OPTIC NERVE AND SHEATH: ACUTE AND CHRONIC INFECTIONS AND NONINFECTIOUS INFLAMMATORY CONDITIONS
KEY POINTS
- The imaging findings in optic nerve and sheath inflammation and infection are most often nonspecific.
- Imaging can identify associated findings and patterns of disease that aid in the differential diagnosis of causative pathology in some patients.
- Imaging can identify causative conditions for infections that can lead to improved outcomes if treated promptly.
- Imaging can identify complications such as detachments, retained foreign bodies, and compressive factors that may lead to improved outcomes if treated promptly.
Infections may be local or related to systemic disease. For instance, optic nerve syphilis will usually be present as part of disease elsewhere but can occur as the only site of obvious infection. This trend is true of any number of viral, bacterial, fungal, or parasitic infections. Perineuritis may also be a complication of infectious orbital disease or due to spread of an intracranial disease process. Pyogenic sinusitis or rhinocerebral mucormycosis or other fungal infection can involve the orbit and lead to such a complication.
Noninfectious inflammatory diseases may be local or related to systemic disease. The most common is idiopathic demyelinating optic neuritis, which may be seen as an isolated disease or in association with multiple sclerosis.
Meningitides, whether infectious or noninfectious, can spread within or along the optic sheath. This is particularly true of chronic diseases such as tuberculosis, syphilis, sarcoidosis, and Wegener granulomatosis or the histiocytoses.1 Spread of tumor such as lymphoma or meningeal metastases within the subarachnoid space or along the meninges may simulate the benign inflammatory disease. The aim of imaging in these patients with visual loss is usually to exclude compression by tumor, sinonasal pathology, thyroid myopathy, or other lesions as a cause for the optic neuropathy.
ANATOMIC AND DEVELOPMENTAL CONSIDERATIONS
Applied Anatomy
The anatomy of the optic nerve and sheath in relation to the eye and orbit as well as more posterior visual pathways are discussed in detail in Chapter 44. In summary, the optic nerve brings with it layers of pia mater, arachnoid, and dura, and by necessity, subarachnoid and subdural spaces, as it exits the cranial vault via the optic canal (Figs. 44.15, 44.19, 44.22, and 44.23) to eventually join the eye. Any of its segments from the eye to the brain may be involved in these infectious or noninfectious inflammatory processes, a good number of them being meningovascular or leptomeningeal in origin rather than primarily arising from the optic nerve.
IMAGING APPROACH
Techniques and Relevant Aspects
The eye and optic nerve and sheath are studied with ultrasound (US), computed tomography (CT), and magnetic resonance (MR) techniques described in detail in Chapters 44 and 45. The inflammatory conditions involving the optic nerve may be seen coincidentally on images of the brain and face and, therefore, on images with much lower resolving power than when those studies might be focused on the eye and optic nerve or at least the orbit.
Dedicated studies of the eye/orbit must be done with the highest possible resolution given other constraints on all the anatomy that needs to be evaluated. Often, a separate protocol for the eye, optic nerve, and orbit is required if both the brain and eye/orbit must be studied definitively with CT and/or magnetic resonance imaging (MRI).
Specific CT and MRI protocols by indications are detailed in Appendixes A and B.
Pros and Cons
The use of US is for the most part restricted to the identification of a swollen optic disc and possible intraocular complications of the disease. US may show findings immediately adjacent to the nerve–globe junction and around the distal sheath that marginally contribute to the differential diagnosis.
Disease beyond the optic disc is studied primarily with MRI and usually with CT done as an adjunct. MRI is far more definitive than CT in its rendering of the optic nerve as separate from the optic sheath. MRI is also far more sensitive than CT to meningeal pathology. It detects intracranial involvement with these inflammatory processes and their intracranial complications much better than CT. MRI can also screen for related vascular complications and perivascular spread, especially in the cases of fungal disease. Dilatation of the nerve/sheath complex (optic sheath hydrops) on CT can mimic a diffusely infiltrative process; whereas on MR, the cerebrospinal fluid (CSF), nerve, and pathology are almost always easily distinguished2 (Fig. 55.1).
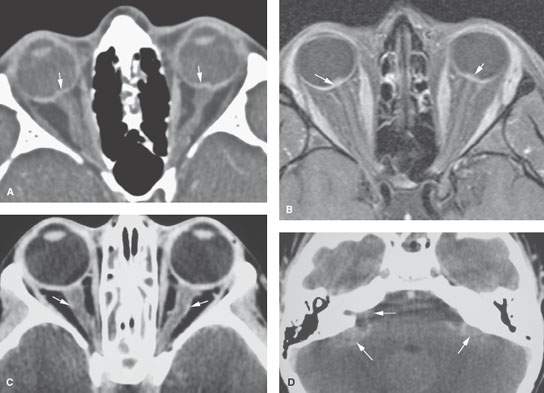
FIGURE 55.1. Imaging studies of three different patients with an enlarged optic sheath. A: Patient 1. Contrast-enhanced computed tomography (CT) study showing the optic sheaths to be dilated bilaterally and the optic nerve heads to be bulging (arrows). This optic sheath hydrops was due to pseudotumor cerebri and not of an inflammatory origin. In the absence of other findings of causative disease, optic sheath hydrops is a nonspecific finding. B: Patient 2. Contrast-enhanced T1-weighted CE magnetic resonance (MR) study showing bilateral optic sheath hydrops and bulging optic disc (arrows) due to pseudotumor cerebri. The nerve/sheath complex is otherwise normal. In the absence of other findings on MR imaging, this can be attributed to raised pressure transmitted through the cerebrospinal fluid (CSF) spaces with a higher degree of confidence on MR imaging than CT, although CSF sampling may still be necessary to confirm raised increased pressure and exclude meningeal pathology. C, D: Patient 3. Contrast-enhanced CT study showing optic sheath hydrops. Study also suggests focal areas of abnormal enhancement of the sheath, although such judgment about subtle meningeal enhancement is typically difficult to make on CT. In (D), this patient also had areas of abnormal meningeal enhancement (arrows). The optic sheath hydrops seen in (C) was due to bacterial meningitis. (NOTE: CT and MR imaging can never exclude meningeal disease.)
CT is used adjunctively or in patients too sick or for some other reason unable to complete a very high quality MRI examination. It is also used to identify possible disease origins in the sinuses and bone changes that might contribute to medical decision making. CT is a reasonable secondary screening tool for identifying intracranial extension of disease and intracranial complications. Computed tomographic angiography is a good and perhaps preferred screening tool to search for vascular complications such as infectious aneurysms and cavernous sinus thrombosis.
SPECIFIC DISEASE/CONDITION
Viral, Bacterial, Fungal, and Parasitic Infections
Etiology
Viral, pyogenic bacterial, granulomatous bacterial (including tuberculosis [TB], syphilis, brucellosis, and others), and fungal infections are all possible etiologies. Parasitic infections including toxoplasmosis, toxocara, schistosomiasis, and cysticercosis can present an acute phase and in general mimic any other source of infection. The infection can be local or systemic.
Self-limited viral infections are likely the most common. Relatively common infections such as catscratch and Lyme diseases as well as those less common such as TB and fungal infections can produce retinochoroiditis and neuroretinitis that can mimic an intraocular mass in its presentation.
When orbital findings are seen on imaging examinations of the face and neck, a sinonasal source or intracranial clues to diagnosis may be visible. Infection may also be secondary to penetrating trauma with a retained orbital or ocular foreign body or seen as a surgical complication.
Prevalence and Epidemiology
These tend to be sporadic infections occurring in both the pediatric and adult populations. Immune suppression can predispose to some infections. Recent surgery or penetrating injury to the orbit or a sinonasal infection considerably raises the risk of pyogenic infection. Populations geographically at risk for certain exposures such as to local parasite populations or Lyme disease will raise the odds of those ocular infections.
Clinical Presentation
Infections usually present with painful loss of vision. An afferent pupillary defect will often be present. Funduscopy will reveal a swollen optic nerve head as well as a possible wide variety of other ocular findings, including uveitis and retinal changes.
Pathophysiology and Patterns of Disease
The pathophysiology of inflammatory conditions and their appearance on imaging studies is discussed in general in Chapter 13.
Inflammatory or infectious disease of the optic nerve/sheath complex will be caused by inflammation of the nerve itself, infectious or noninfectious vasculitis, and inflamed meninges. These will express themselves morphologically in the following ways:
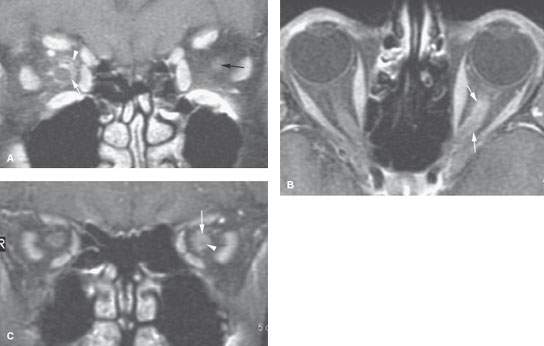
FIGURE 55.2. Two patients with abnormal optic nerve/sheath complex enhancement. A: Patient 1 had a right optic neuropathy. The study shows enhancement of the optic sheath (arrow) and surrounding retrobulbar soft tissues (arrowhead). This was steroid-responsive disease and believed to be due to pseudotumor. Note that the optic nerve does not enhance; it appears essentially the same as the nerve on the left (black arrow). B, C: Patient 2 with optic neuritis and no definite evidence of multiple sclerosis. In (B), the optic sheath enhances (arrows), but it is not possible to determine whether the nerve is also enhancing. In (C), the T1-weighted fat-suppressed coronal image shows clear evidence of optic sheath enhancement (arrow). The nerve is visible within the enhancing nerve sheath complex (arrowhead). The nerve is likely partially enhancing compared to the left side.
- Indistinctness/enhancement limited to the optic sheath or extending into the surrounding retrobulbar fat (Figs. 55.1 and 55.2)
- Enlargement of the optic nerve/sheath complex (Figs. 55.1–55.6)
- Enlargement of the optic nerve (Figs. 55.2–55.4)
- Enhancement of the optic nerve due to blood–brain barrier breakdown (Figs. 55.2–55.5)
- Decreased size of the optic nerve due to atrophy (Fig. 55.4B)
Enlargement of the optic sheath may be exclusively or partially due to optic sheath hydrops. Optic sheath hydrops is pathologic enlargement of the CSF space within the optic nerve/sheath complex; when diffuse, it implies that elevated intracranial pressures are being transmitted to the optic nerve/sheath complex (Fig. 55.1). The CSF space within the optic nerve/sheath complex communicates directly with the anterior suprasellar cistern.
Elevated CSF pressure transmitted to the optic nerve produces clinical and imaging evidence of papilledema (Figs. 55.1 and 55.2). The combination of swelling at the nerve head ending, prominent optic nerve sheath fluid, and a block of communication of the nerve with the subarachoid space (SAS) or a disease that causes rise of intracranial CSF pressure will produce optic hydrops (Figs. 55.1 and 55.7). Dynamic CT has been used to document reduced perfusion to the optic nerve in pathologic conditions that produce optic sheath hydrops and/or optic disc protrusion.3 This may further raise the risk of permanent optic nerve injury due to the inflammatory condition as it causes pressure within the sheath that may impede perfusion of the nerve. This supports the theory that optic nerve fenestration might preserve optic nerve function. CT or MR, however, cannot quantitate the contribution of optic nerve hydrops to the risk of nerve damage and would not be predictive of the outcome of such a procedure.
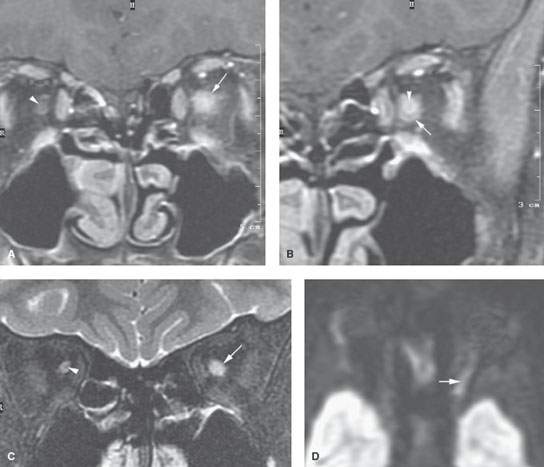
FIGURE 55.3. Pediatric patient with neuromyelitis optica, which is also known as Devic disease. A: Contrast-enhanced T1-weighted (T1W) coronal image shows that both the nerve and optic sheath enhance as well as the retrobulbar soft tissue surrounding the sheath (arrow) compared to the opposite side. B: Close-up T1W coronal image of the affected side clearly shows marked enhancement of the optic nerve (arrowhead) that can be differentiated from the related enhancement of the optic sheath. C: T2-weighted fat-suppressed image showing that the optic nerve cannot be differentiated from the fluid within the optic sheath due to its increased signal (arrow). Note that the optic nerve on the right side is seen but is atrophic due to a prior episode of optic neuritis on the right (arrowhead). D: Diffusion-weighted imaging during the acute phase of the left optic neuritis in this patient showing the restricted diffusion (arrow).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








