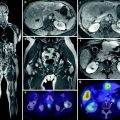
Fig. 1
76yr male with metastatic carcinoid to his liver. He has had the carcinoid syndrome daily for the last 3 years and was treated with long acting octreotide injections. However, the octreotide was starting to become ineffective and he was referred for SIRT. a and b These are representative images from his pretreatment scan demonstrating multiple highly enhancing metastases within his liver. c This is a celiac arteriogram demonstrating the extreme vascularity of the lesions, d and e 4 months after treatment of both lobes of his liver with yttrium-90 microspheres, the previously noted enhancing metastases no longer enhance and have a sharp border. No new lesions were present. His carcinoid syndrome was completely relieved within 1 week after treatment. He remains disease free in his liver 1 year later
The effectiveness of this treatment has been demonstrated in both retrospective and prospective studies. A prospective trial of SIRT using systemic 5-fluorouracil(5-FU) therapy as a radiation sensitizer was conducted and resulted in a 65 % response rate (18 % complete response, 32 % partial response, and 15 % stable disease) (King et al. 2008). The decrease in the amount of disease present, as measured by RECIST criteria, parallels the drop in the systemic biochemical markers with 41 % showing a decrease in Chromogranin A at 3 months and 46 % showing a drop at 30 months with responders showing a greater decrease than the nonresponders. While three-quarters of the patients had carcinoid syndrome, half of these patients reported symptomatic improvement but as important, no new cases of carcinoid syndrome were reported. A survival improvement is expected since at the time of publication, the mean survival had not reached the median. Complications are usually mild with abdominal pain, nausea, fever, and lethargy reported beginning 4–7 days after treatment and lasting between 1 week and 1 month. Gastritis or ulcers were seen in 3/34 patients and there was one death from radiation-induced liver disease. This therapy appears to be a significant improvement over bland or chemoembolization where no complete responders have been reported and the observed survival is shorter than in SIRT. Additionally, most patients did not require hospitalization and the quality of life is much better.
A multi-institutional retrospective review of patients undergoing SIRT for salvage therapy after prior chemotherapy, surgery, and bland or chemoembolization, demonstrated that there was a 86 % response rate with 60 % showing partial response, 3 % complete response, and stable disease in 23 % (Kennedy et al. 2008). Extra-hepatic tumors were responsible for most deaths as has been noted previously (Saxena et al. 2010). The toxicity was also noted to be very low with two-thirds of the patients not having a Grade 3 or 4 event. Safety was again demonstrated with no radiation-induced liver disease appearing.
While there has been no “magic bullet” developed to cure metastatic NETs, a number of studies, both prospective and retrospective, have shown that SIRT is a safe and very effective therapy.
3.1 Practical Aspects of SIRT for mNETs
The basic principles and details of this treatment have been detailed in earlier chapters. However, there are several additional consideration when this treatment is performed that are specific to mNETs:
1.
Pretreatment medications should include the basic anti-emetic and steroid but also octreotide to prevent a carcinoid crisis during the procedure. Two hundred micrograms of octreotide should be administered intravenously immediately before the treatment as well as before the screening arteriograms (Vyleta and Coldwell 2011).
2.
Dosimetry for the best effect in these tumors should take into account the very high vascular volume contained in the tumor. For SirSpheres, the Body Surface Area calculation equation gives a dose that is likely to be appropriate for the tumor. It has been previously noted that a reduction in dose is appropriate in most tumors due to extensive prior therapy; however, the increased vascular volume in these tumors make it more likely than not that such a decrease in dose is not required.
3.
After the SIRT is completed, the patient should be kept on their octreotide therapy for several weeks since the tumors are necrosing and spilling their contents into the systemic circulation.
References
Biku JJ, Davidson BR (2012) Treatment options for unresectable neuroendocrine lever metastases. Expert Rev Gastroenterol Hepatol 6:357–369CrossRef
Chamberlain RS, Brown KT, Canes D et al (2000) Hepatic neuroendocrine metastases: does intervention alter outcomes? J Am Coll Surg 190:432–445PubMedCrossRef
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree