Introduction
In many ways, the challenges related to occupational and environmental lung disease imaging reflect the challenges for all of radiology. The best imaging interpretation relies heavily on the appropriate imaging selection for the particular indication and access to patient history and clinical evaluation. The decision between ordering chest radiography, CT, MRI, or PET can absolutely make the difference for the correct diagnosis or treatment. Knowledge of the patient’s exposure history and relative timing of symptoms plays a critical role in diagnostic considerations. Table 20.1 provides a quick reference for more common occupational and environmental lung diseases seen in practice matched with the associated typical occupational or environmental setting. At other times, the occupational lung disease may have characteristic manifestations that can be incidentally recognized on studies performed for other indications. Making sure that those imaging diagnoses enter into the patient’s medical history and overall care plan is important, but can be challenging. Many diagnoses require multidisciplinary coordination and interaction. Multidisciplinary conferences, ideally including the pulmonologist, occupational and environmental medicine physician, radiologist, and pathologist, provide necessary interactions to weigh the various clinical, laboratory, imaging, and pathology data appropriately, as well as determine the best course for disease surveillance and management. Finally, the radiologist’s knowledge and experience in the various imaging manifestations and complications of disease contribute to the patient’s appropriate workup, diagnosis, and treatment.
| DISEASE | ASSOCIATED OCCUPATIONAL OR ENVIRONMENTAL EXPOSURE |
|---|---|
| Asbestos-related disease | Shipyards, manufacturing, mining, pipe stripping, demolition |
| Silicosis | Foundries, sandblasting, hard rock mining, ceramics construction, stone cutting, grinding |
| Chronic beryllium disease | Ceramics, dentistry, aerospace industry, nuclear weapons and reactors, fluorescent light bulb manufacturing |
| Coal workers’ pneumoconiosis | Coal mining |
| Hypersensitivity pneumonitis | Farming, hot tubs, avian exposures, household water damage, humidifiers, machine operators, paint refinishers |
In other ways, the imaging of occupational and environmental lung disease presents several unique challenges. Some arise from the long history of occupational lung disease imaging. Although screening and surveillance of occupational lung disease with chest radiography have provided a wealth of knowledge about various exposures, the ongoing reliance on chest radiography for diagnosis limits imaging sensitivity for identifying subtle but real disease. Another challenge for radiology arises from the success of mitigating occupational lung diseases in developed nations. Strict government oversight of workplace environment and public awareness of environmental exposures have decreased some inhalational lung diseases in the developed nations, but a highly mobile world population and constant immigration results in the sporadic presentation of unexpected occupational and environmental lung diseases to all radiology practices. Finally, the constant evolution of industrial practices and environmental conditions challenges the radiologist by causing an ongoing broadening of occupational and environmental lung disease while reintroducing well-known pneumoconioses in new settings.
Imaging Modalities
Imaging plays a key role in the screening, diagnosis, surveillance, and management of occupational and environmental lung diseases. The most commonly used modalities include chest radiography (often used as a screening tool) and chest CT. Chest CT is critical for the diagnosis, surveillance, and management of symptomatic patients with an occupational exposure history, as well as for patients with a known pneumoconiosis. CT is the primary modality used to evaluate the type of involvement, extent of involvement, and pulmonary complications of occupational and environmental exposures. For example, chest CT is useful for following the progression of fibrosis and evaluating for potential bronchogenic carcinoma because there is a well-established causal relationship between several of the pneumoconioses and pulmonary malignancy. In most cases, the greater the exposure, the higher the risk of malignancy. Bronchogenic carcinoma is estimated to develop in 20% to 25% of asbestos workers with heavy exposure. Many individuals affected by occupational and environmental lung diseases also smoke tobacco products. Tobacco smoke and asbestos exposure together carry an increased risk of malignancy that is synergistic in increasing the risk of developing lung cancer. Studies have demonstrated a 92-fold or greater increase in lung cancer risk when exposed to both tobacco smoke and asbestos compared to individuals exposed to neither substance. Also, the reported typical latency period for complications of pneumoconioses ranges between 10 and 40 years, so ongoing imaging at regular intervals can be common.
Patients Who Need Radiologic Screening
No well-defined screening guidelines exist for pneumoconioses, and protocols vary by type of exposure and organization. In summary, anyone with respiratory symptoms and/or a significant exposure history could benefit from imaging. The National Institute for Occupational Safety and Health (NIOSH) administers a free voluntary medical screening that must be offered to coal mine workers by their employers as part of the Coal Workers’ Health Surveillance Program. A component of this medical screening consists of a baseline radiograph, subsequent radiographs 3 years later, and, if abnormalities are detected, 2 years later. The Agency for Toxic Substances and Disease Registry (ATSDR) endorses a chest radiograph as a first-line screening for asbestos-related lung disease. If the radiograph is abnormal or inconclusive, and there is an exposure history, a repeat radiograph in subsequent years is recommended. Lateral and/or oblique radiographs are recommended for pleural changes. The ATSDR does not propose chest CT as a screening tool. CT is only advocated in situations in which pulmonary function test results suggest disease without corresponding radiographic abnormality or in cases of indeterminate findings on a chest radiograph. The ATSDR also notes that CT may assist in differentiating pleural plaques from soft tissue densities and cancer from round atelectasis when findings are indeterminate on chest radiograph.
Determining Which Imaging Techniques and Protocols Are Best
For decades, chest radiography has been the primary screening tool for occupational and environmental lung diseases in the United States and worldwide. The advantages of a chest radiograph include low cost, low radiation dose, and availability. Unfortunately, it has been well established that chest radiographs are insensitive for the detection of pneumoconioses, especially the early changes of occupational lung diseases and ground-glass opacities. As many as 10% to 15% of patients with proven asbestosis have normal chest radiographs. In addition to being insensitive, abnormalities demonstrated on chest radiographs are also nonspecific. For example, cigarette smoking can result in many of the same radiographic abnormalities as occupational lung diseases.
Numerous studies have demonstrated that CT is more sensitive for the detection and classification of pulmonary abnormalities associated with occupational and environmental lung disease; however, it is also more costly and confers a higher radiation dose. The most appropriate CT imaging protocol includes image acquisition in both the prone and supine positions, which can be beneficial in differentiating between basilar fibrosis and atelectasis. Likewise, obtaining images in both the inspiratory and expiratory phases of the respiratory cycle can provide evidence of air trapping and small airway disease.
The National Lung Screening Trial (NLST) demonstrated that low dose high-resolution CT (HRCT) decreases mortality from lung cancer in high-risk individuals (smokers and former smokers), although this study did not specifically investigate populations with occupational and environmental exposures. Research has suggested the benefit of screening asbestos-exposed, high-risk individuals with low-dose CT, but more investigation will be required before formal recommendations can be outlined.
Similar to the International Labor Organization (ILO) classification system for radiographs, grading systems for screening HRCT for occupational lung disease have been proposed. A CT classification system would provide a standardized method for evaluating CT images in occupational and environmental lung disease in a systematic, semiquantitative, and reproducible way. In one study in which such a system was used, reliability (as measured by interreader agreement) was deemed satisfactory. Although this type of classification system has been discussed, it has not been verified on a large scale and is not currently in widespread use.
New image reconstruction techniques have also allowed for ultralow-dose CT scans that have comparable sensitivity to standard radiation dose CT scans in detection of asbestos-related diseases. Some of these ultralow-dose CT scans have radiation doses comparable to a two-view chest radiograph. Ultralow-dose CT potentially has a future role in pneumoconiosis screening but has not yet been validated. The sensitivity for the detection of other pneumoconioses other than asbestos-related disease remains unknown. As an example, Fig. 20.1 demonstrates a case of unsuspected subtle asbestos-related pleural disease identified by low-dose lung cancer screening CT.

International Labor Organization Classification of Radiographs
The ILO classification system for radiographs was designed over 60 years ago for the purposes of codifying radiographic abnormalities of pneumoconioses in a simple, reproducible manner for statistical, research, and epidemiologic purposes. It classifies abnormalities based on posteroanterior chest radiograph appearance only. The grading is based on comparison to a set of standard radiographs. Criteria for grading include technical quality, parenchymal abnormalities, pleural abnormalities, and additional abnormalities. Parenchymal abnormalities include opacity type, profusion (the number of small rounded or irregular opacities, which are further subclassified), and extent. The interpreter is instructed not to consider any additional information (e.g., exposure history) when determining the classification. In 2011 the ILO released a classification system for digital radiographs that allows for side-by-side comparison of standards with the current examination on a digital workstation. Not only are digital radiographs more accurate for the classification of abnormalities, they also have the added benefit of reduced radiation dose when compared with conventional radiographs.
Unfortunately, the ILO classification has limitations, including the lack of specificity. An abnormal classification does not necessarily indicate lung disease or the presence of pneumoconiosis, and approximately 5% of patients with an “abnormal” classification have not had any occupational exposure.
A and B Readers
The ILO conducts a course and examination for physicians using the ILO classification system. Trained readers have demonstrated less interobserver variability in classification compared with untrained physicians. It designates the terms A reader for a physician who has completed the ILO course and B reader for one who has passed the accompanying examination. B readers must be recertified every 4 years to maintain B reader status.
Imaging Occupational and Environmental Lung Diseases
Role of PET/CT
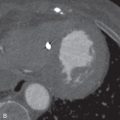
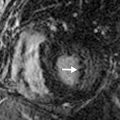
The role of PET/CT is somewhat controversial. Several studies have demonstrated that PET/CT can be helpful in distinguishing benign and malignant imaging features. For example, atypical round atelectasis and pleural plaques, which could be equivocal for malignancy on CT, are not usually fluorodeoxyglucose (FDG)-avid on PET/CT, whereas malignancy characteristically is FDG-avid. Additionally, there have been case reports of the utility of PET/CT in distinguishing progressive massive fibrosis from pulmonary malignancy. However, there have also been reports to the contrary, with cases of FDG-avid, nonmalignant lung nodules in patients with pneumoconioses ( Fig. 20.2 ). The potential role of PET/CT in the distinction of intrapulmonary malignancy from changes associated with occupational and environmental lung diseases is in the process of being elucidated. PET/CT plays an important role in increasing the conspicuity of nodal and extrathoracic metastases in patients with known malignancy and in cases of suspected recurrent mesothelioma, where PET/CT has been shown to be more specific than contrast-enhanced CT.


Role of MRI
At this time, MRI does not have an established role in the imaging algorithm for the workup of occupational and environmental lung diseases. Some research has suggested that MRI is equally as or more sensitive than CT in detecting malignancy in the setting of asbestos-related pleural disease. Although MRI has the benefit of no ionizing radiation, which can be a concern in individuals who require serial follow-up CT examinations, it is much more costly, time-consuming, and usually not as accessible.
Imaging Approach
Role of the Radiologist
Radiologists play an instrumental role in the diagnosis, surveillance, and management of individuals with suspected occupational and environmental lung diseases. Imaging is one component of a multidisciplinary effort in diagnosis and treatment. In addition to imaging, a workup usually includes detailed medical, exposure, and occupational histories (including a smoking history), physical examination, and pulmonary function tests. Radiologists also have the opportunity to add value in cases where an occupational and environmental lung disease was not initially suspected and may suggest this cause in the differential diagnosis. With the increased use of HRCT and ever-expanding insights into the patterns of pulmonary disease, such an occurrence is becoming more commonplace.
Consideration of Occupational and Environmental Lung Diseases
Many occupational and environmental lung diseases can present with imaging features that overlap with other entities, so it is important that they be considered, regardless of exposure history. Pneumonoconioses can share imaging features with hypersensitivity pneumonitis (HP), organizing pneumonia, usual interstitial pneumonia (UIP), nonspecific interstitial pneumonia (NSIP), and sarcoidosis. For example, many cases of pulmonary sarcoidosis can appear similar to chronic beryllium disease (CBD). A case series of patients initially diagnosed with sarcoidosis demonstrated CBD in over one-third of cases on re-review. Thus when sarcoidosis is suggested, CBD should at least be considered as a diagnostic possibility.
Asbestos-Related Disease
Relying on a Clinical History of Exposure
A provided indication of asbestos exposure for an imaging study is the exception rather than the rule, with most cases of asbestos-related pleural disease being recognized incidentally on a chest radiograph or CT scan.
Pleural plaques are the most common imaging abnormality associated with asbestos exposure. The characteristic findings are bilateral calcified pleural plaques, predominantly along the anterolateral upper lobes, posterior and diaphragmatic lower lobes, and mediastinum. Usually, asbestos-related pleural plaques overlie the ribs and involve the parietal pleural; however, visceral pleural thickening does occur and is associated with round atelectasis or an abnormality in the underlying lung parenchyma. The well-defined undulating contour of the pleural plaque has been said to bear a resemblance to a holly leaf when viewed en face on a posteroanterior chest radiograph ( Fig. 20.3 ). Calcification within the plaques is identified on 10% to 15% of chest radiographs and is more common with increasing chronicity of pleural disease. Along the diaphragm, pleural plaques have a plateau appearance that may help differentiate plaques from eventration of the diaphragm.


Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree