, Brian M. Trotta2, Mark J. Jameson3, Max Wintermark4 and Prashant Raghavan5
(1)
Division of Neuroradiology, Department of Radiology and Medical Imaging, University of Virginia Health System, Charlottesville, VA, USA
(2)
Coastal Radiology Associates, PLLC, New Bern, NC, USA
(3)
Division of Head and Neck Surgical Oncology, Department of Otolaryngology – Head and Neck Surgery, University of Virginia Health System, Charlottesville, VA, USA
(4)
Department of Radiology and Medical Imaging, University of Virginia Health System, Charlottesville, VA, USA
(5)
Division of Neuroradiology, Department of Diagnostic Radiology and Nuclear Medicine, University of Maryland School of Medicine, Baltimore, MD, USA
Abstract
Squamous cell carcinomas (SCCs) represent the vast majority of lesions in the oral cavity and oropharynx (OC/OP). The imaging appearance of these cancers and their common pathways of spread are the focus of this chapter, and a few of the other lesions of the OC/OP are reviewed.
4.1 Introduction
Squamous cell carcinomas (SCCs) represent the vast majority of lesions in the oral cavity and oropharynx (OC/OP). The imaging appearance of these cancers and their common pathways of spread are the focus of this chapter, and a few of the other lesions of the OC/OP are reviewed.
4.2 Anatomy
The oral cavity is separated from the sinonasal region by the hard and soft palate and from the oropharynx by the circumvallate papilla of the tongue, soft palate, and anterior tonsillar pillars (Fig. 4.1). The maxillary tuberosity serves as the radiographic border between the oral cavity and oropharynx.
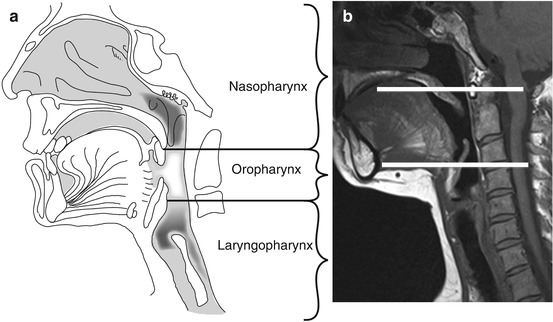
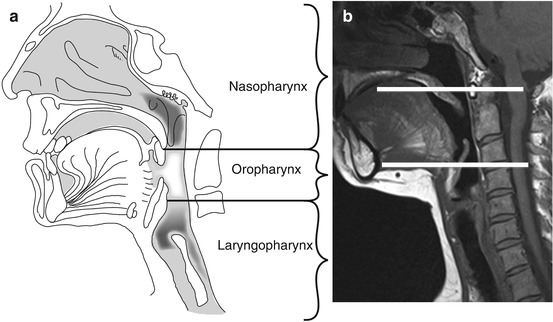
Fig. 4.1
Sagittal graphic (a) showing the anatomical landmarks of the oropharynx in between the nasopharynx and laryngopharynx. The oropharynx lies. It is the area in between the hard/soft palate and the pharyngo-epiglottic folds at the level of the inferior epiglottis, marked by the two horizontal white lines on the sagittal MR image (b)
From an imaging standpoint, the oral cavity can be subdivided into four distinct regions: (1) the oral mucosal surface, including the floor of mouth; (2) the root of the tongue; (3) the sublingual space; and (4) the submandibular space (Fig. 4.2). All the surfaces of the oral cavity structures are covered with keratinizing stratified squamous epithelium along with minor salivary gland rests.
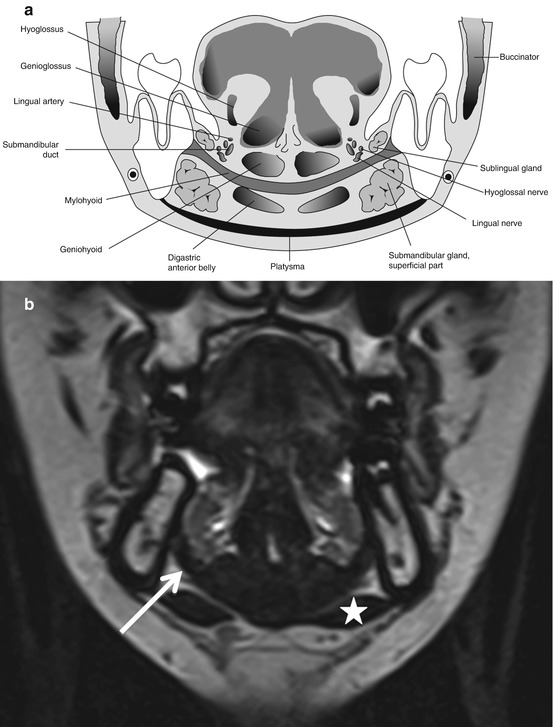
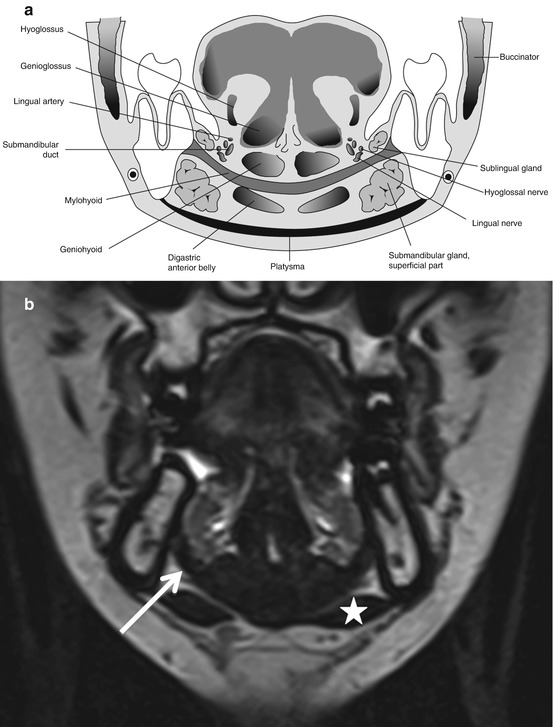
Fig. 4.2
Coronal graphic (a) shows the relationship of the sublingual and the submandibular spaces with the mylohyoid muscle. Also note the neurovascular pedicle (consisting of lingual artery and vein, lingual nerve) within the sublingual space. The hypoglossal nerve courses both in the posterior submandibular and sublingual spaces and runs along the surface of hyoglossus muscle before terminating within the tongue. Coronal MR (b) shows the mylohyoid muscle as a dark curvilinear sling (arrow)-like structure separating the upper sublingual and the inferior submandibular spaces. Also note the paired anterior belly of digastric below the mylohyoid (star)
The tongue is divided into an oral part (anterior two-thirds within the oral cavity), the base (posterior one-third within the oropharynx), and the root. The circumvallate papilla of the tongue separates the oral tongue from the base of tongue, which also includes the lingual tonsils. The tongue consists of extrinsic muscles (genioglossus, hyoglossus, styloglossus, and palatoglossus), which predominantly move the tongue body, and the intrinsic muscles (superior and inferior longitudinal, transverse, and vertical muscles), which alter tongue shape during swallowing and speech. The root of the tongue consists of the genioglossus-geniohyoid complex and the lingual septum; it extends from the extrinsic tongue muscles superiorly to the mylohyoid sling inferiorly (Fig. 4.3). The vasculature of the tongue consists of the lingual artery (second branch of external carotid) and corresponding lingual vein within the sublingual space. The hypoglossal nerve provides the motor supply and enters the sublingual space just lateral to the posterior hyoglossus. Sensory supply for the anterior two-thirds is by the lingual nerve, while the posterior one-thirds is supplied by branches from glossopharyngeal nerve (CN IX). The chorda tympani nerve, a branch from the facial nerve (CN VII), carries the taste fibers from the anterior two-thirds within the lingual nerve. All these run in the sublingual space (Fig. 4.2).
