ORAL CAVITY AND FLOOR OF THE MOUTH: INTRODUCTION
IMAGING APPROACH
Techniques and Relevant Aspects
General Examination
Patients should be positioned with the neck extended so that the mandibular body is perpendicular to the tabletop for either computed tomography (CT) or magnetic resonance (MR) study. When using multidetector computed tomography (MDCT), the data acquisition is best done with zero gantry tilt. This may cause problems when dental fillings or unremoveable appliances are present. If the images are severely degraded by these artifacts arising from dental appliances, one solution is to obtain a second series of CT images with the mouth opened.1 The CT gantry may also be angled, based on the planning digital radiograph, to minimize artifacts produced by dental appliances that cannot be removed and two separate data acquisitions done at the expense of some reirradiation of overlapping sections. At least one acquisition angled along the body of the mandible should be obtained in any case. Alternatively, a complementary MR study may be done.
Oral cavity CT and magnetic resonance imaging (MRI) always includes axial views as a routine and routine use of coronal sections. Coronal and sometimes sagittal viewing is essential for many studies of cancer patients and in those cases when there is a complex relationship between the pathology and the floor of the mouth, tongue base, mandible, and spaces of the suprahyoid neck.
On CT studies, axial sections are acquired and then these source images are archived. Axial images are the mainstay for evaluating pathologic relationships in most critical anatomic zones. MDCT ($16 slice) makes it simple to obtain the axial images as a volume data set that can be routinely reconstructed and then viewed with multiplanar reformation tools in virtually any plane, as discussed in Chapter 2. These volume CT data sets should be obtained with 0.5- to 1.0-mm sections suitable for the highest-resolution multiplanar reconstructions and/or reformations required for the diagnostic task at hand. Reconstruction of the images at 1 to 3 mm slice thickness (SLT) is, however, suitable for evaluating the soft tissue extent of cancers, and reconstructing at that larger SLT will improve low-contrast resolution considerably and will suffice when fine bone detail and reformations are not necessary (Appendix A). Sections to evaluate bone detail should not exceed 1 mm.
Iodinated contrast is used on almost all oral cavity CT studies. If iodinated contrast cannot be used, then MRI should be done instead unless only bone information is the object of interest. It is very important not to begin scanning too early in the contrast injection. Peak enhancement of most cancers and other pathology not directly related to blood vessels relative to normal tissue may be missed if scanning is begun too early. Specific CT protocols are presented in Appendix A.
MRI should be done with 3- to 4-mm sections and a field of view of about 12 to 16 cm. All three orthogonal planes might be obtained, but axial and coronal sections almost always suffice. T1- and T2-weighted images should be obtained. Fat suppression may be used but may be unpredictably degraded by susceptibility artifacts in critical areas such as the mandible, usually due to dental appliances (Fig. 1.3). Non–fat-suppressed T1-weighted images before and after contrast and T2-weighted images are a safer choice, although the examination becomes lengthened. Intravenous contrast is used in most cases. MR protocols are presented in Appendix B.
MRI is primarily done in the axial plane, almost always parallel to the mandibular body. The axial images are the mainstay for interpretation. Coronal and sagittal acquisitions are done selectively to evaluate depth of penetration of processes into the floor of the mouth and whenever there is a complex relationship between the pathology and the floor of the mouth, tongue base, mandible, and spaces of the suprahyoid neck. Sagittal images are only occasionally useful or necessary.
Pros and Cons
CT and MR are used for the majority of nondental imaging in the oral cavity. Plain radiographs, orthopantomography, and occlusal views remain useful tools for studying the teeth and mandible as discussed in Chapter 96. Dental-related artifacts can seriously degrade both CT and MR images through the oral tongue and mid oral cavity in general. The problem is generally worse on CT. The problem is accentuated on MRI when fat suppression is used. MRI is very frequently significantly degraded by jaw and other motion as discussed in Chapters 1 through 3.
Ultrasound has a very limited, if any, role in oral cavity pathology. There is some adjunctive and experimental usage using elasticity to evaluate the degree of invasiveness at tumor margins and its relationship to risk of nodal metastases.
Angiography is used occasionally in both diagnosis and treatment settings. Catheter angiography is necessary if angioarchitecture and temporal flow dynamics of a lesion are in question. If not, then CT and/or MR angiography will usually suffice; 320 MDCT or its equivalent will replace most diagnostic angiography. Angiography is almost always used following imaging studies, although it is occasionally the primary examination in conditions such as intractable bleeding or as a prelude to endovascular procedures.
Radionuclide studies, particularly single photon emission computed tomography (SPECT) gallium and bone scanning, are useful in highly selected cases of infectious disease. Fluorine-18 2-fluoro-2-deoxy-D-glucose positron emission tomography (FDG-PET) is used selectively in cancer patients. It should not be used routinely since it will most often not alter management decisions or outcome. Specific radionuclide technique depends on the indications, and this is discussed elsewhere and in general in Chapter 5.
Specific Areas of Interest
Developmental Abnormalities
Potentially cystic congenital lesions that primarily arise outside the oral cavity with potentially complex relationships to the floor of the mouth and deep spaces of the suprahyoid neck or even potential central nervous system connections are very effectively imaged with MR—especially in children, where one would like to limit exposure to ionizing radiation.
If MRI, CT, or the clinical evaluation suggest a venolymphatic or other vascular malformation, then angiography may be done to confirm this impression if there is a potential of a high-flow lesion and may be used to direct endovascular or direct injection as part of therapy. Such treatment may be definitive treatment or an adjunct to surgical removal.
Inflammatory Disease
Complex inflammatory oral cavity disease, such as that associated with a high likelihood of associated abscess or when the source of the inflammation is uncertain, are studied with contrast-enhanced computed tomography (CECT) since dental disease and submandibular gland pathology are very common sources of such pathology. MRI may be used very occasionally as a supplemental study.
Determining the Extent of Known Oral Cavity Cancer and Related Regional Lymph Node Metastases and Evaluation of Masses of Uncertain Etiology and Posttreatment Surveillance
Patients with benign and malignant tumors of the oral cavity usually present with obviously mucosal masses. They occasionally present with submucosal masses or pain, trismus, or other functional complaints related to swallowing, mastication, or speech without a visible mass. Either sublingual or submandibular glands may be a source of such pathology.
Both CT and MR can be used to demonstrate the presence, possible nature, and extent of a mucosal or submucosal mass lesion. In most cases, a CT study is usually adequate for all of these tasks. A variety of sometimes unusual lesions, either benign or malignant, can be encountered in this clinical context. As the initial biopsy results may be inconclusive or negative, MR may be used in an attempt to further characterize the lesion. In pediatric patients, MR might be preferred because it does not use ionizing radiation.
Both CT and MR can supply information needed by the clinician for optimal treatment planning in known cancers. CT has a number of important advantages. The CT studies are easier to execute and are more reproducible than MRI because of the short data acquisition time that results in less image motion degradation. MDCT systems also now offer high-quality multiplanar imaging with the image quality equal to or exceeding that of multiplanar MR images when the superiority of bone-related information on CT is factored into this comparison. The evaluation of bone on CT is superior to that on MRI. CT detects calcifications better than MRI. Also, CT is better and easier to perform and interpret than MRI with regard to the extent of metastatic adenopathy. Supplemental MRI is occasionally necessary in patients with tumors whose extent cannot be fully appreciated by a combination of the clinical examination and CECT; this occurs most often due to dental-related artifacts on initial CT studies. The MR in these cases is usually focused on clarifying specific issues that may critically alter patient management, including but not limited to1 (a) depth of invasion,2 (b) nature of an atypical mass lesion,3 and (c) presence and extent of perineural disease.
The qualities described in the previous paragraph make CT preferable for surveillance imaging including early detection of tumor recurrence and/or treatment complications such as osteoradionecrosis of the mandible. Problems such as osteonecrosis are more confidently diagnosed based on the CT pattern of disease as discussed in Chapter 21. Moreover, osteonecrosis due to radiation may mimic recurrence clinically; with MR, early bone invasion as a sign of actual tumor recurrence or persistence may go unnoticed. Recent developments in MRI, such as diffusion-weighted MRI and perfusion imaging, may increase the role of this imaging modality in cancer treatment decision making and surveillance imaging in future.2–4
FDG-PET should play a selective role but not a primary role in oral cavity cancers. It is most useful in looking for recurrence after treatment. It should not be used as a routine staging procedure. There is a limited role for sentinel node imaging in the treatment of oral cavity cancer.
If MRI, CT, or the clinical evaluation suggests a vasoformative lesion or highly vascular tumor, then angiography may be done to confirm this impression. In hypervascular lesions, endovascular therapy may be used as a definitive treatment or adjunct to surgical removal.
Trauma
CT has replaced plain films for evaluating patients at risk or with complex injuries. These studies require CT done with as near to isotropic volume acquisition as possible and multiplanar reformation viewing and archiving. Plain films may be used for confirmation of hardware placement and uncomplicated follow-up.
Controversies
Computed Tomography Versus Magnetic Resonance Imaging for Cancer Evaluation
There is some limited debate with regard to whether CT or MR should be the primary imaging tool for evaluating patients with oral cavity cancer. This discussion sometimes emphasizes which study is best at showing bone involvement. CT is better than MRI at showing all stages of bone invasion except for unusual cases of spread within the marrow cavity. In the vast majority of cases, the bone information from imaging must exclude invasion with a high degree of confidence. That anatomic imaging study must then determine the amount of invasion precisely. MRI is not optimally suited to these tasks, as discussed in Chapters 1 through 3 and 21.
The nature of oropharyngeal cancer is that the area of bone destruction as seen on CT almost always geographically corresponds to the tumor involvement of the marrow cavity of the mandible or the discrete cortical defect that is visible along the posterior maxilla or border of the hard palate. It is only under unusual circumstances that the spread of cancer within the marrow space goes beyond the zone of obvious bone destruction seen on CT; thus, supplemental MRI for mandibular marrow space spread is only very infrequently or rarely necessary. The deficiencies of MR in this regard should obviate the use this imaging as the primary diagnostic study for oropharyngeal cancer in any rational practice of head and neck radiology unless CT is done whenever the primary approaches bone as seen on MRI. This still fails to address the competitive advantage of CT in evaluating regional nodal disease.
“Routine” Use of FDG-PET in Known Cancers
The standard or “routine” use of FDG-PET in head and neck cancer remains not yet clearly evidenced based, although its use is common. FDG-PET should only be used with discernment with regard to its likelihood of contributing to medical decision making that might significantly alter the plan of therapy and/or improve patient outcome in any individual case.
NORMAL ANATOMY
General Description
The oral cavity encompasses several relatively discrete regions. These include the hard palate, floor of the mouth, buccal mucosa including the upper and lower gingivobuccal sulci, retromolar trigone, and anterior two thirds or oral portion of the tongue and lips (Figs. 190.2–190.5 and 196.1). The oral cavity leads to the oropharynx, which begins at the anterior tonsillar pillars (Fig. 190.1).
Detailed Description of Specific Areas
Lips
The lips are covered by skin externally and mucosa externally. The oral cavity part (noncutaneous/skin) of the lip begins at the vermilion or mucocutaneous junction. The orbicularis oris muscle, part of the superficial musculoaponeurotic system (SMAS) of the face, which makes up part of its substance, is innervated by the facial nerve (Figs. 78.25 and 196.2). The blood supply is the labial artery from the facial artery. The sensory nerve supply to the lower lip is via the mental nerve, a branch of the inferior alveolar nerve. The sensory nerve of the upper lip is the infraorbital branch of the maxillary nerve.
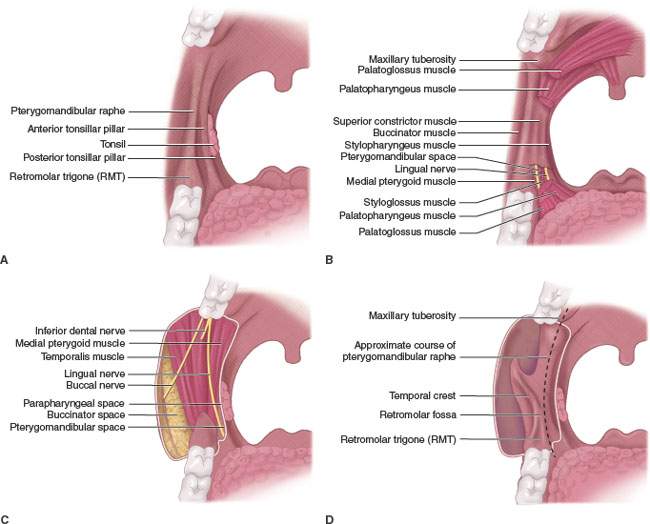
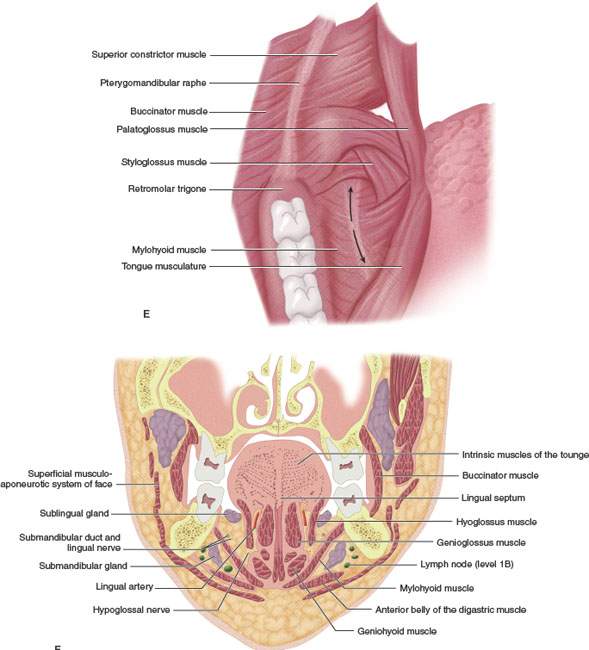
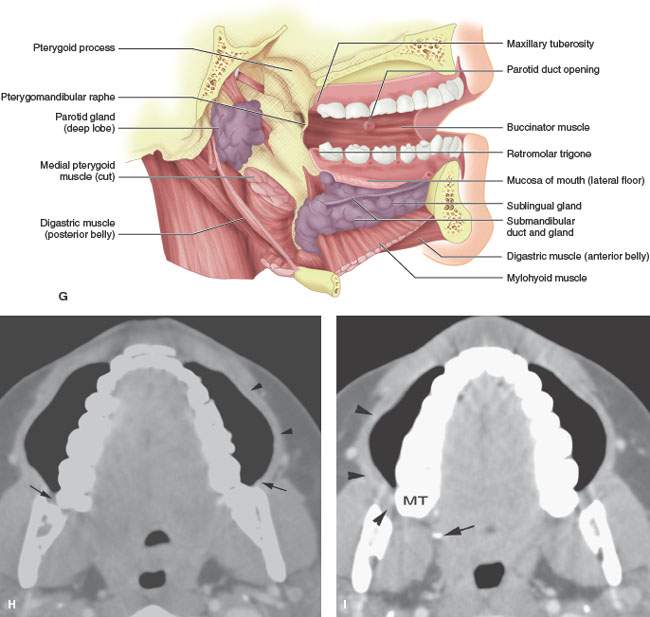
FIGURE 196.1. A series of anatomic diagrams and a computed tomography (CT) scan illustrating important anatomic relationships within the oral cavity. A–D: Diagram illustrating the superficial and deep anatomic relationships of the pterygomandibular raphe and adjacent oral cavity and oral pharyngeal structures. Note that the diagrams show progressively deeper anatomic relationships. In particular, the relationship of the retromolar trigone region to the pterygomandibular raphe and the superior relationship of that to the maxillary tuberosity are emphasized. Deeper dissections show the muscular, neural, and bony relationships of these areas. E: Anatomic diagram showing the junction of the oral cavity and the oropharynx. The transition between these two regions is bound by the pterygomandibular raphe and retromolar trigone laterally and the anterior tonsillar pillar medially. The arrows along the posterior floor of the mouth demonstrate the lingual alveolar sulcus. This zone is an important one with regard to understanding how tumors arising in either the oral cavity or oropharynx may spread from one region to another. F: Coronal anatomic diagram showing important anatomic relationships throughout the oral cavity regions illustrated subsequently by both whole organ sections and images. G: Anatomic diagram showing the relationship of the mylohyoid muscle to the surrounding major salivary gland and deeper anatomic structures of the oral cavity. H, I: Contrast-enhanced CT images made while the patient is doing a “puffed cheek” maneuver. This illustrates the attachments of the buccinator muscle (black arrowheads) to the pterygomandibular raphe (black arrows in H) as well as the upper limits of the pterygomandibular raphe as demonstrated by the maxillary tuberosity (MT) and the hamulus of the medial pterygoid plate (black arrow in I).
Buccal Mucosa
Gross Anatomy
The upper gingivobuccal sulcus is a normally collapsed recess lying between the cheek and the maxillary alveolar ridge (Figs. 190.3 and 196.2). The sulcus is covered by mucoperiosteum on its medial surface and the mucosa and submucosal tissue reflecting over the buccinator muscle. The buccinator muscle is the muscular substance of the cheek. The buccinator attaches to the posterior aspect of the maxillary alveolar ridge, to the upper medial surface of the mandibular body, and along the pterygomandibular raphe (Figs. 190.2–190.5, 196.1, and 196.2). The muscle then sweeps forward to join the orbicularis oris (part of the SMAS) at the angle of the mouth.
The lower gingivobuccal sulcus lies between the mandibular alveolar ridge and cheek. The buccinator muscle bridges the gap between the posterior maxilla and mandible lying medial to the fatty buccinator space (Figs. 190.2–190.5, 196.1, and 196.2). The parotid duct pierces the buccinator muscle from its opening on the buccal mucosa opposite the upper second molar, with the duct then coursing through the buccinator space (Figs. 175.9–175.11). The buccinator space is continuous with the retroantral fat pad within the infratemporal fossa above.
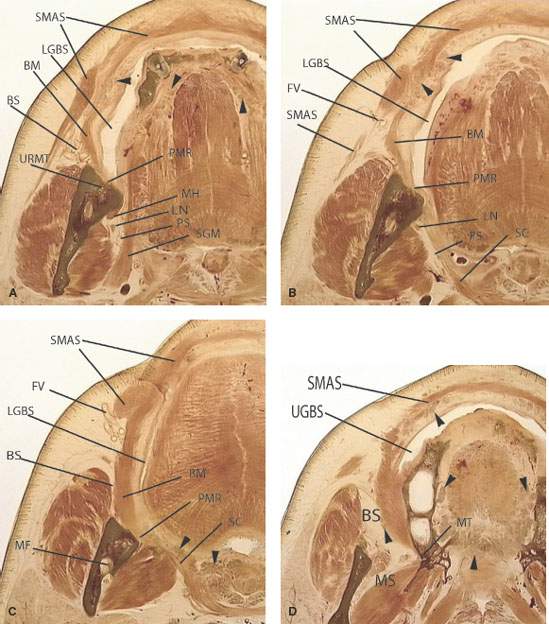
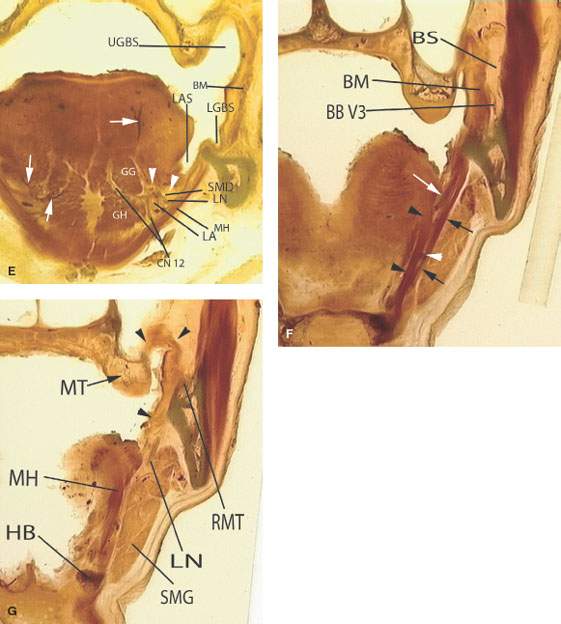
FIGURE 196.2. A series of whole organ sections demonstrating anatomic relationships of structures and regions related to the oral cavity. Abbreviations common to these illustrations are as follows: SMAS, superficial musculoaponeurotic system made up of muscles of facial expression; LGBS, lower gingivobuccal sulcus; BM, buccinator muscle; BS, buccinator space; URMT, upper retromolar trigone; PMR, pterygomandibular raphe; MH, mylohyoid muscle; LN, lingual nerve; PS, parapharyngeal space; SGM, styloglossus muscle; FV, facial vessels; SC, superior constrictor muscle; LGBS, lower gingivobuccal sulcus; MF, mandibular foramen; UGBS, upper gingivobuccal sulcus; MS, masticator space; MT, maxillary tuberosity; LAS, lingual alveolar sulcus; SMD, submandibular duct; LA, lingual artery; CN 12, hypoglossal nerve; BBV3, buccal branch of V3; RMT, retromolar trigone; HB, hyoid bone; and SMG, submandibular gland. A–D: A series of images emphasizing the relationship of the buccal mucosa and gingivobuccal sulci to the pterygomandibular raphe and surrounding bony anatomy. The attachments of the musculature in this region are important conduits of deep spread of cancer as seen in prior and subsequent chapters. The black arrowheads in these four sections point out accessory minor salivary gland tissue beneath the buccal mucosa in the lips as well as that located in the submucosa of the oral tongue, anterior tonsillar pillar, and hard and soft palate. In (D), this tissue is seen within the buccal space, and it can also be seen frequently immediately adjacent to the retromolar trigone. E–G: A series of whole organ sections that should be correlated with the anatomic diagram in Figure 196.1F. These coronal images demonstrate the important relationships of the mylohyoid muscle to surrounding structures and in particular its importance as a boundary between the floor of the mouth (FOM) and submandibular space. In (E), the white arrows demonstrate branches of the lingual vessels distributed throughout the FOM and oral tongue. In (F), the hyoglossus muscle (arrowheads) and mylohyoid muscle (black arrows) create compartments within the FOM that house, among other neurovascular structures, the lingual nerve (white arrow) and the hypoglossal nerve (white arrowhead). In (G), the line of attachment of the buccinator muscle and pterygomandibular raphe extending from the posterior edge of the mylohyoid muscle to the region of the maxillary tuberosity can be appreciated (black arrowheads).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








