Fig. 1
Microcalcifications: from benign to malignant morphology. Green frame: microcalcifications with typically benign morphology (I); orange frame: microcalcifications with indeterminant morphology (II); red frame: microcalcifications with typically malignant morphology (III) (for color reproduction see p 320)
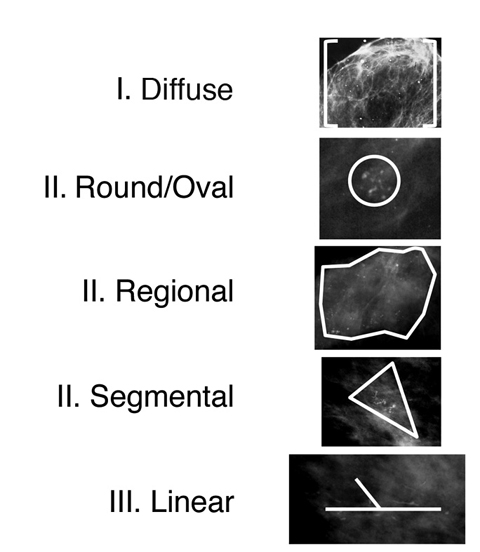
Fig. 2
Microcalcifications: from benign to malignant distribution. Green frame: microcalcifications with benign distribution (I); orange frame: microcalcifications with indeterminant distribution (II); red frame: microcalcifications with typically malignant distribution (III) (for color reproduction see p 320)
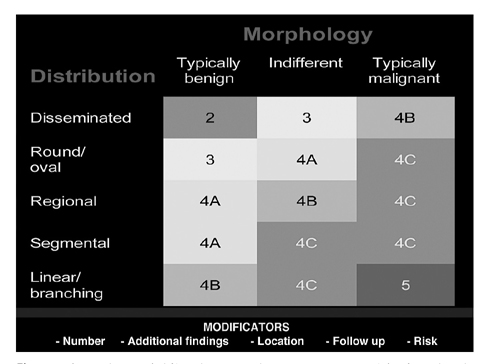
These “distribution modifiers” are evaluated as suggested in the BI-RADS® lexicon. The BI-RADS® lexicon itself neither defines nor quantifies the varying influence of the distribution modifiers on the assessment categories. Some distribution modifiers (regional versus segmental) have not been shown to be of different statistical significance in the literature [20, 21]. Using data found in current literature, the distribution modifiers are attributed to varying probability levels of malignancy [7, 8, 10, 20–22]. Thereby, we have developed the standardized scheme we use for classification of microcalcifications according to the BI-RADS® morphology and distribution parameters [19]. This matrix system is demonstrated in Fig. 3.
BI-RADS® and Indications for Biopsy
While some microcalcifications will be visible on ultrasound, the vast majority of those that require biopsy need to be sampled under stereotactic X-ray guidance using either upright add-on or prone table biopsy systems. It is important to ensure accurate sampling of the microcalcifications and the adjacent breast tissue, and for this reason vacuum-assisted core biopsy (VAB) is the preferred method. Indications for biopsy of calcifications vary but the BI-RADS® system does facilitate some consistency:
BI-RADS® 2 (typically benign); biopsy is not usually indicated.
BI-RADS® 3 (probably benign finding); two different approaches are common: the first involves short interval follow-up (e.g., 6-month intervals for the first two examinations, 12 months for the subsequent two examinations, with a total follow-up time of 3 years). Additional risk factors that should prompt biopsy rather than follow-up are: a strong family history of breast cancer; a personal history of invasive breast cancer, DCIS, lobular neoplasia or atypical ductal/lobular hyperplasia.
BI-RADS® 4 and 5 (suspicious abnormality (Figs. 4–6) and highly suspicious findings Fig. 7. VAB is performed to confirm the diagnosis of cancer, to reduce the rate of underdiagnosis (biopsy: DCIS; operation: invasive cancer; this has potential implications for lymph node biopsy) and to define the extent and type of disease to inform the surgical options (breast conservation therapy, mastectomy) with biopsy at the two most distant regions of the lesion, if applicable.
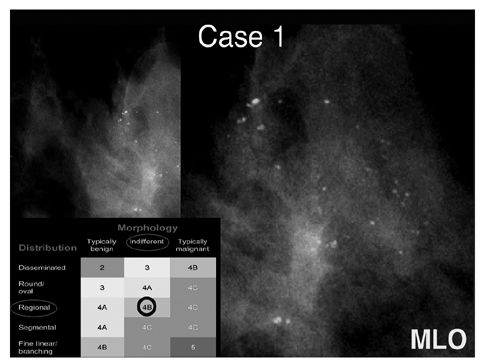
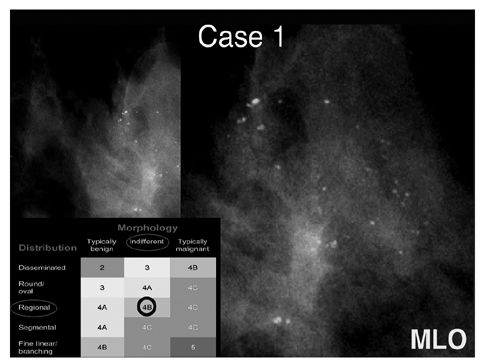
Fig. 4
Case 1: Indifferent type of microcalcifications with regional distribution (BI-RADS, 4B). Histology: fibrocystic changes, sclerosing adenosis, usual ductal hyperplasia. MLO, mediolateral oblique view (for color reproduction see p 320)
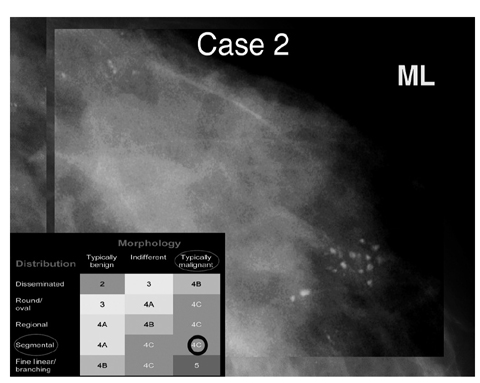
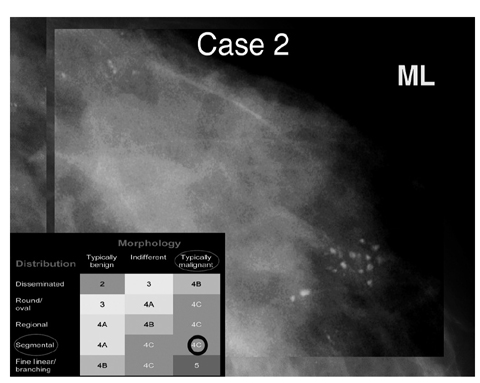
Fig. 5
Case 2: Typically malignant type of microcalcifications with segmental distribution (BI-RADS, 4C). Histology: invasive ductal cancer. ML, mediolateral view (for color reproduction see p 321)
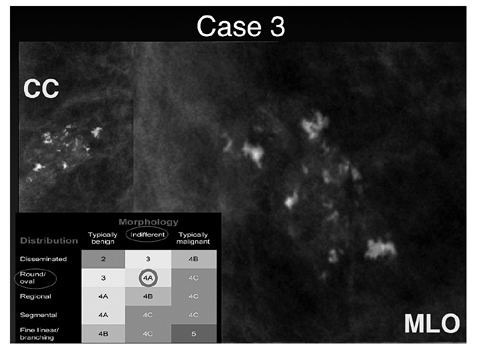
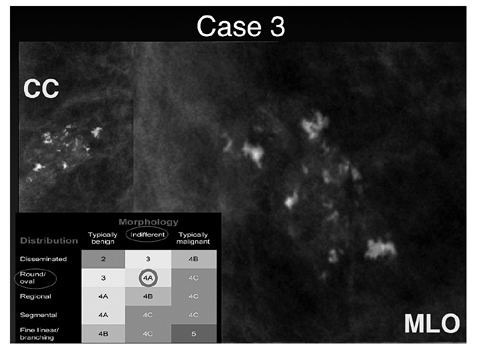
Fig. 6
Case 3: Indifferent (including coarse heterogeneous) type of microcalcifications with round/oval distribution (BI-RADS, 4A). Histology: fibroadenoma, fibrocystic changes. CC, craniocaudal view; MLO, mediolateral oblique view (for color reproduction see p 321)
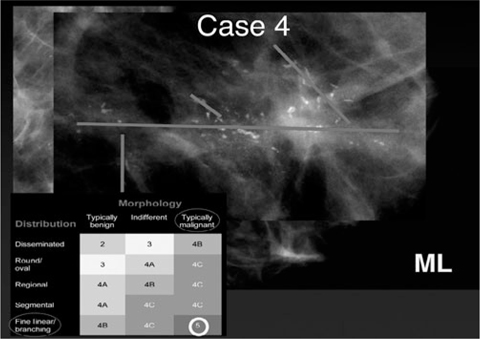
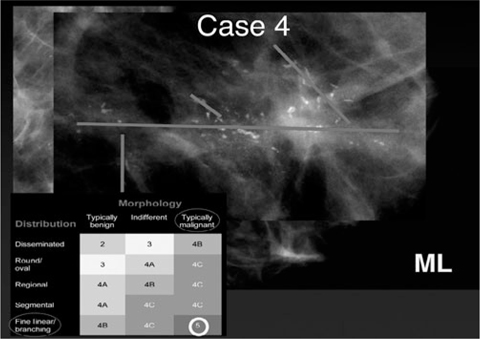
Fig. 7
Case 4: Typically malignant type of microcalcifications with linear and branching distribution (BI-RADS, 5). Histology: ductal carcinoma in situ (high grade). ML, mediolateral view (for color reproduction see p 321)
There are a number of different vacuum biopsy systems available that are suitable for sampling tissue containing calcifications and most are compatible with either prone biopsy or add-on upright systems [23]. The technique for stereotactic breast biopsy is well described elsewhere (15, 24, 25). Lignocaine with adrenaline is the preferred local anesthetic as it reduces hematoma formation and provides longer-lasting anesthesia, particularly as multiple large cores of tissue are usually required for accurate diagnosis. It is imperative that the core samples are subjected to X-ray examination to confirm that sufficient and representative microcalcifications have been retrieved. In case of complete removal of the microcalcifications, one can either insert a marker at the end of the VAB procedure or wait for the histology report and then insert a marker (e.g., Cook coil) into the biopsy hole by ultrasound guidance. Markers that are visible on both ultrasound and mammography are preferred, as they facilitate localization if surgery is then required under ultrasound guidance.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree