OPTIC NERVE AND SHEATH: DEVELOPMENTAL ABNORMALITIES
KEY POINTS
- Magnetic resonance imaging is the study of choice for complete and definitive imaging evaluation of congenital abnormalities of the optic nerve.
- Septo-optic dysplasia is a condition that may have a broad spectrum of abnormalities involving the optic nerve, pituitary gland, and forebrain.
Developmental abnormalities of the optic nerve and sheath are relatively common and may be isolated findings. As with ocular anomalies, these are often associated with other findings involving the visual system and may also be seen as part of syndromes and other more generalized genetic errors. Once a potential developmental abnormality of the eye is recognized, it becomes important to identify such possible related conditions and their likely origin.
The range of eye size variation and focal abnormalities of shape were discussed in Chapter 46, which included a discussion of colobomas and their relationship to the optic sheath/nerve. This chapter is therefore focused on hypoplasia (septo-optic dysplasia) and developmental atrophy of the optic nerve.
ANATOMIC AND DEVELOPMENTAL CONSIDERATIONS
Embryology
The optic vesicles form at 3 weeks of gestation as an eventration of the primitive forebrain.1,2 Subsequently, each optic vesicle first invaginates distally to form an optic cup and optic stalk and then forms a cleft, the choroidal fissure, along its inferior nasal surface (Fig. 46.1 and Chapter 46). The folding in or invagination of the distal optic vesicle creates the two layers of the retina—the neural and pigmented layers. The proximal end of the optic vesicle creates the optic stalk, which ultimately becomes the optic nerve.
Neural crest mesenchyme forms the optic sheath, a duralike covering for the optic nerve. Neural crest cells are also the source of Schwann cells for intraorbital sensory and motor nerves, but no Schwann cells cover the optic nerve.
The visually active cells from the developing retina send their axonal processes retrograde within the optic stalk, filling the central cavity and forming the optic nerve. Axonal processes cross appropriately at the optic chiasm, synapse at the lateral geniculate body, and separate from the hypothalamus. Myelination begins prenatally and extends well into the postnatal period.
Applied Anatomy
The anatomy of the eye and orbit are discussed in detail in Chapter 44. The following section provides a working understanding of the scope of anatomic knowledge required for evaluating abnormal size and shape as well as developmental abnormalities of the optic nerve and sheath.
The optic nerve brings with it layers of pia mater, arachnoid, and dura, and by necessity, subarachnoid and subdural spaces, as it exits the cranial vault via the optic canal (Figs. 44.15, 44.19, 44.22, and 44.23). The subarachnoid space surrounding the optic nerve communicates intracranially with the suprasellar cistern. Variations in the size of subarachnoid space can create differences in the apparent size of the “optic nerve.” Optic nerves are virtually always symmetric in size, but the optic nerve/sheath complex (nerve, sheath, and space) varies; it measures 5.5 +/− 0.7 mm just posterior to the nerve–globe junction and 4.2 +/− 0.6 mm at its waist.3 It may be difficult to clearly distinguish the optic nerve from its sheath when the intervening subarachnoid space contains only a small amount of cerebrospinal fluid. Coronal T2-weighted images show that the optic nerve in adults normally measures 2.5 +/− 0.4 mm (1 standard deviation = 0.2 mm). It may be slightly smaller in young children.
IMAGING APPROACH
Techniques and Relevant Aspects
Ultrasound is generally performed with a 10- to 12-MHz transducer. Either A-mode or B-mode and color flow and power Doppler techniques are used depending on specific indications.
Specific computed tomography (CT) and magnetic resonance imaging (MRI) protocols by indications are detailed in Appendixes A and B.
Intravenous contrast is used frequently. If calcifications are important to the detection of pathology and/or the differential diagnosis, a noncontrast acquisition should be done. That decision should be made on a case-by-case basis to avoid a radiation dose to the lens.
Pros and Cons
Disorders of the optic pathways should almost always be studied with magnetic resonance (MR). MR displays the entire visual pathway, including the optic nerve, chiasm, and tracts as well as the lateral geniculate body, optic radiations, visual cortex, cavernous sinus, and brain stem. In these developmental abnormalities, MRI will clearly allow the most definitive complete evaluation of optic nerve size and possibly associated anomalies of the brain.
SPECIFIC DISEASE/CONDITION
Optic Nerve Hypoplasia (Septo-Optic Dysplasia) and Aplasia
Etiology
Hypoplasia (septo-optic dysplasia) is one of the milder forms of brain and orbital developmental disorders associated with ventral induction of the neural axis in the first trimester of gestation (Figs. 53.1–53.5). It is also known as de Morsier syndrome. It is likely best to consider this disorder as one of a spectrum of anomalies that may affect the optic nerve, hypophysis, and forebrain.4,5
Aplasia of the optic nerve and eye are rare (Fig. 46.6). This occurs sporadically due to failure to form the optic vesicle. Absence of eye development results in concomitant orbital hypoplasia and facial deformity.4 Leber hereditary optic neuropathy (LHON) eventually leads to bilateral optic nerve atrophy (Fig. 53.6).
These are due to chromosomal abnormalities that are usually sporadic due to any variety of teratogens and are occasionally syndromic.
Prevalence and Epidemiology
There is no gender predilection, and these not uncommon anomalies occur worldwide except for LHON, which is passed maternally only to males.
Clinical Presentation
Vision in children with mild optic nerve hypoplasia can be near normal. However, in children with smaller and paler optic nerves, visual impairment may be severe. Children with bilateral disease may demonstrate nystagmus. There may also be evidence of pituitary dysfunction and hormonal deficiencies, most commonly in infants with severe bilateral disease and nystagmus.
Pathophysiology and Patterns of Disease
Hypoplasia (septo-optic dysplasia) is one of the milder forms of brain and orbital developmental disorders associated with ventral induction of the neural axis in the first trimester of gestation.4,5 The optic nerves, chiasm, and tracts develop concurrently with the ventral induction process, and inhibition of ventral induction results in several brain fusion problems including semilobar and lobar forms of holoprosencephaly and septo-optic dysplasia (Figs. 53.1–53.5). The latter is characterized by absence of the septum pellucidum, focal ectasia of the frontal horns, and hypoplasia of the optic nerves. Eye development is generally normal. The failure of brain development results in limited need for optic fibers, hence the optic nerve hypoplasia. Migrational abnormalities of the brain also commonly occur in this condition. Both anterior and posterior pituitary dysfunction may also occur5 (Fig. 53.2).
Aplasia of the optic nerve and eye are rare. This occurs sporadically due to failure to form the optic vesicle. Absence of eye development results in concomitant orbital hypoplasia and facial deformity.4
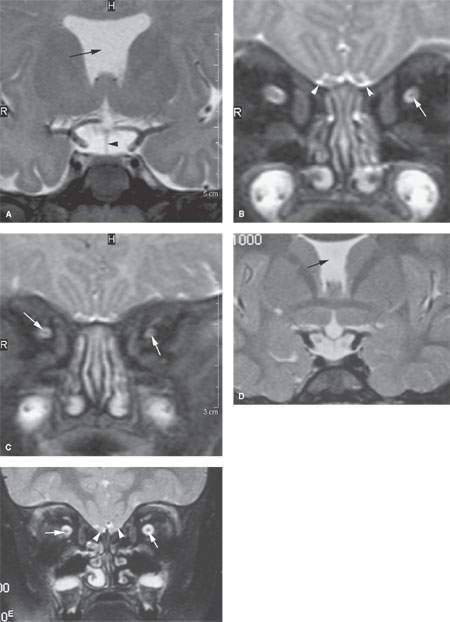
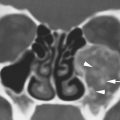
FIGURE 53.1. MRI of a child with septo optic dysplasia. A: T2-weighted (T2W) coronal image shows an absent septum pellucidum (black arrow). The pituitary (arrowhead) is present, but the optic chiasm is not seen. B: T2W coronal image shows atrophy of the left optic nerve compared to the right (arrow) and normally developed olfactory structures including the olfactory tracts, olfactory sulcus, and gyrus rectus (arrowheads). C: T2W coronal image more posterior than (B) shows that there is actually bilateral optic nerve atrophy (arrows) showing that the optic nerves can appear segmentally abnormal in this disease. A different patient with septo-optic dysplasia seen in (D) and (E). In (D), there is an absent septum pellucidum (arrow). In (E), there is bilateral optic nerve atrophy (arrows). The olfactory region is markedly abnormal (arrowheads) with abnormal fusion of the olfactory tract and bulb to the dysmorphic inferior frontal lobe. There is no normal olfactory sulcus or gyrus.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree