Fig. 1
Coronal short tau inversion recovery (STIR) image of the left wrist on a 1.5T extremity magnetic resonance scan. A nondisplaced fracture is visualized in the proximal pole of the scaphoid. No edema is present, consistent with an older fracture
Ulnar Impaction Syndrome
Ulnar impaction syndrome is a common cause of ulnarsided wrist pain. This is often exacerbated by activity and relieved by rest. Impaction between the ulnar carpal bone and the ulnar head may be secondary to positive ulnar variance and leads to degeneration of the ulnar side of the wrist. This can be seen in cases of excessive load-bearing across the ulnar carpus, TFCC and ulnar head [10, 11]. Ulnar variance is the length between the distal end of the ulna and radius measured on PA radiographs. Note that this varies with wrist and forearm pronation and supination, and should only be measured on a standardized PA view [12]. An underlying cause for positive ulnar variance may be shortening of the radius, secondary to a distal radius fracture or a previous surgical procedure. Early changes, such as bone marrow edema and cartilage loss, might be subtle and can be assessed on MRI. Chronic impaction is radiographically evident, showing subchondral cyst formation and sclerosis of the lunate, triquetrum and ulnar head, and joint space narrowing of the ulnocarpal and distal radioulnar joints. However, MR arthrography is the modality of choice to evaluate a degenerative tear of the TFCC and lunotriquetral ligament tear [11]. The treatment most frequently used is ulnar shortening osteotomy (USO). In a retrospective review of 30 patients with ulnocarpal abutment syndrome after a minimum follow-up of 5 years, arthroscopic evaluation of the TFCC at the time of both USO and plate removal was performed. Most TFCC disc tears identified at the initial surgery had healed at long-term arthroscopic follow-up [13].
Distal Radial Ulnar Joint Instability
Another cause of ulnar-sided pain after trauma is damage to the distal radial ulnar (DRU) joint with instability. It can be the result of an isolated injury of the ligament or be part of a complex lesion such as a Colles or Galleazzi fracture. Diagnosis is a challenge, since standard lateral wrist radiographs can only confirm DRU joint instability if a true lateral neutral view is acquired, which may be difficult. In addition, DRU joint subluxation may not be obvious in the neutral position. Cross-sectional imaging with CT can overcome these limitations. In cases of suspected unilateral distal DRU joint subluxation, bilateral wrist CT might be a good imaging modality. Imaging is performed with a straight elbow in extreme supination and extreme pronation. CT criteria for diagnosing dorso- volar subluxation have been examined by Nakamura et al. [14]. In general, the convex articular surface of lateral distal ulna should be congruent with the sigmoid notch regardless of wrist position. However, there is a large variation in DRU joint translation because of differences in laxity of ligaments and other stabilizing soft tissues. The modified radioulnar line method [14] is commonly used because it is simple, has few false-positive results, and good interobserver agreement. To compare both wrists can be of additional value. Dorsal displacement of the ulna with respect to the distal radius is most commonly found, and this increases by pronation. Volar displacement is rare; however, it can be present after a hypersupination injury. The treatment of chronic volar or dorsal DRU joint instability is surgical. Specific surgical procedures such as distal ulna resection-stabilization are used, with good clinical results [15].
Soft Tissues
Ligaments
Scapholunate (SL) and lunotriquetral (LT) ligaments connect the bones in the proximal carpal row and are important stabilizers of the wrist. There is a connection at the dorsal and volar margins of the bones, as well as a central (proximal) membranous component. Imaging modalities used to diagnose ligament tears include radio — graphy in ulnar and radial deviation, arthrography, and CT and MR with and without arthrography [16, 17]. US provides good visualization of the dorsal aspect of the SL ligament, and dynamic imaging (radial and ulnar deviation) may help to diagnose a tear. However, US is not a good method to observe TL tears [18]. With advancing age, the presence of degenerate tear increases [19]. The differentiation between a traumatic and degenerate tear can be made based on the location: a traumatic tear is in the periphery, whereas a degenerate tear is located centrally. A dorsal SL tear is clinically significant and might lead to SL dissociation with wrist instability. Scapholunate advanced collapse, a SLAC wrist, might be the end result [2].
Triangular Fibrocartilage Complex
Direct MR arthrography is the preferred modality to evaluate TFCC as well as wrist ligaments; however, MDCT arthrography can also be used [20, 21]. There is no role for US in the diagnosis of TFCC tears [16]. Single-, double- and triple-compartment injections are used. On MRI, the normal cartilage disc has a low signal intensity on all sequences. However, the radial and ulnar attachments may show an intermediate to high signal intensity on T1- or T2-weighted images, and this should not be interpreted as pathology [19]. In addition, a central, radial-sided communicating defect of the TFCC is often asymptomatic and bilateral. With increasing age defects and central communication within the TFCC increase in frequency [22].
Note that the presence of fluid in the DRU joint on T2- weighted images can be secondary to synovitis or DRU instability.
Without intra-articular contrast, the identification of clinically meaningful ulnar-sided peripheral tears is difficult to diagnose (Figs. 2, 3).

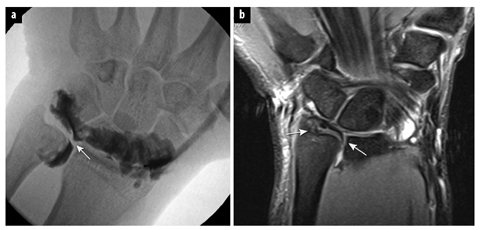

Fig. 2
Fluoroscopic image: needle position for radiocarpal joint injection, located radial from the scapholunate ligament
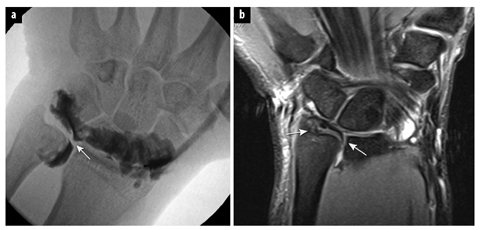
Fig. 3
a Fluoroscopic image of an arthrogram at the radiocarpal joint. Contrast has leaked in the distal radial ulnar joint (arrow). b Coronal T1-weighted fat-suppressed magnetic resonance arthrogram shows the radial-sided defect of TFCC. Contrast leaks in the soft tissues on the ulnar side (arrows)
Tendons
Tendon pathology is a frequent cause of wrist pain. On MRI, the tendons are described based on changes in morphology, signal intensities and associated findings. Surmenage is an underlying cause of wrist tendon pathology, and acute and chronic changes can coexist. Fluid is the hallmark of acute disease, whereas tendon thickening and synovial hypertrophy are predominantly seen in chronic disease. Tendinosis shows an increase in thickness and focal increase of tendon signal intensity on T1-weighted or proton density images, whereas high signal on T2- weighted images in the tendon correlates with intrasubstance degeneration or a partial tear. However, the signal intensity in some wrist tendons is complicated by the magic angle phenomenon, which can simulate pathology. Classically this phenomenon occurs in ligaments and other ordered structures when they are oriented approximately 55 degrees to the main magnetic field (B0) [23]. The tendons of the extensor pollicis longus (third compartment) and flexor pollicis longus, especially on T1- weighted images, are prone to this phenomenon because of their oblique course [19]. On US, the fibrillar structure of the tendons can be well assessed. Changes in echogenicity and volume of the tendons are well visualized. Using the heel-toe procedure, rocking the transducer, differentiates a normal tendon from a pathologic tendon (Fig. 4). In the axial plane, a normal tendon changes from hyper- to hypoechoic, called anisotropy, whereas a pathologic tendon will keep its hypoechogenicity. In addition, the movement of the tendon in the tendon sheath, passively or actively, can be shown, thus diagnosing triggering or a partial or full thickness tear. With color Doppler, the presence of hypervascularization is seen. If necessary, US-guided injection can be performed.
Fig. 4
Axial ultrasound images of the volar wrist at the level of the carpal tunnel (a, b) and palm of the hand (c) demonstrate a diffuse soft tissue mass (asterisks, a) around the superficial and deep flexor tendons extending distally in the palm of the hand (c). Part of the hypoechogenicity is based on anisotrophy (b); however, a definite soft tissue mass is present, with hyperemia secondary to an infection. Clinically, carpal tunnel syndrome was evident. MN median nerve (for color reproduction see p 301)
The wrist tendons can be divided in extensor and flexor tendons. Based on anatomic landmarks, the extensor tendons are subdivided in six dorsal compartments, numbered from radial to ulnar. The deep and superficial flex-or tendons for the fingers pass the carpal tunnel together with the flexor pollicis longus and the median nerve.
Wrist Tendon Pathology
At the level of the wrist, the tendons are surrounded by a synovial sheath. Tenosynovitis, inflammation of the synovial lining, is commonly found. Rheumatoid arthritis (RA) is the number one cause, and tenosynovitis may be one of the first signs of RA (Fig. 5) [24].