Fig. 5.1
Vaginal examination in labor with fetal head in occiput posterior position
Ultrasound has become a very useful tool in the diagnosis of fetal head position during labor, in both active phase and second stage (Fig. 5.2). Different approaches, transabdominal (TA), transperineal (TP), and transvaginal (TV), have been investigated by various authors [5–14].
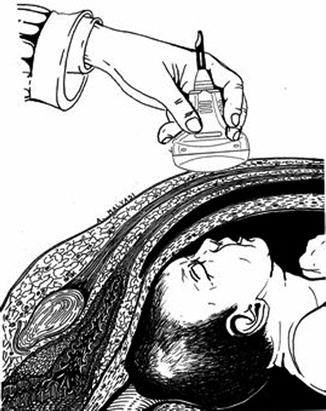
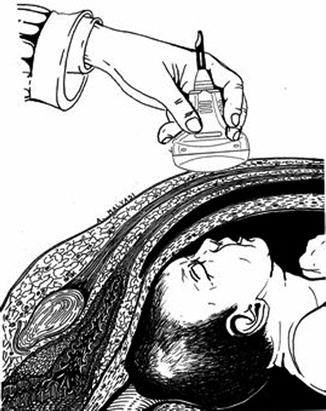
Fig. 5.2
Graphic representation of occiput posterior position by transabdominal ultrasound examination in a longitudinal section
The transabdominal approach is performed obtaining a transverse view with reference to maternal anatomy. Specific fetal anatomical midline structures (cavum septi pellucidi, falx midline, thalami, and cerebellar hemispheres) and anterior or posterior cranial structures (orbits, nasal bridge, and cervical spine) may be visualized [5, 8, 11, 12]. The position of the fetal spine should also be identified at the level of the fetal heart in relationship to the mother’s abdomen. This approach is easy and very reliable during the first stage of labor (see Figs. 5.3, 5.4, and 5.5).
Fig. 5.3
Identification of occiput posterior position by transabdominal ultrasound. The probe is placed on mom’s abdomen on a transverse view (panel a). Specific fetal anatomic structures are visualized. In this case, fetal orbits and nasal bridge are clearly visualized at 12:00 o’clock, just underneath the exploring probe, with the occiput consequently in a posterior position (panel b). In this position one can see the lens of the eye and, through them, one can see the Rotal Eyes Movements (REM). These movements are visible outside the contraction and end during the contraction
Fig. 5.4
Identification of occiput posterior position by transabdominal ultrasound. The probe is placed on mom’s abdomen on a transverse view (panel a). Fetal orbits are visualized at 02:00 o’clock, toward the upper portion of the left pubic rami. Consequently, the occiput is localized at 07:00 o’clock, making an objective diagnosis of right occiput posterior (panel b)
Fig. 5.5
Identification of occiput posterior position by transabdominal ultrasound. The probe is placed on mom’s abdomen on a transverse view (panel a). Fetal orbits are visualized at 10:00 o’clock, toward the upper portion of the right pubic rami. Consequently, the occiput is localized at 04:00 o’clock, making an objective diagnosis of left occiput posterior (panel b)
During the second stage of labor, when the fetal head is engaged and progressing into the pelvic canal, transabdominal approach may be very limiting in obtaining the desired information. The ultrasound probe can then be covered with a glove and positioned transversally at the perineum to achieve a coronal view with reference to maternal anatomy. An image of the fetal head is obtained and specific landmarks identified [5, 11] (see Fig. 5.6).
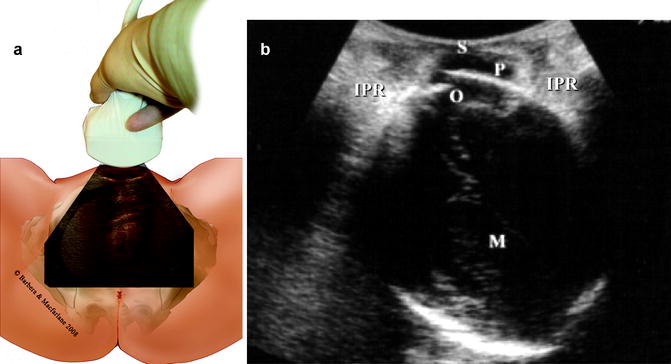
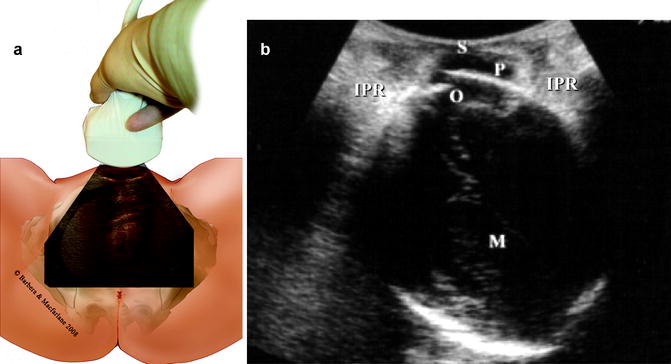
Fig. 5.6
Identification of maternal and fetal landmark by transperineal ultrasound. The probe is positioned on mom’s perineum on a transverse view (panel a). The ultrasound image is reporting an occiput anterior position, but specific fetal landmark can be easily recognized (panel b). S symphysis, P parietal bone, O occiput, M midline brain echo, IPR ischiopubic rami
Zahalka et al. [14] introduced the transvaginal approach as the most successful and accurate method for the determination of fetal head position in the second stage of labor (see Fig. 5.7).
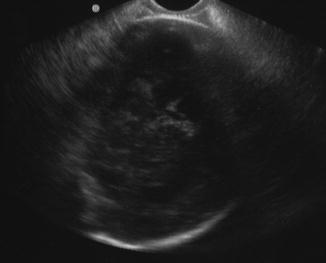
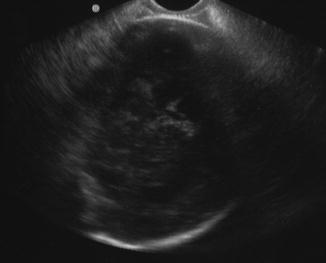
Fig. 5.7
Transvaginal axial view of fetal head. The midline echo is easily recognized as well as the occiput at 02:00 o’clock. Fetal head in left occiput anterior position
5.2 Etiology of OP Position
Cunningham et al. [15] report that 87% of the OP position at the onset of labor end with an occiput anterior (OA) position at time of delivery, and this is most likely secondary to a spontaneous rotation (Figs. 5.8 and 5.9). The remaining 13% of OP delivering in such a position are thought to be a consequence of a malrotation from an initial occiput anterior or transverse position. The exact reason for failure of spontaneous rotation is unknown but a strong contributing factor is certainly a transverse narrowing of the midpelvis.
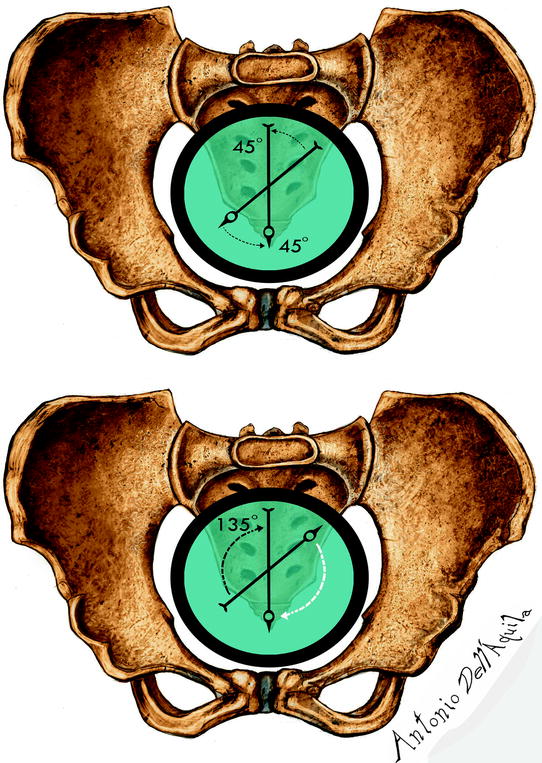
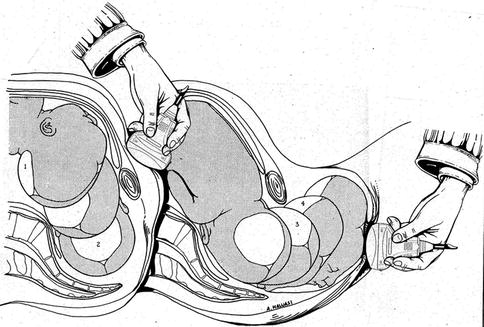
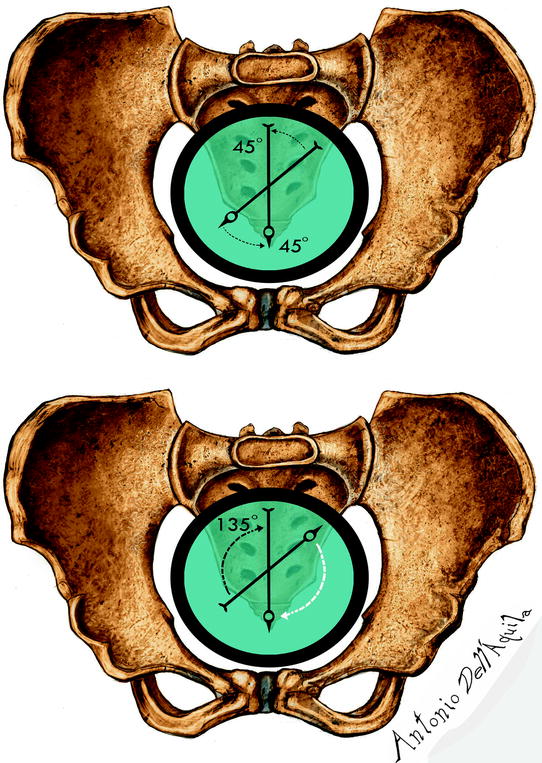
Fig. 5.8
