OPTIC NERVE AND SHEATH: TRAUMA
KEY POINTS
- The imaging findings in optic nerve trauma are critical to treatment decisions, including precise surgical planning.
- Computed tomography may not be definitive in acute trauma; in highly selected cases, magnetic resonance imaging may help with treatment triage.
- Imaging can identify findings that are critical to the prognosis.
- Imaging may help detect a complicating infection or retained foreign body.
- Computed tomography should not be used for evaluating the optic nerve after radiation or for chronic traumatic effects unless magnetic resonance imaging is not possible.
Acute, direct trauma to the optic nerve may be blunt force or penetrating from a wide variety of untoward events. Both mechanisms can also occur during surgery, and both may result in the presence of retained foreign bodies. Indirect traumatic optic neuropathy can occur from blunt force injury without a direct gross injury to the optic nerve or sheath or overt bony compression.
The chronic effects of optic nerve trauma due to those blunt force and penetrating injuries as well as those due to radiation therapy are also discussed.
ANATOMIC AND DEVELOPMENTAL CONSIDERATIONS
Applied Anatomy
The anatomy of the optic nerve and sheath in relation to the eye and orbit as well as more posterior visual pathways are discussed in detail in Chapter 44. In summary, the optic nerve brings with it layers of pia mater, arachnoid, and dura, and by necessity, subarachnoid and subdural spaces, as it exits the cranial vault via the optic canal (Figs. 44.15, 44.19, 44.22, and 44.23) to eventually join the eye. Its segments most likely to be involved in blunt force and penetrating injury are those in the orbit and optic canal. The portion of the optic nerve most often involved by radiation-induced neuritis is that segment just distal to the optic chiasm and that segment within and just distal to the optic canal.
IMAGING APPROACH
Techniques and Relevant Aspects
The eye and optic nerve and sheath are studied with the ultrasound (US), computed tomography (CT), and magnetic resonance (MR) techniques described in detail in Chapters 44 and 45. The traumatic conditions involving the optic nerve may be seen coincidentally on images of the brain and face and, therefore, on images with much lower resolving power than when those studies might be focused on the eye and optic nerve or at least the orbit.
Dedicated studies of the eye/orbit must be done with the highest possible resolution given other constraints on all of the anatomy that needs to be evaluated. Often, a separate protocol for the eye, optic nerve, and orbit is required if both the brain and eye/orbit must be studied definitively with CT and/or magnetic resonance imaging (MRI).
Specific CT and MRI protocols by indications are detailed in Appendixes A and B.
Pros and Cons
CT is the primary imaging examination for evaluation of blunt force and penetrating orbital trauma, with MR used adjunctively in those trauma patients and primarily for the evaluation of radiation optic neuritis. CT can identify most clinically significant findings affecting the traumatized eye, optic nerve, and bony orbit. The extent of bony injury may be a critical determinant in the evaluation of potential optic nerve injury and for evaluation of orbital injury that may require repair. CT is also capable of detecting a retained foreign body. CT is also the primary study for evaluating delayed complications of trauma such as infection.
MR is used adjunctively in highly selected cases of possibly retained foreign bodies and in delayed complications such as orbital infection. It is the primary study for evaluating disorders of the visual pathways that might be related to radiation injury.
SPECIFIC DISEASE/CONDITION
Direct and Indirect Optic Nerve Injury Due to Blunt and Penetrating Trauma
Etiology
Blunt and/or penetrating trauma most commonly occur due to motor vehicle and bicycle accidents, assaults, altercations, sports injuries, gunshot wounds, and a host of less usual circumstances. Operative optic nerve injury occurs most commonly during the surgical repair of combined orbital and facial injuries.
Any traumatic event may be associated with a secondary infection. Those effects are discussed in Chapter 50, and their end result may follow a final common pathway that leads to loss of vision.
Prevalence and Epidemiology
Traumatic optic neuropathy has an incidence of approximately 2.5% following midfacial fracture and has been reported to occur in 2.0% of patients with closed head trauma.
Clinical Presentation
The injuries are almost always clinically obvious to both the patient and the treating physician; however, there may be so much periorbital and intraorbital swelling that the eyes cannot be examined. In less obvious injury, pain and alteration in visual acuity will be the dominant complaints. The diagnosis of direct injury to the optic nerve and/or indirect traumatic optic neuropathy requires documentation of diminished vision manifest as either decreased visual acuity, loss of side vision, or decreased color vision and an afferent pupillary defect.
Pathophysiology and Patterns of Disease
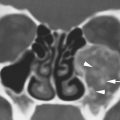
The optic nerve may be compressed, transected, avulsed, or lacerated by the force of the trauma and/or from a penetrating foreign body or bony fragment (Fig. 54.1). These are all self-evident direct effects of trauma. Optic nerve sheath hematoma may compress the optic nerve. Optic nerve transection is seen in severe blunt force orbital trauma with fractures or penetrating orbital injury. Optic nerve avulsion usually follows severe orbital trauma but can occur with relatively minor eye trauma (Fig. 54.2). Diffuse orbital hemorrhage and orbital emphysema can lead to tension orbit (Fig. 48.3 and Chapter 48), and a discreet orbital hematoma can produce the same effects (Fig. 48.2). Optic nerve sheath hematoma may be difficult to detect, and it is not predictable based on mechanism of trauma. These direct injuries should be considered as a separate entity compared to the indirect traumatic optic neuropathy not associated with such usually self-evident mechanisms.
The exact mechanism of traumatic optic neuropathy is poorly understood. It typically follows blunt trauma to the superior orbital and lateral orbital rims and/or orbital frontal area. It is likely due to concussive and transiently compressive forces transmitted to the orbital apex and optic canal. The portion of the optic nerve in the optic canal is likely contused and edematous, resulting in secondary injury due to swelling-induced local ischemia (Fig. 54.3). This is similar to the secondary injury that occurs in the traumatized brain in closed head injury; since the optic nerve is much like the brain, such a mechanism of primary and secondary injury seems logical. This is compounded by the swelling occurring in a bony canal; thus, the secondary changes recycle the injury process somewhat analogous to brain swelling within the skull.
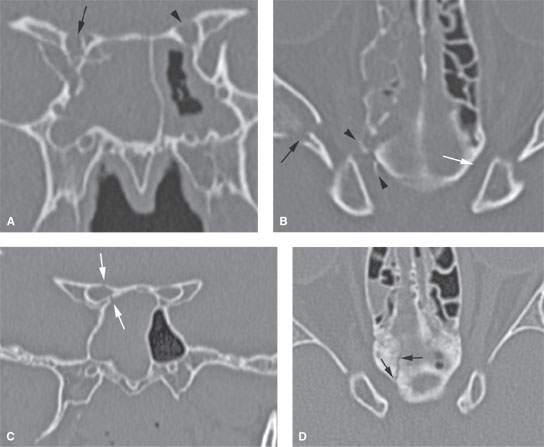
FIGURE 54.1. CT scans of two patients suffering craniofacial trauma. A, B: Patient 1. In (A), there is a comminuted fracture of the right optic canal compared to the left, which appears normal (arrowhead). In (B), the axial sections show a fracture through the greater wing of the sphenoid (arrow) and bony fragments present within the optic canal (arrowheads) compared to normal optic canal on the left (white arrow). C, D: Patient 2. In (C), there is a nondisplaced fracture through the right optic canal (arrows). In (D), the fracture seen in (C) was an extension of fractures of the anterior skull base (arrows). Both of these patients had compromised visual acuity. The second patient recovered eyesight. The first did not.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree