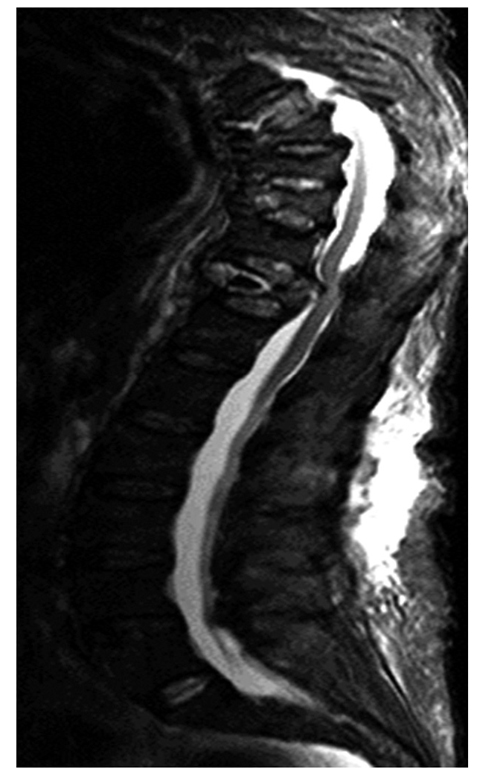
Fig. 1
Asymptomatic degenerate disc disease in a patient aged 45 years
Patients present in a variety of ways and the interpretation of imaging is based very much on the clinical pattern. The syndromes that may be considered are: (1) postural low back pain, (2) nerve root pain (sometimes called sciatica), (3) spinal claudication, (4) cauda equine syndrome and myelopathy, (5) mechanical pain, and (6) difficulty in maintaining sagittal balance.
Specific Patterns of Degeneration
Intervertebral Disc Degeneration
Disc degeneration is signified by tears within the annulus fibrosus. Disruption of the normal contour of the annulus leads to disc bulges and substantial tears lead to disc herniation. There is debate over the significance of hydration of the nucleus. Some studies have shown that there is little change in the hydration and that the signal changes observed on magnetic resonance imaging (MRI) may be regarded as fibrotic changes occurring with annular tears. However, there is up to a 20% decrease in hydration by the third decade of life. The annulus does not normally contain substantial vessels or large numbers of nerve fibres; those who undertake discographic procedures are aware that the periphery of the annulus is a very sensitive area. During the degenerate process there is increasing vascularization and an increasing number of nerve fibres within the degenerate material. In the late stages of degeneration, tears may allow extrusion of nucleus pulposus material into a hernial sac. Disc herniation is very common and may be confined to the region deep within the longitudinal ligament, or may herniate into the spinal canal, or at any point around the periphery of the vertebral disc. The majority of disc hernias are asymptomatic; however, those that cause compression of nerve roots may produce leg pain and neurological deficit.
There is considerable evidence that the acute disc herniation releases a number of chemicals that exacerbate the symptoms. These include prostaglandins, tumor necrosis factor and interleukin.
Annular tears may be associated with a small highintensity zone within the margins of the tear. The socalled high-intensity zone has been associated with increased incidence of pain arising from the affected disc. There is evidence from a comparison of lumbar discography with the high-intensity zone seen on MRI showing that there is a strong association. However, this is not a universal finding and there are patients who will have asymptomatic high-intensity zones.
Joint Degeneration
Facet joint arthropathy follows a similar pattern to osteoarthritis elsewhere in the body. Cartilage fragmentation and thinning is associated with the formation of marginal osteophytes. Bone edema deep to the articular surface resolves. Hypertrophy of the margins of the joint leads to osteophytes that may in turn compress adjacent nerve roots. Mechanical instability of the facet joints arises due to disruption of the normal attachment of the capsule of the joints. Subchondral cysts may form within the facet joints leading to further structural collapse.
The disc space is not a synovial joint; however, osteophytes may form at the insertion of the longitudinal ligaments. Traction osteophytes are associated with mechanical segment instability and may in turn lead to nerve root compression.
Osteophyte formation is more common in the areas of maximum mobility, including the lower lumbar region and the mid-cervical region.
Ligamentous trauma may lead to premature degeneration resulting in an unstable segment.
Although not a direct result of degeneration, osteoporosis may lead to fractures, which in turn cause mechanical instability of the segment and accelerate degenerative changes. In many, the pain associated with vertebral fractures is difficult to disassociate from that resulting from facet joint overload in the same area. Facet joint overload is due to mechanical changes in the shape and structure of the spine.
The combination of facet joint instability and disc degeneration with reduction in vertebral height of the disc will lead to shortening of the spinal column, which in turn may lead to additional mechanical instability and nerve root entrapment.
Nerve Compression and Spinal Claudication
In younger patients, the commonest cause of nerve root compression is disc prolapse. Some patients with lytic spondylolisthesis may also show entrapment of the exiting nerve roots. Older patients with disc space narrowing, facet joint osteoarthritis and facet joint synovial cysts are more likely to have bony entrapment in the narrow exit foramina. In many patients, the nerve compression is multifactorial [1, 2].
Osteophyte formation, loss of height and buckling of the ligament and flavum may cause further narrowing of the spinal canal. This may be associated with disc prolapse, which may worsen or could be the primary cause of the narrowing or stenosis. Spinal stenosis crowds the blood supply to the cauda equina and may cause claudication symptoms, with back pain and leg symptoms associated with walking, which is then relieved by rest. Spinal stenosis of this nature tends to be progressive and it is unusual to see spontaneous improvement. Clinical examination of the peripheral blood supply is important to differentiate spinal from vascular causes. Lateral recess stenosis without central canal stenosis may also cause claudicant symptoms, but is often confined to one side or limited segmental innervation regions [3] (Fig. 2).


Fig. 2
Intervertebral disc prolapse with sequestration; note the increased signal in the disc fragment indicating separation from the parent disc (for color reproduction p 306)
Sagittal Imbalance
Osteoporosis is normally considered a metabolic disorder and not a degenerative disease. However the very high incidence of insufficiency fractures in the aging population is linked to symptoms associated with degenerative disease. Fractures are most often asymptomatic or minimally symptomatic and therefore occur insidiously in older individuals [4]. The structural change due to vertebral collapse increases load on adjacent segments and the overall deterioration in sagittal balance causes pain in remote parts of the spine. Therefore, those with insufficiency fractures old or new will have a predisposition to postural pain resulting from what may be termed „adult spinal deformity”. The concept of sagittal balance is useful. When standing, the center of the C7 vertebral body should be vertically above the centre of the S1 vertebral body. With worsening kyphosis, the first compensation to prevent losing balance is to rotate the pelvis with the iliac crests more posterior and the acetabulae more anterior. When this compensation is exhausted some increase in the cervical and lumbar lordotic curves will occur, and this leads to extra load on the facet joints and may cause impingement of the spinous processes (Baarstrup’s disease). These are common causes of pain on standing. Eventually even these compensations are insufficient and walking is only possible leaning on a walking frame or sticks (Fig. 3).