Fig. 1
Osteomyelitis and bone abscess in the left tibial head of a 24-year-old man. a Anteroposterior radiograph of the left knee shows focal trabecular lysis involving the tibial head (arrowheads). b Coronal STIR image shows an osteolytic area with marked perifocal bone marrow edema and reactive periosteal and soft tissue edema at the medial aspect of the tibial head. c On the axial T1- weighted turbo spin-echo image there is a barely visible thin hyperintense line („penumbra sign”) at the border of the abscess (arrowheads). d The corresponding T1-weighted fat-suppressed post-contrast image shows linear peripheral contrast enhancement of the abscess and lack of central enhancement. There is also contrast enhancement of the periosteal membrane and adjacent soft tissue at the anteromedial aspect of the tibial head
A fluid-sensitive STIR-sequence or fat-suppressed intermediate or T2-weighted turbo spin-echo sequence is the mainstay of magnetic resonance (MR) imaging in the evaluation of suspected osteomyelitis. Acute osteomyelitis can be excluded in the absence of an abnormal high signal in fluid-sensitive sequences [4]. An additional T1-weighted spin-echo sequence is acquired to evaluate the extent and location of osteomyelitis. T1- weighted fat-suppressed spin-echo sequences after intravenous administration of gadolinium-bearing contrast media is the sequence of choice to distinguish abscesses or necrotic tissue from inflammatory edema [5, 6]. On MR images, an ill-defined area within the bone marrow, which is hyperintense on fluid-sensitive sequences and hypointense on T1-weighted sequences, is the typical presentation of acute osteomyelitis [7]. Generally, the size of the lesion is smaller on T1-weighted sequences than on fluid-sensitive sequences or contrast-enhanced fat-suppressed T1-weighted sequences [8]. Perifocal edema is a hallmark of acute osteomyelitis. Without its presence or if the perifocal edema is very thin, the diagnosis of osteomyelitis has to be questioned. Edema in the adjacent periosteal membrane, soft tissue edema and reactive synovitis of adjacent joints may be present. A bone abscess is defined as a circumscribed site of active infection surrounded by sclerotic bone and granulation tissue. Abscesses typically occur in a subperiosteal location in children or in the bone marrow in adults. Both, abscesses and reactive edema are characterized by hyperintense signal on fluid-sensitive sequences. Peripheral enhancement and lack of central enhancement on gadolinium-enhanced sequences is diagnostic of an abscess. Occasionally, a hyperintense rim at the margin of an abscess can be seen on T1-weighted images, which is called „penumbra sign” (Fig. 1c) [9]. The penumbra sign is highly specific for musculoskeletal infection and helpful in differentiating neoplasm from infection [10]. Secondary septic arthritis in osteomyelitis located within the epiphysis is difficult to differentiate from reactive joint effusion and contrast media enhancement of the synovial membrane. In the course of disease there is often a smooth transition from reactive changes in a joint to septic arthritis. Joint effusion and mild synovitis are compatible with reactive changes, whereas septic arthritis is characterized by marked synovitis and enhancement of the adjacent soft tissue. The spectrum of imaging findings in patients with acute osteomyelitis, neoplastic bone disease and stress fractures sometimes overlap. Biopsy may be needed to rule out bone tumors or to identify the causing organism. The latter only makes sense if there was no previous antibiotic therapy.
Chronic Osteomyelitis
Long-standing osteomyelitis over at least 4–6 weeks is defined as chronic osteomyelitis. Clinically less severe, non-septic disease is sometimes termed subacute osteomyelitis.
Brodie’s abscess is the classical form of a clinically less severe osteomyelitis. In around 50% of cases Staphylococcus aureus can be cultivated. Brodie’s abscess is characterized by a sharply delineated focus of infection.
Chronic osteomyelitis in almost all cases occurs due to nonhematogenous route of infection (chronic exogenous osteomyelitis). Primary chronic osteomyelitis initiated by hematogenous seeding is possible but rare [11]. These cases mostly represent acute osteomyelitis with inadequate antibiotic therapy, which turn to chronicity.
The classical route of infection in chronic exogenous osteomyelitis is by direct inoculation of pathogens into the soft tissues and/or bone (traumatic or iatrogenic). The other route is penetration of injured barriers (skin, teeth). Chronic osteomyelitis in the majority of cases shows an acute onset, followed by a chronic course of disease with a strong tendency to relapse. Chronic osteomyelitis is a long-standing disease.
Signs of relapse in the time course of chronic osteomyelitis are destruction of infected bone and formation of new bone, presence of an abscess, sequestrum or involucrum. Formation of a sinus tract, cloaca or fistula may ensue. An abscess in primary chronic osteomyelitis is typically caused by low-virulence organisms and is generally large in size. The term sequestrum indicates a piece of necrotic bone located in the bone marrow or soft tissue without connection to living bone. Sequestra may embody infective organisms and therefore constitute a source of recurrent disease. A sequestrum is characterized by signal-void on fluid-sensitive sequences and lack of contrast enhancement. Bony substance around a sequestrum exhibits hyperintense signal on fluid-sensitive sequences. Reactive, mostly periosteal, new bone formation encapsulating a sequestrum is called an involucrum. An involucrum can completely surround a sequestrum or become perforated by sinus tracts depending on immune competence of the patient and the aggressiveness of the infective organism. A sinus tract increasing in size and forming a gap in the periosteum/involucrum through which pus may discharge is called a cloaca (Fig. 2). Fistulation denotes sinus tracts connecting two internal organs or an internal organ with the skin surface [1].
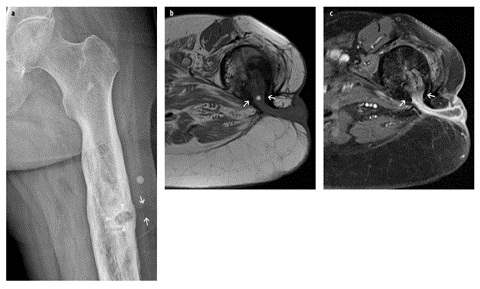
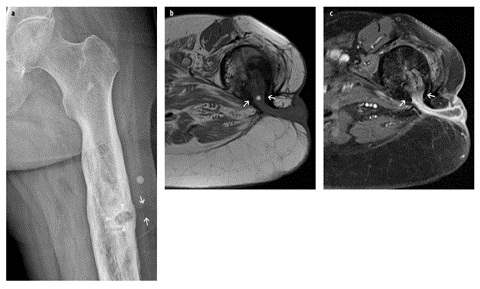
Fig. 2 A–C
Chronic post-traumatic osteomyelitis and cloaca in a 64-year-old man 1 year after a compound femoral fracture. a Anteroposterior radiograph of the left femur demonstrates marked post-traumatic remodeling and a solitary soft tissue calcification at the lateral aspect of the femoral shaft. There is a well-defined osteolytic area (arrowheads) and peripheral osteosclerosis. In the adjacent lateral soft tissues, a barely visible hypodense area (arrows) raises suspicion for soft tissue involvement. On the axial T1-weighted turbo spin-echo image (b) and the corresponding T1-weighted fat-suppressed post-contrast image (c), there is a wide cortical defect (*) with adjacent periosteal new bone formation (involucrum) (arrows). Pus discharges in the adjacent soft tissue forming an abscess without visible fistulation through the skin but marked subcutaneous edema
MR imaging of chronic osteomyelitis follows the same principles as described for acute osteomyelitis. Infection of the bone marrow is characterized by low signal intensity on T1-weighted images and high signal on fluid-sensitive sequences when compared with unaffected bone marrow. On gadolinium-enhanced sequences, granulation tissue and the membrane of an abscess typically enhance, whereas the center of an abscess does not. On diffusion-weighted images, the center of an abscess typically demonstrates high diffusivity [high signal on diffusion-weighted images and low signal on apparent diffusion coefficient (ADC) maps] [12]. This enables identification of pus formations and differentiation from cystic lesions [13, 14]. During the first months after trauma/surgery, osteomyelitis is difficult to distinguish from nonspecific postoperative/post-traumatic changes such as edema, granulation tissue and fibrosis on MR images [15, 16]. Therefore, an abscess or fistula needs to be present to justify the diagnosis of bacterial osteomyelitis. In later stages, marked remodeling processes, such as osteosclerosis, persistent callus and soft tissue fibrosis, may be impressive.
Susceptibility artifacts due to metallic implants may considerably lessen image quality and necessitate adaptation of the imaging protocol. Measures to reduce susceptibility artifacts are: using a scanner with lower magnetic field strength, increasing receiver band-width, reducing echo time, reducing slice thickness, using fast spin-echo sequences instead of spin-echo sequences, using STIRsequences instead of frequency-selective fat saturation, or utilizing novel sequences combining in-plane and through-plane correction for metallic artifacts (e.g., view-angle tilting, VAT, or slice encoding for metal artifact correction, SEMAC, technique) [17].
Septic Arthritis
Septic arthritis is a medical emergency. Hematogenous spread to the synovial membrane and subsequent infection of the joint fluid is the most common route of infection. Otherwise spreading from adjacent (epiphyseal) osteomyelitis or soft tissue infection, post-traumatic direct implantation, postoperative septic arthritis following injections, surgery or arthroplasty is possible. The diagnosis is generally made by joint aspiration. On radio — graphs, the first signs of septic arthritis are periarticular soft-tissue swelling, joint effusion with articular distention, and fuzziness of periarticular fat planes. In pyogenic infections, proteolytic enzymes released by leukocytes and lysosomes based in the synovial membrane rapidly degrade joint cartilage. Therefore, joint space narrowing, bony erosions and juxta-articular osteoporosis are early changes. In tuberculous arthritis, periarticular osteopenia is the main feature, whereas joint space narrowing and bony erosions occur late in the course of the disease.
On MR images, joint effusion and a markedly thickened synovial membrane with contrast enhancement are mandatory for the diagnosis of septic arthritis. Without their presence septic arthritis can be excluded [18]. However, differentiation from reactive changes due to adjacent infection, rheumatoid arthritis or sterile synovitis (e.g., coxitis fugax) may be difficult.
In primary septic arthritis, contrast enhancement of adjacent bone and increased signal intensity on fluid-sensitive sequences are common findings and do not necessarily represent osteomyelitis [19]. Adjacent osteomyelitis may be difficult to differentiate from reactive bone changes. The presence of bone marrow changes isolated to one side of the infected joint, obvious bone erosions and periosteal reaction suggests osteomyelitis [1].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







