Opening Round
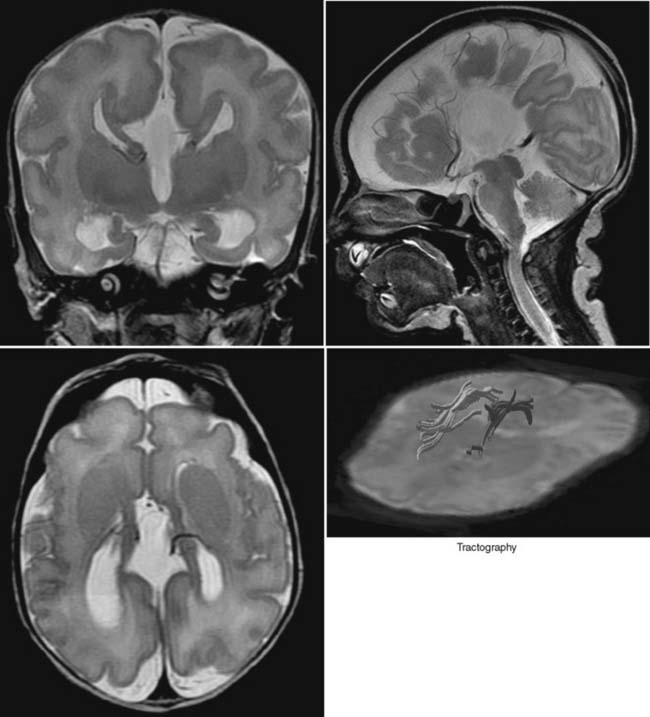
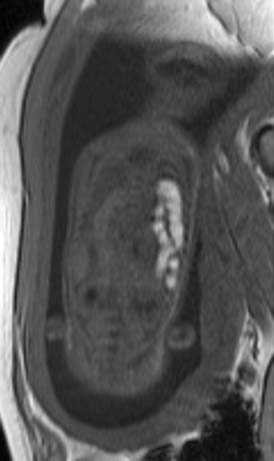
Case 1
Answers: Case 1
Diagnosis: Corpus Callosum Agenesis
Hetts S.W., et al. Anomalies of the corpus callosum: an MR analysis of the phenotypic spectrum of associated malformations. AJR Am J Roentgenol. 2006;187:1343-1348.
Case 2
Answers: Case 2
Diagnosis: Croup
Kuhn J.P., Slovis T.L., Haller J.O. Caffey’s pediatric diagnostic imaging, ed 10, Philadelphia: Mosby; 2004:814.
Case 3
Answers: Case 3
Kuhn J.P., Slovis T.L., Haller J.O. Caffey’s pediatric diagnostic imaging, ed 10, Philadelphia: Mosby; 2004:811.
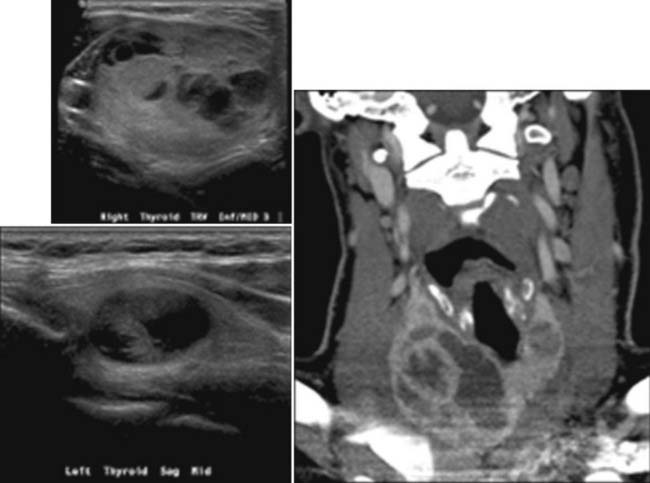
Case 4
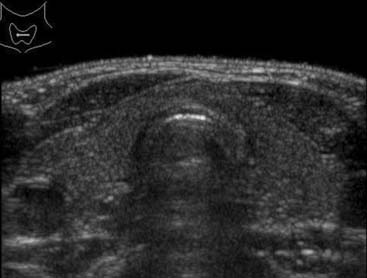
Answers: Case 4
Hegedus L., Bonnema S.J., Bennedbaek F.N. Management of simple nodular goiter: current status and future perspectives. Endocr Rev. 2003;24(1):102.
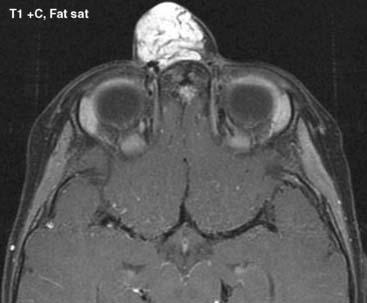
Case 5
Answers: Case 5
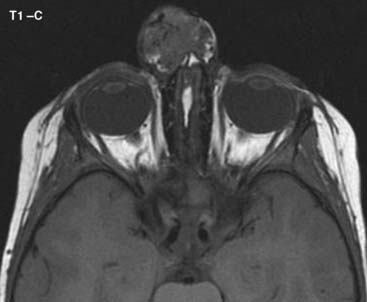
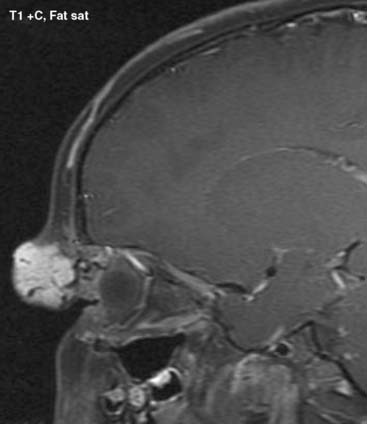
Diagnosis: Nasal Hemangioma
Mulliken J.B., Glowacki J. Hemangiomas and vascular malformations in infants and children: a classification based on endothelial characteristics. Plast Reconstr Surg. 1982;69(3):412-422.
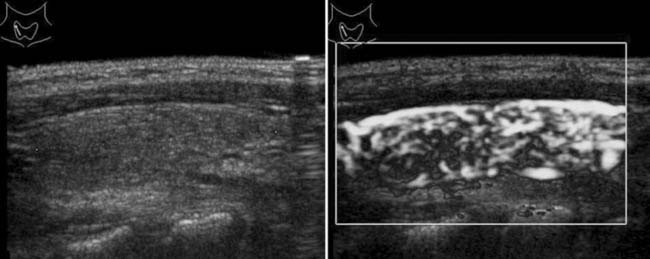
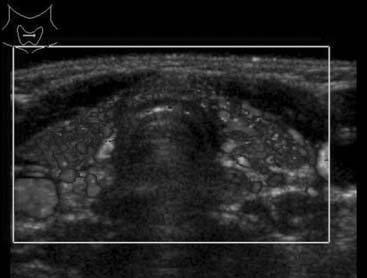
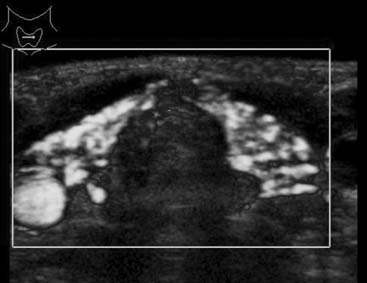
Case 6
Lorini R., Gastaldi R., Traggiai C., et al. Hashimoto’s thyroiditis. Pediatr Endocrinol Rev. 2003;1(Suppl 2):205.
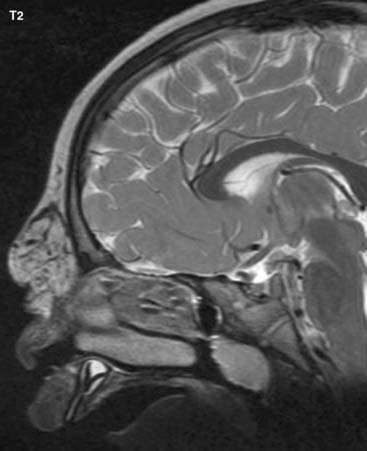
Case 7
Answers: Case 7
Kuhn J.P., Slovis T.L., Haller J.O. Caffey’s pediatric diagnostic imaging, ed 10, Philadelphia: Mosby; 2004:814.
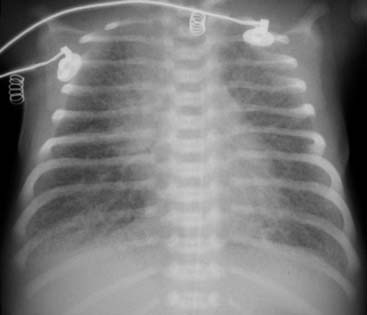
Case 8
Answers: Case 8
Diagnosis: Surfactant Deficiency Disease
Kuhn J.P., Slovis T.L., Haller J.O. Caffey’s pediatric diagnostic imaging, ed 10, Philadelphia: Mosby; 2004:77-79.
Donoghue V. Radiologic imaging of the neonatal chest, ed 2, Berlin-Heidelberg-New York: Springer; 2008:67-72.
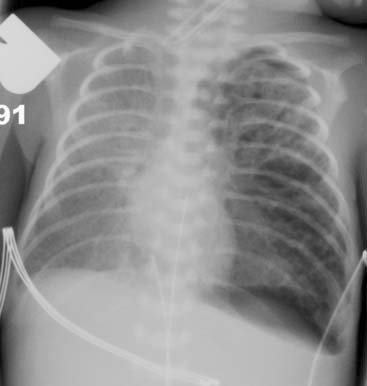
Case 9
Schuh S., Lalani A., Allen U., et al. Evaluation of the utility of radiography in acute bronchiolitis. J Pediatr. 2007;150(4):429-433.
Case 10
Answers: Case 10
Case 11
Answers: Case 11
Diagnosis: Hodgkin Lymphoma
Stage II: Involvement of two lymph nodes on same side of diaphragm (e.g., both sides of neck).
Stage III: Lymph node involvement on both sides of diaphragm (e.g., groin and armpit).
Olson M.R., Donaldson S.S. Treatment of pediatric Hodgkin lymphoma. Curr Treat Options Oncol. 2008;9:81-94.
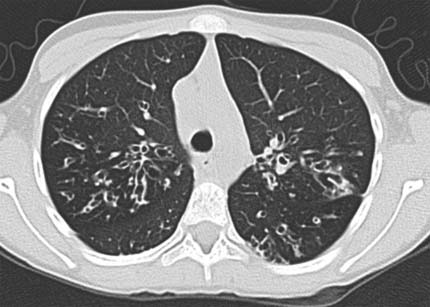
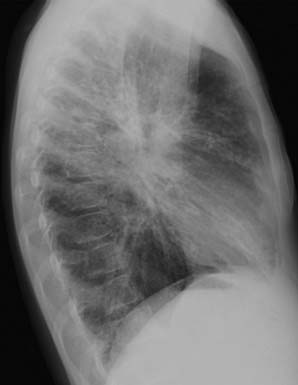
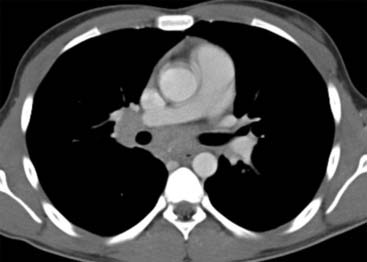
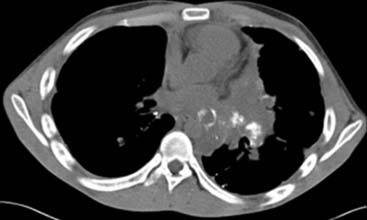
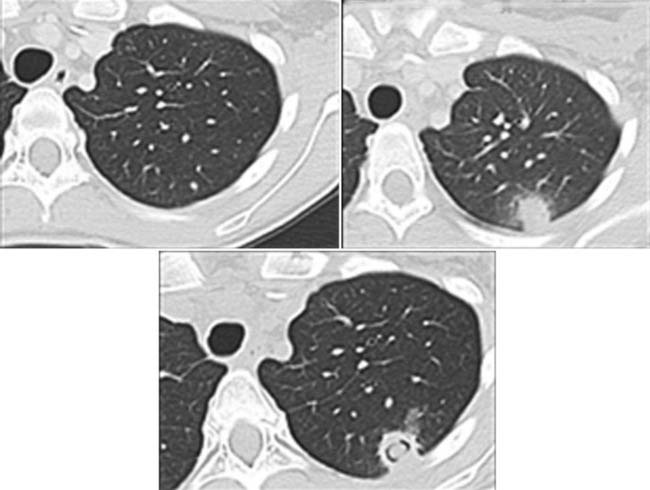
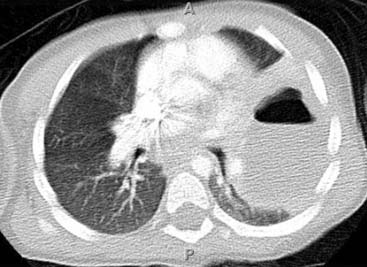
Case 12
Answers: Case 12
Diagnosis: Pulmonary Nodules Due to Osteosarcoma
Antunes M., Benardo J., Salete M., et al. Excision of pulmonary metastases of osteogenic sarcoma of the limbs. Eur J Cardiothorac Surg. 1999;15(5):592-596.
Case 13
Answers: Case 13
Demirkazik F.B., Akin A., Uzun O., et al. CT findings in immunocompromised patients with pulmonary infections. Diagn Interv Radiol. 2008;14:75-82.
Case 14
Answers: Case 14
Diagnosis: Neonatal Pneumonia
Swischuk L.E. Imaging of the newborn, infant and young child, ed 5, Philadelphia: Lippincott Williams & Wilkins; 2004:43-46.
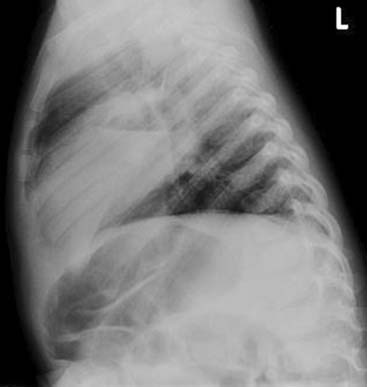
Case 15
Answers: Case 15
Diagnosis: Congenital Diaphragmatic Hernia
Johnson A.M. Congenital anomalies of the fetal/neonatal chest. Semin Roentgenol. 2004;39(2):197-214.
Case 16
Answers: Case 16
Diagnosis: Lung Abscess
Puligandla P., Laberge J.M. Respiratory infections: pneumonia, lung abscess and empyema. Semin Pediatr Surg. 2008;17(1):42-52.