Top, representation of the occipito-anterior rotation of 45° with the head close to the average over the ischial spines. The arrow indicates the rotation in the occipito left front, the narrow top, where the midline sagittal suture or ultrasound are in axis with the conjugated diagonal, and the narrow medium where the sagittal suture and the midline are aligned with the anteroposterior axis pelvic, which corresponds precisely to a rotation of 45°, from left to right. At the center, normal rotation in occipito anterior 45 degrees and below, anomalous rotation in occipito-posterior position of 135°
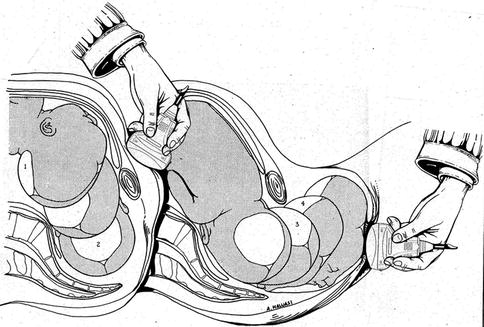
Fig. 5.9
Mechanism of confinement in position occipito back and consequent rotation in occipito anterior, in which the occiput rotates toward the pubic symphysis of 135°
Akmal et al. [16] reported that they did not find any supportive evidence of this concept of malrotation. In their study, the vast majority of OP deliveries were the consequence of failure to rotate from this position during labor, rather than malrotation from an initial occiput anterior.
They found that 70%, 91%, and 100% of OP deliveries were in this position at 3–5, 6–9, and 10 cm of cervical dilatation, respectively. Conflicting results were also reported by other authors.
Gardberg and associates [17] used transabdominal sonography to record the position of the fetal head in 408-term pregnancies at either before the onset of labor or in the early stage of active labor. They reported that 68% of OP position deliveries resulted from malrotation during labor from an initially occipito-anterior position, whereas only 32% of persistent cases were occipito-posterior (dorsoposterior) at the onset of labor (Fig. 5.10).
Fig. 5.10
Measurement of progression angle by translabial ustrasonography in occiput posterior position: (a) Down position, (b) Horizontal position, and (c) Up position
In contrast, Souka et al. [11] reported that 75% of OP deliveries were due to a persistent occiput position during the entire labor. Souka’s ultrasounds were performed during the first and second stage of labor.
5.3 Maternal and Neonatal Outcomes
Independently of its etiology, being persistent during the entire labor or the result of malrotation, the OP position is associated with increased maternal and neonatal morbidity.
In comparison with deliveries occurring in occiput anterior position, OP position deliveries were complicated by increased maternal and neonatal morbidity [3]. Length of labor >12 h (OA 26.2%, OP 49.7%; P < 0.001), oxytocin augmentation (OA 36.8%, OP 48.9%; P < 0.001), chorioamnionitis (OA 1.1%, OP 4.7%; P < 0.001), assisted vaginal delivery (OA 9.4%, OP 24.6%; P < 0.001), cesarean section (OA 6.6%, OP 37.7%; P < 0.001), 3rd/4th degree tear (OA 6.7%, OP 18.2%; P < 0.001), excessive blood loss (OA 9.9%, OP 13.6%; P = 0.03), postpartum infection (OA 0.8%, OP 2,2%; P < 0.01), and Apgar at 1 min 0–6 (OA 7.1%, OP 12.4%; P < 0.001) were all significantly different in nulliparous and multiparous combined in OA position deliveries versus OP position deliveries, confirming that OP position delivery is associated with a variety of adverse maternal outcomes.
Cheng et al. [18] reported a difference in short-term neonatal outcomes of infants delivered in the occiput posterior position when compared with those in the occiput anterior position. Neonates born in occiput posterior position had higher rates of 5-min Apgar scores less than 7 (3.8% for OP, 1.9% for OA; adjusted odds ratio [OR] 1.50 with 95% CI 1.17–1.91), umbilical artery pH less than 7 (1.8% for OP, 0.5% for OA; OR 2.92 with 95% CI 1.84–4.62), and base excess <−12 (2.2% for OP, 0.9% for OA; OR 1.96 with 95% CI 1.42–2.69); more incidence of meconium-stained amniotic fluid (32.3% for OP, 22.7% for OA; OR 1.29 with 95% CI 1.17–1.42), meconium aspiration syndrome (1.2% for OP, 0.7% for OA; OR 1.21 with 95% CI 0.80–1.81), birth trauma (1.4% for OP, 0.8% for OA; OR 1.77 with 95% CI 1.22–2.57), and admission to the intensive care nursery (5.6% for OP, 3.1% for OA; OR 1.57 with 95% CI 1.28–1.92); and higher mean duration of stay in hospital (3.68 days for OP, 2.60 days for OA; P < 0.001). Furthermore, when a composite variable, “neonatal morbidity,” was created to examine the association between fetal position and neonatal outcome, higher rates of neonatal morbidity in occiput posterior delivery were noted (10.7% for OP, 6.0% for OA; OR 1.45 with 95% CI 1.24–1.65).
5.4 Relationship Between Vaginal Digital Examination and Intrapartum Sonography
In the light of all these data about maternal and neonatal outcomes associated with delivery of a fetus in OP position, the correct diagnosis of fetal position in labor is extremely important.
Sherer’s data demonstrated that when compared with transabdominal ultrasound evaluation, digital assessment of fetal head position showed a 76% error rate in 102 women in the active labor [9] and 65% error rate in 112 women during the second stage of labor [10].
In 2003, Akmal et al. [7] examined 496 patients and showed that when compared to abdominal ultrasound, the vaginal digital examinations failed to define the fetal head position in 34% of the cases, and in those in whom the position was defined it was incorrect in 52% if the cases. In 64 patients undergoing to operative vaginal delivery, either vacuum or forceps, Akmal et al. [8




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree