The lifetime risk of developing breast cancer in American women is reported to be approximately 11%, and over one-half of breast cancers occur in women after the age of 65 years. In autopsy series of women with metastatic breast carcinoma, the frequency of bone metastases has been reported to be between 44% and 71%.
The lifetime risk of developing breast cancer in American women is reported to be approximately 11%, and over one-half of breast cancers occur in women after the age of 65 years. In autopsy series of women with metastatic breast carcinoma, the frequency of bone metastases has been reported to be between 44% and 71%.
 The digital rectal examination and serum PSA test are currently the recommended screening procedures for prostate carcinoma. Approximately one-third of men over the age of 50 years harbor foci of prostatic carcinoma without clinical evidence of disease.
The digital rectal examination and serum PSA test are currently the recommended screening procedures for prostate carcinoma. Approximately one-third of men over the age of 50 years harbor foci of prostatic carcinoma without clinical evidence of disease.
 Approximately 80% of patients with detectable prostate carcinoma and distant metastases are found to have bone metastases.
Approximately 80% of patients with detectable prostate carcinoma and distant metastases are found to have bone metastases.
Radiologic
 The majority of metastatic bone tumors appear as focal regions of increased radiotracer accumulation on radionuclide bone scan. However, photopenic foci can be seen in malignancies such as breast, lung, renal, and anaplastic carcinomas; neuroblastoma; and multiple myeloma.
The majority of metastatic bone tumors appear as focal regions of increased radiotracer accumulation on radionuclide bone scan. However, photopenic foci can be seen in malignancies such as breast, lung, renal, and anaplastic carcinomas; neuroblastoma; and multiple myeloma.
 Soft tissue neoplasms can invade bone and produce increased radiotracer uptake or a photopenic focus, which usually has a rim of increased radiotracer accumulation.
Soft tissue neoplasms can invade bone and produce increased radiotracer uptake or a photopenic focus, which usually has a rim of increased radiotracer accumulation.
 Benign bone conditions that can appear photopenic include bone infarction, bone resection, very early osteomyelitis, radiation-induced bone changes, and histiocytosis X.
Benign bone conditions that can appear photopenic include bone infarction, bone resection, very early osteomyelitis, radiation-induced bone changes, and histiocytosis X.
 Skeletal involvement from multiple myeloma, plasma-cytoma, neuroblastoma, and eosinophilic granuloma can produce normal, increased, or decreased radio-tracer accumulation.
Skeletal involvement from multiple myeloma, plasma-cytoma, neuroblastoma, and eosinophilic granuloma can produce normal, increased, or decreased radio-tracer accumulation.
 Particular care must be taken in evaluating the radio-nuclide bone imaging study of a patient with bone metastases during the first 4 to 6 months after starting chemotherapy, because a disparity between the clini-cal/radiologic status and findings on radionuclide bone scan can be seen. These patients can improve clinically and have a decrease in the number and size of bone lesions on radiographs but no change or apparent worsening of lesions (the so-called flare phenomenon) on the radionuclide bone imaging study. This pattern change presumably reflects healing of lesions and is most commonly reported in bone metastases from a primary breast or prostate tumor. Following further healing of bone lesions after this initial period, the radionuclide bone study reflects the clinical and radiologic status more accurately.
Particular care must be taken in evaluating the radio-nuclide bone imaging study of a patient with bone metastases during the first 4 to 6 months after starting chemotherapy, because a disparity between the clini-cal/radiologic status and findings on radionuclide bone scan can be seen. These patients can improve clinically and have a decrease in the number and size of bone lesions on radiographs but no change or apparent worsening of lesions (the so-called flare phenomenon) on the radionuclide bone imaging study. This pattern change presumably reflects healing of lesions and is most commonly reported in bone metastases from a primary breast or prostate tumor. Following further healing of bone lesions after this initial period, the radionuclide bone study reflects the clinical and radiologic status more accurately.
 Patients with a PSA value of <10 ng/mL during their initial evaluation for prostate carcinoma have a very low likelihood of having a positive radionuclide bone imaging study for metastases.
Patients with a PSA value of <10 ng/mL during their initial evaluation for prostate carcinoma have a very low likelihood of having a positive radionuclide bone imaging study for metastases.
 The likelihood of a solitary bone scan lesion being a metastasis is reported to range from 10% (in adults) to 60% (in children).
The likelihood of a solitary bone scan lesion being a metastasis is reported to range from 10% (in adults) to 60% (in children).
 In the presence of a known primary malignancy, approximately 10% to 20% of solitary rib lesions on bone scans are metastases. On the other hand, focal rib lesions having a string-of-pearls pattern are highly likely to be benign rib fractures.
In the presence of a known primary malignancy, approximately 10% to 20% of solitary rib lesions on bone scans are metastases. On the other hand, focal rib lesions having a string-of-pearls pattern are highly likely to be benign rib fractures.
 Correlation with radiographs or other imaging studies is often useful to confirm the presence of bone metas-tases in patients with bone scan abnormalities. In the presence of an abnormal radionuclide bone scan, a normal radiograph actually makes a bone metastasis a likely consideration by excluding other possible causes.
Correlation with radiographs or other imaging studies is often useful to confirm the presence of bone metas-tases in patients with bone scan abnormalities. In the presence of an abnormal radionuclide bone scan, a normal radiograph actually makes a bone metastasis a likely consideration by excluding other possible causes.
SUGGESTED READING
Beheshti M, Langsteger W, Fogelman I. Prostate cancer: Role of SPECT and PET in imaging bone metastases. Semin Nucl Med 2009;39:396–407.
Ben-Haim S, Israel O. Breast cancer: Role of SPECT and PET in imaging bone metastases. Semin Nucl Med 2009;39:408–415.
Chua S, Gnanasegaran G, Cook GJ. Miscellaneous cancers (lung, thyroid, renal cancer, myeloma, and neuroendocrine tumors): role of SPECT and PET in imaging bone metastases. Semin Nucl Med 2009;39:416–430.
Hanks GE, Myers CE, Scardino PT. Cancer of the prostate. In VT DeVita Jr, S Hellman, SA Rosenberg (eds), Cancer—Principles and Practice of Oncology (4th ed). Philadelphia, PA: Lippincott, 1993;1073–1113.
Janicek MJ, Hayes DF, Kaplan WD. Healing flare in skeletal metastases from breast cancer. Radiology 1994;192:201–204.
O’Connor MK, Brown ML, Hung JC, Hayostek RJ. The art of bone scintigra-phy—technical aspects. J Nucl Med 1991;32:2332–2341.
R. EDWARD
COLEMAN
HISTORY
A 75-year-old man being treated for hypercalcemia.
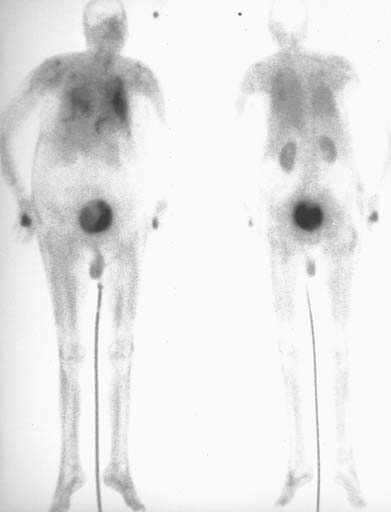
 FIGURE 10-6 Anterior (left) and posterior (right) images from a radionuclide bone scan obtained 2 hours after the IV administration of 20 mCi of Tc-99m MDP. Abnormal accumulation of radiotracer is present in the lungs and in the stomach as a result of the hypercalcemia. However, no radiotracer accumulation is seen in the bones. Normal renal and bladder radiotracer accumulation are seen, as well as a small focus of activity at the injection site in the right hand.
FIGURE 10-6 Anterior (left) and posterior (right) images from a radionuclide bone scan obtained 2 hours after the IV administration of 20 mCi of Tc-99m MDP. Abnormal accumulation of radiotracer is present in the lungs and in the stomach as a result of the hypercalcemia. However, no radiotracer accumulation is seen in the bones. Normal renal and bladder radiotracer accumulation are seen, as well as a small focus of activity at the injection site in the right hand.
 Administration of incorrect radiopharmaceutical: This diagnosis is unlikely because no radiopharmaceu-tical has the pattern of distribution seen in this patient.
Administration of incorrect radiopharmaceutical: This diagnosis is unlikely because no radiopharmaceu-tical has the pattern of distribution seen in this patient.
 Presence of excess aluminum ion: Contamination of Tc-99m methylene diphosphonate (MDP) with aluminum ion from the eluate or the presence of high plasma aluminum levels in patients taking aluminum hydroxide antacids can alter biodistribution of the radiophar-maceutical agent. However, these conditions cause increased uptake in the liver and kidneys and not the lung accumulation, seen in the case illustrated.
Presence of excess aluminum ion: Contamination of Tc-99m methylene diphosphonate (MDP) with aluminum ion from the eluate or the presence of high plasma aluminum levels in patients taking aluminum hydroxide antacids can alter biodistribution of the radiophar-maceutical agent. However, these conditions cause increased uptake in the liver and kidneys and not the lung accumulation, seen in the case illustrated.
 Effect of therapy for hypercalcemia: The patient shown above was receiving intravenously administered etidronate for treatment of hypercalcemia. Etidronate (hydroxyethylidene diphosphonic acid [HEDP]) inhibits the formation, growth, and dissolution of hydroxyap-atite crystals. This agent can cause the lack of radio-pharmaceutical accumulation within bones, as shown above.
Effect of therapy for hypercalcemia: The patient shown above was receiving intravenously administered etidronate for treatment of hypercalcemia. Etidronate (hydroxyethylidene diphosphonic acid [HEDP]) inhibits the formation, growth, and dissolution of hydroxyap-atite crystals. This agent can cause the lack of radio-pharmaceutical accumulation within bones, as shown above.
 Premature imaging: Images obtained immediately after administration of Tc-99m MDP will typically show blood pool activity, prominent soft tissue activity, and some bone accumulation. However, accumulation in the lungs would not be expected, making this diagnosis unlikely.
Premature imaging: Images obtained immediately after administration of Tc-99m MDP will typically show blood pool activity, prominent soft tissue activity, and some bone accumulation. However, accumulation in the lungs would not be expected, making this diagnosis unlikely.
 Iron overload: This diagnosis might be considered because in iron overload, such as in hemochromatosis or following multiple blood transfusions, the accumulation of Tc-99m MDP into bone is diminished and renal excretion is increased. However, pulmonary deposition of the radiotracer would not be expected.
Iron overload: This diagnosis might be considered because in iron overload, such as in hemochromatosis or following multiple blood transfusions, the accumulation of Tc-99m MDP into bone is diminished and renal excretion is increased. However, pulmonary deposition of the radiotracer would not be expected.
DIAGNOSIS
Hypercalcemia with etidronate therapy
KEY FACTS
Clinical
 Hypercalcemia can occur secondary to a number of entities, including hyperparathyroidism, metastatic skeletal disease, hyperthyroidism, and sarcoidosis.
Hypercalcemia can occur secondary to a number of entities, including hyperparathyroidism, metastatic skeletal disease, hyperthyroidism, and sarcoidosis.
 Biphosphonates such as etidronate and pamidronate are used to treat the hypercalcemia of malignancy because of their effect on bone turnover. The biphos-phonates interact with the hydroxyapatite crystal, inhibiting bone resorption, and may impair osteoclast function. These agents are also used to treat Paget’s disease and heterotopic ossification and may have a role in treating osteoporosis.
Biphosphonates such as etidronate and pamidronate are used to treat the hypercalcemia of malignancy because of their effect on bone turnover. The biphos-phonates interact with the hydroxyapatite crystal, inhibiting bone resorption, and may impair osteoclast function. These agents are also used to treat Paget’s disease and heterotopic ossification and may have a role in treating osteoporosis.
 Radionuclide bone scans in patients with hypercalcemia and elevated calcium phosphorus products frequently show abnormal localization of the radiopharmaceutical in the lungs, stomach, and kidneys, reflecting the acid-base changes that occur in these tissues. Furthermore, these are the sites of metastatic calcification that can occur in these patients.
Radionuclide bone scans in patients with hypercalcemia and elevated calcium phosphorus products frequently show abnormal localization of the radiopharmaceutical in the lungs, stomach, and kidneys, reflecting the acid-base changes that occur in these tissues. Furthermore, these are the sites of metastatic calcification that can occur in these patients.
 The effect of biphosphonates on Tc-99m MDP bone scans is variable. The biphosphonate used and the method of administration (oral or intravenous) may make a difference in the effect on the bone scan. Some studies report difficulty in interpretation of radionu-clide bone scans in patients undergoing biphosphonate therapy, whereas other studies have shown no effect on the sensitivity of the bone scan.
The effect of biphosphonates on Tc-99m MDP bone scans is variable. The biphosphonate used and the method of administration (oral or intravenous) may make a difference in the effect on the bone scan. Some studies report difficulty in interpretation of radionu-clide bone scans in patients undergoing biphosphonate therapy, whereas other studies have shown no effect on the sensitivity of the bone scan.
Radiologic
 A Tc-99m MDP bone scan that shows poor bone uptake and prominent soft tissue accumulation usually results from a radiopharmaceutical preparation problem, with excess Tc-99m pertechnetate in the preparation. The excess pertechnetate is manifested by radiotracer accumulation in the thyroid and stomach.
A Tc-99m MDP bone scan that shows poor bone uptake and prominent soft tissue accumulation usually results from a radiopharmaceutical preparation problem, with excess Tc-99m pertechnetate in the preparation. The excess pertechnetate is manifested by radiotracer accumulation in the thyroid and stomach.
 The clue to the diagnosis in the patient shown above is accumulation of the Tc-99m MDP in the lungs, which occurs with hypercalcemia. In a patient with accumulation of Tc-99m MDP in the lungs, associated bone scan findings should be considered as possibly related to hypercalcemia or its treatment.
The clue to the diagnosis in the patient shown above is accumulation of the Tc-99m MDP in the lungs, which occurs with hypercalcemia. In a patient with accumulation of Tc-99m MDP in the lungs, associated bone scan findings should be considered as possibly related to hypercalcemia or its treatment.
 Radionuclide bone scans usually provide diagnostic information in patients receiving biphosphonates, but as noted above, this agent can affect the scan. The effect of this therapy needs to be taken into account when interpreting the images.
Radionuclide bone scans usually provide diagnostic information in patients receiving biphosphonates, but as noted above, this agent can affect the scan. The effect of this therapy needs to be taken into account when interpreting the images.
SUGGESTED READING
Chong WK, Cunningham DA. Case report: intravenous etidronate as a cause of poor uptake on bone scanning, with a review of the literature. Clin Radiol 1991;44:268–270.
Lam MG, de Klerk JM, van Rijk PP, Zonnenberg BA. Bone seeking radio-pharmaceuticals for palliation of pain in cancer patients with osseous metastases. Anticancer Agents Med Chem 2007;7:381–397.
Paes FM, Serafini AN. Systemic metabolic radiopharmaceutical therapy in the treatment of metastatic bone pain. Semin Nucl Med 2010;40:89–104.
Pecherstorfer M, Schilling T, Janisch S, et al. Effect of clodronate treatment on bone scintigraphy in metastatic breast cancer. J Nucl Med 1993;34:1039–1044.
Sahni M, Guenther HL, Fleisch H, et al. Biphosphonates act on rate of bone resorption through mediation of osteoblasts. J Clin Invest 1993;91:2004–2011.
SARA M. O’HARA
HISTORY
A 6-week-old girl presents with jaundice. Her total bilirubin is 19.8 mg/dL, and conjugated bilirubin is 7.8 mg/dL.

 FIGURE 10-7A Anterior images of a diisopropyliminodiace-tic acid scan obtained immediately after injection. Good extraction of the radiopharmaceutical by the hepatocytes is seen, with prompt clearance of the blood pool. Homogenous radiotracer activity is present throughout the liver. Tracer activity is identified in both kidneys and the bladder. However, the central bile ducts, GI tract, and gallbladder have not accumulated the radiotracer. This pattern persisted on 24-hour delayed films (not shown).
FIGURE 10-7A Anterior images of a diisopropyliminodiace-tic acid scan obtained immediately after injection. Good extraction of the radiopharmaceutical by the hepatocytes is seen, with prompt clearance of the blood pool. Homogenous radiotracer activity is present throughout the liver. Tracer activity is identified in both kidneys and the bladder. However, the central bile ducts, GI tract, and gallbladder have not accumulated the radiotracer. This pattern persisted on 24-hour delayed films (not shown).

 FIGURE 10-7B Follow-up study 1 month later. In the interim since the previous study, the patient has undergone a Kasai procedure (portoenterostomy). This is an anterior image obtained 3.5 hours after injection. Radiopharmaceutical is again distributed homogeneously throughout the liver parenchyma. GI activity is now identified in the midabdomen, partially superimposed over the lower pole of the right kidney.
FIGURE 10-7B Follow-up study 1 month later. In the interim since the previous study, the patient has undergone a Kasai procedure (portoenterostomy). This is an anterior image obtained 3.5 hours after injection. Radiopharmaceutical is again distributed homogeneously throughout the liver parenchyma. GI activity is now identified in the midabdomen, partially superimposed over the lower pole of the right kidney.
 Idiopathic neonatal hepatitis: Jaundice and bile stasis are features of idiopathic neonatal hepatitis, but the biliary system is patent (unlike the case illustrated). Hepatic uptake and blood pool clearance of radiotracer can be delayed in neonatal hepatitis, and the degree of delay reflects the severity of hepatocyte damage.
Idiopathic neonatal hepatitis: Jaundice and bile stasis are features of idiopathic neonatal hepatitis, but the biliary system is patent (unlike the case illustrated). Hepatic uptake and blood pool clearance of radiotracer can be delayed in neonatal hepatitis, and the degree of delay reflects the severity of hepatocyte damage.
 Choledochal cyst: The absence of visualization of the proximal ducts or an actual cyst makes this diagnosis unlikely.
Choledochal cyst: The absence of visualization of the proximal ducts or an actual cyst makes this diagnosis unlikely.
 Biliary atresia: This is the best diagnosis because good hepatocyte extraction of radiopharmaceutical is seen in the absence of visible intrahepatic bile ducts or gastrointestinal (GI) activity, even on 24-hour images.
Biliary atresia: This is the best diagnosis because good hepatocyte extraction of radiopharmaceutical is seen in the absence of visible intrahepatic bile ducts or gastrointestinal (GI) activity, even on 24-hour images.
 Bile plug syndrome: This rare condition results in conjugated hyperbilirubinemia due to obstruction of the common bile duct (CBD) by inspissated bile/secretions. Sepsis, hemolytic disorders, dehydration, total par-enteral nutrition, and cystic fibrosis are predisposing conditions. Careful ultrasound examination to exclude echogenic, nonshadowing bile plugs within the dilated biliary tree is necessary to distinguish this condition from biliary atresia.
Bile plug syndrome: This rare condition results in conjugated hyperbilirubinemia due to obstruction of the common bile duct (CBD) by inspissated bile/secretions. Sepsis, hemolytic disorders, dehydration, total par-enteral nutrition, and cystic fibrosis are predisposing conditions. Careful ultrasound examination to exclude echogenic, nonshadowing bile plugs within the dilated biliary tree is necessary to distinguish this condition from biliary atresia.
 Arteriohepatic dysplasia (Alagille syndrome): This syndrome is characterized by typical dysmorphic facies, pulmonary artery stenosis, and hepatic ductular hypoplasia. Distinction from true biliary atresia can be difficult if the other components of the syndrome are not recognized.
Arteriohepatic dysplasia (Alagille syndrome): This syndrome is characterized by typical dysmorphic facies, pulmonary artery stenosis, and hepatic ductular hypoplasia. Distinction from true biliary atresia can be difficult if the other components of the syndrome are not recognized.
DIAGNOSIS
Biliary atresia
KEY FACTS
Clinical
 Hyperbilirubinemia is a common problem in neo-nates and infants. Unconjugated hyperbilirubinemia, in which <15% of the total bilirubin is conjugated (or “direct,” which is the nomenclature used on laboratory reports), is most often due to physiologic jaundice of the newborn, breast milk jaundice, or erythroblasto-sis fetalis. In conjugated hyperbilirubinemia, where at least 30% of the bilirubin is conjugated, a search for causes of obstructive jaundice is necessary. The most common causes of obstructive jaundice are included in the differential diagnosis listed above.
Hyperbilirubinemia is a common problem in neo-nates and infants. Unconjugated hyperbilirubinemia, in which <15% of the total bilirubin is conjugated (or “direct,” which is the nomenclature used on laboratory reports), is most often due to physiologic jaundice of the newborn, breast milk jaundice, or erythroblasto-sis fetalis. In conjugated hyperbilirubinemia, where at least 30% of the bilirubin is conjugated, a search for causes of obstructive jaundice is necessary. The most common causes of obstructive jaundice are included in the differential diagnosis listed above.
 Biliary atresia is the most common cause of extrahe-patic cholestasis in infants. The incidence ranges from 1 in 8,000 to 1 in 10,000 live births.
Biliary atresia is the most common cause of extrahe-patic cholestasis in infants. The incidence ranges from 1 in 8,000 to 1 in 10,000 live births.
 Distinction between idiopathic neonatal hepatitis, a nonsurgical disease, and biliary atresia, a surgical disease, is important within the first 3 months of life. The Kasai procedure (or portoenterostomy) is performed using a Roux-en-Y loop of intestine to bypass the hypo-plastic or absent biliary duct segments. The surgical success rate varies according to the patient age at the time of surgery. The procedure is 90% effective in patients <2 months of age, but only 17% effective in patients <3 months of age.
Distinction between idiopathic neonatal hepatitis, a nonsurgical disease, and biliary atresia, a surgical disease, is important within the first 3 months of life. The Kasai procedure (or portoenterostomy) is performed using a Roux-en-Y loop of intestine to bypass the hypo-plastic or absent biliary duct segments. The surgical success rate varies according to the patient age at the time of surgery. The procedure is 90% effective in patients <2 months of age, but only 17% effective in patients <3 months of age.
Radiologic
 Diisopropyliminodiacetic acid (DISIDA, disofenin) and mebrofenin (trimethyl-bromo-IDA) have the highest extraction rate by hepatocytes and shortest transit time of the IDA derivatives. Between 5% and 15% of the disofenin is excreted via the kidneys in normal subjects. Dynamic image acquisition immediately after radiopharmaceutical injection is helpful to determine hepatocyte extraction and hepatocyte function. Static images performed over the next 1 to 2 hours with delayed images taken up to 24 hours are generally required.
Diisopropyliminodiacetic acid (DISIDA, disofenin) and mebrofenin (trimethyl-bromo-IDA) have the highest extraction rate by hepatocytes and shortest transit time of the IDA derivatives. Between 5% and 15% of the disofenin is excreted via the kidneys in normal subjects. Dynamic image acquisition immediately after radiopharmaceutical injection is helpful to determine hepatocyte extraction and hepatocyte function. Static images performed over the next 1 to 2 hours with delayed images taken up to 24 hours are generally required.
 Pretreatment with oral phenobarbital (5 mg/kg/day for 5 days) is recommended to improve bile flow. With phe-nobarbital pretreatment, biliary scintigraphy is approximately 95% accurate in determining biliary patency in infants <3 months of age.
Pretreatment with oral phenobarbital (5 mg/kg/day for 5 days) is recommended to improve bile flow. With phe-nobarbital pretreatment, biliary scintigraphy is approximately 95% accurate in determining biliary patency in infants <3 months of age.
 Progressive hepatocyte damage and hepatic cirrhosis occur in the setting of untreated biliary atresia and in persistent neonatal hepatitis. The two diseases can be indistinguishable in patients >3months of age.
Progressive hepatocyte damage and hepatic cirrhosis occur in the setting of untreated biliary atresia and in persistent neonatal hepatitis. The two diseases can be indistinguishable in patients >3months of age.
SUGGESTED READING
Esmaili J, Izadyar S, Karegar I, Gholamrezanezhad A. Biliary atresia in infants with prolonged cholestatic jaundice: diagnostic accuracy of hepatobiliary scintigraphy. Abdom Imaging 2007;32:243–247.
Kasai M, Suzuke H, Ohashi E, et al. Technique and results of operative management of biliary atresia. World J Surg 1978;2:571–580.
Paltiel HJ. Imaging of neonatal cholestasis. Semin Ultrasound CT MR 1994;15:290-305.
Sevilla A, Howman-Giles R, Saleh H, et al. Hepatobiliary scintigraphy with SPECT in infancy. Clin Nucl Med 2007;32:16-23.
Treves ST, Jones AG, Markisz J. Liver and spleen. In ST Treves (ed), Pedia-tric Nuclear Medicine. New York, NY: Springer, 1995;466-495.
Wells RG, Sty JR. Radionuclide imaging of the liver, biliary system, and spleen. In JH Miller, MJ Gelfand (eds), Pediatric Nuclear Imaging. Philadelphia, PA: Saunders, 1994;103-156.
MICHAEL W.
HANSON
HISTORY
A 68-year-old man with a history of Crohn’s disease of the terminal ileum and colon presents with a 3-day history of nausea and right upper quadrant pain radiating posteriorly to the back. The pain is worsened by eating.

 FIGURE 10-8A Ultrasound shows small calculi in the gallbladder with mild thickening of the gallbladder wall. There is no pericholecystic fluid. The CBD (not shown) was normal in caliber.
FIGURE 10-8A Ultrasound shows small calculi in the gallbladder with mild thickening of the gallbladder wall. There is no pericholecystic fluid. The CBD (not shown) was normal in caliber.

 FIGURE 10-8B Hepatobiliary imaging study at 10 minutes. There is good hepatic extraction of Tc-99m disofenin with good visualization of the hepatic parenchyma. Radiotracer in the CBD and the duodenum indicates patency of the CBD.
FIGURE 10-8B Hepatobiliary imaging study at 10 minutes. There is good hepatic extraction of Tc-99m disofenin with good visualization of the hepatic parenchyma. Radiotracer in the CBD and the duodenum indicates patency of the CBD.
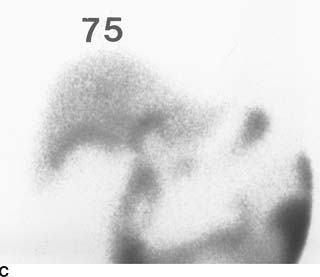
 FIGURE 10-8C Hepatobiliary imaging study at 75 minutes. Persistent radiotracer is seen in the CBD and within the small bowel. No radiotracer is present in the gallbladder, but a region of relatively increased radiotracer is seen within the liver parenchyma along the gallbladder fossa.
FIGURE 10-8C Hepatobiliary imaging study at 75 minutes. Persistent radiotracer is seen in the CBD and within the small bowel. No radiotracer is present in the gallbladder, but a region of relatively increased radiotracer is seen within the liver parenchyma along the gallbladder fossa.
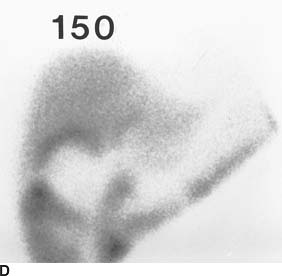
 FIGURE 10-8D Hepatobiliary imaging study at 150 minutes. The gallbladder is not visualized. A persistent region of prominent radiotracer accumulation exists in the liver parenchyma, consistent with pericholecystic hepatic uptake of Tc-99m disofenin.
FIGURE 10-8D Hepatobiliary imaging study at 150 minutes. The gallbladder is not visualized. A persistent region of prominent radiotracer accumulation exists in the liver parenchyma, consistent with pericholecystic hepatic uptake of Tc-99m disofenin.
 Acute pancreatitis: This process presents with abdominal pain and can be seen in patients with Crohn’s disease. An elevated serum amylase and/or lipase is usually present. Hepatobiliary imaging studies are normal unless pancreatitis is due to underlying hepatobili-ary disease. This diagnosis is therefore unlikely.
Acute pancreatitis: This process presents with abdominal pain and can be seen in patients with Crohn’s disease. An elevated serum amylase and/or lipase is usually present. Hepatobiliary imaging studies are normal unless pancreatitis is due to underlying hepatobili-ary disease. This diagnosis is therefore unlikely.
 Acalculous cholecystitis: Acute inflammation of the gallbladder can occur in the absence of cholelithiasis, most often as a complication of severe underlying illnesses (e.g., burns, trauma, sepsis, and following major surgery) associated with bile stasis. The benign clinical features and sonographic finding of gallstones make this diagnosis unlikely.
Acalculous cholecystitis: Acute inflammation of the gallbladder can occur in the absence of cholelithiasis, most often as a complication of severe underlying illnesses (e.g., burns, trauma, sepsis, and following major surgery) associated with bile stasis. The benign clinical features and sonographic finding of gallstones make this diagnosis unlikely.
 Common bile duct obstruction: Approximately 10% to 15% of patients with cholelithiasis will pass a gallstone into the CBD, where it can: (1) pass into the duodenum, (2) remain in the CBD without producing symptoms, or (3) obstruct the CBD. The presence of radiotracer in the CBD and the duodenum by 10 minutes essentially excludes CBD obstruction.
Common bile duct obstruction: Approximately 10% to 15% of patients with cholelithiasis will pass a gallstone into the CBD, where it can: (1) pass into the duodenum, (2) remain in the CBD without producing symptoms, or (3) obstruct the CBD. The presence of radiotracer in the CBD and the duodenum by 10 minutes essentially excludes CBD obstruction.
 Chronic cholecystitis: Patients with chronic cholecystitis frequently have gallstones and gallbladder wall thickening, and can have repeated bouts of biliary colic without cystic duct obstruction. The most frequent abnormal finding on scintigraphy is delayed visualization of the gallbladder beyond 1 hour, but imaging is often normal. Scintigraphy is generally an ineffective study in the evaluation of chronic cholecystitis, except to exclude a superimposed acute cystic duct obstruction. The majority of patients with chronic cholecystitis alone would be expected to have visualization of the gallbladder by 180 minutes, making this diagnosis unlikely in the case illustrated.
Chronic cholecystitis: Patients with chronic cholecystitis frequently have gallstones and gallbladder wall thickening, and can have repeated bouts of biliary colic without cystic duct obstruction. The most frequent abnormal finding on scintigraphy is delayed visualization of the gallbladder beyond 1 hour, but imaging is often normal. Scintigraphy is generally an ineffective study in the evaluation of chronic cholecystitis, except to exclude a superimposed acute cystic duct obstruction. The majority of patients with chronic cholecystitis alone would be expected to have visualization of the gallbladder by 180 minutes, making this diagnosis unlikely in the case illustrated.
 Acute cholecystitis: This entity typically has the presentation of right upper quadrant pain and tenderness with fever and leukocytosis. It often begins as an attack of biliary colic that progressively worsens and is associated with anorexia, nausea, and, commonly, emesis. With cystic duct obstruction, bile does not flow into or out of the gallbladder (as in the case presented above). The imaging findings in this case make this the most likely diagnosis.
Acute cholecystitis: This entity typically has the presentation of right upper quadrant pain and tenderness with fever and leukocytosis. It often begins as an attack of biliary colic that progressively worsens and is associated with anorexia, nausea, and, commonly, emesis. With cystic duct obstruction, bile does not flow into or out of the gallbladder (as in the case presented above). The imaging findings in this case make this the most likely diagnosis.
DIAGNOSIS
Cholelithiasis with acute cholecystitis
KEY FACTS
Clinical
 Patients with Crohn’s disease have an increased risk for developing cholelithiasis (due to altered bile salt absorption) as well as acute cholecystitis.
Patients with Crohn’s disease have an increased risk for developing cholelithiasis (due to altered bile salt absorption) as well as acute cholecystitis.
 Acute cholecystitis is most commonly caused by acute occlusion of the cystic duct by a gallstone.
Acute cholecystitis is most commonly caused by acute occlusion of the cystic duct by a gallstone.
 Seventy-five percent of patients with acute cholecystitis respond to medical therapy, of whom 25% have recurrent acute cholecystitis within 1 year. Another 25% of patients treated conservatively develop a major complication, such as empyema, hydrops, gangrene, emphy-sematous cholecystitis, perforation of the gallbladder, or gallstone ileus. Therefore, early surgical therapy is the preferred treatment.
Seventy-five percent of patients with acute cholecystitis respond to medical therapy, of whom 25% have recurrent acute cholecystitis within 1 year. Another 25% of patients treated conservatively develop a major complication, such as empyema, hydrops, gangrene, emphy-sematous cholecystitis, perforation of the gallbladder, or gallstone ileus. Therefore, early surgical therapy is the preferred treatment.
 As expected, patients with suspected empyema, emphy-sematous cholecystitis, or perforated gallbladder require more urgent surgical intervention than those with uncomplicated acute cholecystitis. It is important to search for evidence of these complications at the time of imaging.
As expected, patients with suspected empyema, emphy-sematous cholecystitis, or perforated gallbladder require more urgent surgical intervention than those with uncomplicated acute cholecystitis. It is important to search for evidence of these complications at the time of imaging.
 Perforation of the gallbladder has an estimated 30% mortality rate. These patients can have sudden transient relief of right upper quadrant pain as the distended gallbladder decompresses but then develop generalized signs of peritonitis.
Perforation of the gallbladder has an estimated 30% mortality rate. These patients can have sudden transient relief of right upper quadrant pain as the distended gallbladder decompresses but then develop generalized signs of peritonitis.
Radiologic
 The diagnosis of acute cholecystitis can be confidently excluded on the basis of a normal hepatobiliary imaging study (negative predictive value of 98%).
The diagnosis of acute cholecystitis can be confidently excluded on the basis of a normal hepatobiliary imaging study (negative predictive value of 98%).
 False-positive hepatobiliary scans can be seen in the following settings: (1) alcoholism, (2) total parenteral nutrition or prolonged fasting, (3) within 2 hours of eating, and (4) in severe intercurrent illnesses.
False-positive hepatobiliary scans can be seen in the following settings: (1) alcoholism, (2) total parenteral nutrition or prolonged fasting, (3) within 2 hours of eating, and (4) in severe intercurrent illnesses.
 Radiotracer in the duodenum or pericholecystic hepatic uptake of radiotracer (the “rim sign”) can be mistaken for gallbladder uptake, resulting in a false-negative interpretation. The finding of pericholecystic hepatic uptake of radiotracer is important to recognize. It is present in 57% of patients with gangrenous cholecystitis and 31% of patients with perforated gallbladder.
Radiotracer in the duodenum or pericholecystic hepatic uptake of radiotracer (the “rim sign”) can be mistaken for gallbladder uptake, resulting in a false-negative interpretation. The finding of pericholecystic hepatic uptake of radiotracer is important to recognize. It is present in 57% of patients with gangrenous cholecystitis and 31% of patients with perforated gallbladder.
 Potential mechanisms by which pericholecystic hepatic uptake occurs include hyperemia with increased delivery and extraction of radiotracer along the gallbladder fossa, focal hepatic cellular injury with impaired excretion of radiotracer, and mechanical obstruction with focally delayed clearance of radiotracer.
Potential mechanisms by which pericholecystic hepatic uptake occurs include hyperemia with increased delivery and extraction of radiotracer along the gallbladder fossa, focal hepatic cellular injury with impaired excretion of radiotracer, and mechanical obstruction with focally delayed clearance of radiotracer.
 If the gallbladder is not seen by 30 to 45 minutes but there is radiotracer in the small bowel, the study can be shortened from 4 to 2 hours by giving intravenous morphine sulfate (0.04 mg/kg; maximum 4 mg). Morphine sulfate contracts the sphincter of Oddi and redirects bile flow into the gallbladder if the cystic duct is patent. The study can be stopped when the gallbladder is filled or at 2 hours (whichever occurs first).
If the gallbladder is not seen by 30 to 45 minutes but there is radiotracer in the small bowel, the study can be shortened from 4 to 2 hours by giving intravenous morphine sulfate (0.04 mg/kg; maximum 4 mg). Morphine sulfate contracts the sphincter of Oddi and redirects bile flow into the gallbladder if the cystic duct is patent. The study can be stopped when the gallbladder is filled or at 2 hours (whichever occurs first).
SUGGESTED READING
Alobaidi M, Gupta R, Jafri SZ, Fink-Bennet DM. Current trends in imaging evaluation of acute cholecystitis. Emerg Radiol 2004;10:256–258.
Grossman SJ, Joyce JM. Hepatobiliary imaging. Emerg Med Clin North Am 1991;9:853–874.
Krishnamurthy GT, Turner FE. Pharmacokinetics and clinical application of technetium-99m-labeled hepatobiliary agents. Semin Nucl Med 1990;2:130–149.
Watson A, Kalff V. Hepatobiliary imaging. Curr Opin Radiol 1991;3:851–858.
Ziessman HA. Acute cholecystitis, biliary obstruction, and biliary leakage. Semin Nucl Med 2003;33:279–296.
MICHAEL W.
HANSON
HISTORY
A 59-year-old man with a history of melena presents with brisk, bright red rectal bleeding. Upper and lower GI endoscopy failed to show a bleeding source.
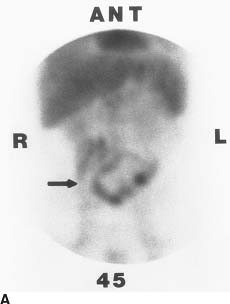
 FIGURE 10-9A Anterior abdominal blood pool images at 45 minutes. Expected radiotracer is seen in the cardiac blood pool, liver, and spleen. Major abdominal vasculature and both kidneys are seen faintly. Moderately intense abnormal radiotracer accumulation is seen in the mid abdomen, the pattern of which conforms to the midportion of the small bowel, most likely the jejunum (arrow).
FIGURE 10-9A Anterior abdominal blood pool images at 45 minutes. Expected radiotracer is seen in the cardiac blood pool, liver, and spleen. Major abdominal vasculature and both kidneys are seen faintly. Moderately intense abnormal radiotracer accumulation is seen in the mid abdomen, the pattern of which conforms to the midportion of the small bowel, most likely the jejunum (arrow).
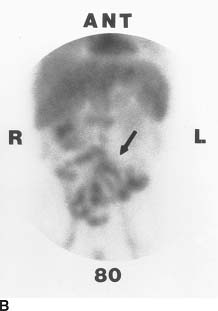
 FIGURE 10-9B Anterior abdominal blood pool images at 80 minutes. The pattern of abnormal radiotracer accumulation now conforms to multiple bowel loops in the mid and distal segments of the small bowel (arrow).
FIGURE 10-9B Anterior abdominal blood pool images at 80 minutes. The pattern of abnormal radiotracer accumulation now conforms to multiple bowel loops in the mid and distal segments of the small bowel (arrow).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