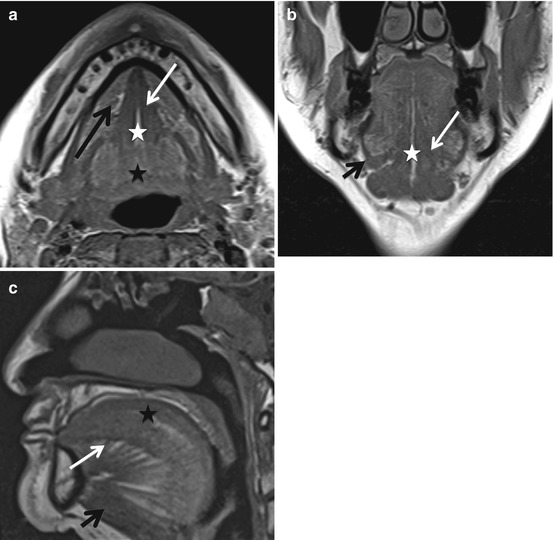
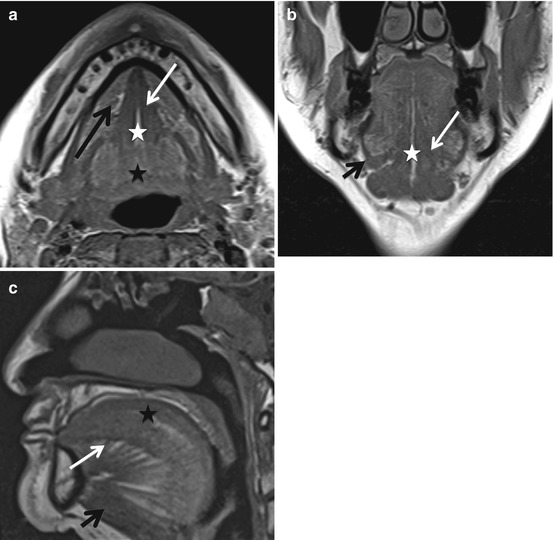
Fig. 4.3
Tongue anatomy is elegantly identified on MR images. On axial T1 (a), the lingual septum (with linear T1 hyperintense fat within it) (white star), the adjacent genioglossus muscles (white arrow), and the intrinsic muscles (black star) which are posterior to it. Also note the sublingual spaces lateral to the genioglossus (long black arrow). Coronal T1 (b) images also show the lingual septum (white star), genioglossus as well as the mylohyoid (short black arrow). Finally, sagittal T1 (c) images show the characteristic fan-like shape of the genioglossus (white arrow) along with the geniohyoid and mylohyoid muscles inferiorly (short black arrow). The intrinsic tongue muscles are superior to the genioglossus on this sagittal image
The floor of the mouth includes the mylohyoid muscle, the hyoglossus muscle, and the sublingual space, which is located between these two muscles (Fig. 4.2). The sublingual space is a horizontal horseshoe-shaped space deep to the oral tongue that communicates posteriorly within the submandibular space and the inferior parapharyngeal space. It lies in between the mylohyoid muscle inferolaterally and the genioglossus muscle medially. The contents of the sublingual space include the lingual artery and vein, distal segments of CNs IX and X, the lingual nerve containing sensory fibers from CN V3 (mandibular branch of trigeminal) as well as taste fibers through the chorda tympani from CN VII (facial), the sublingual gland and ducts, the deep portion of the submandibular gland, and the submandibular duct.
The submandibular space is a vertical horseshoe-shaped space, inferolateral to the mylohyoid muscle and superior to the hyoid bone. It communicates both with the inferior parapharyngeal space and the posterior aspect of the sublingual space. The submandibular space contains the larger superficial portion of the submandibular gland, anterior belly of the digastric, the facial vein and artery, the inferior loop of the hypoglossal nerve (CN XII), and the submental and submandibular lymph node groups (Fig. 4.2).
The oropharynx includes the posterior third of tongue (base of tongue), the vallecula, the palatine tonsils and tonsillar fossa, the soft palate, the uvula, and the posterior and lateral pharyngeal walls from the soft palate superiorly to the pharyngo-epiglottic folds inferiorly (Fig. 4.1).
Regional nodal metastasis from oral cavity and base of tongue cancers commonly occurs to the submental, submandibular, and upper and mid-cervical lymph chains (levels I–III); for tonsil and pharyngeal wall cancers, regional metastases rarely involve level I.
4.3 Squamous Cell Carcinoma
The most commonly recognized risk factors for SCCs in the head and neck include long-term overuse of alcohol and tobacco. Recently, human papillomavirus (HPV) has been shown to be responsible for the majority of new oropharyngeal SCCs, with HPV-16 accounting for 90–95 % of such cases. Radiologists should be aware of a unique presentation of HPV-associated oropharyngeal cancers, which have an increased tendency to present with large cystic/necrotic level IIa nodal metastases. Given that they have a tendency to occur in younger nonsmokers, these can easily be misinterpreted as second branchial cleft cysts, resulting in missed diagnosis and/or delayed treatment (Fig. 4.4). While second branchial cleft cysts also present as level IIa cystic lesions, they typically present in the first two decades and, unless infected, appear smooth, well circumscribed, and unilocular without any stranding of surrounding structures and without thick or nodular walls. Thus, the presence of an underlying head and neck primary cancer should always be excluded in a young adult with a newly diagnosed level II neck mass.
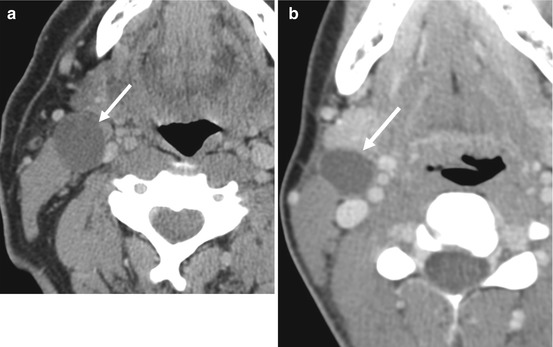
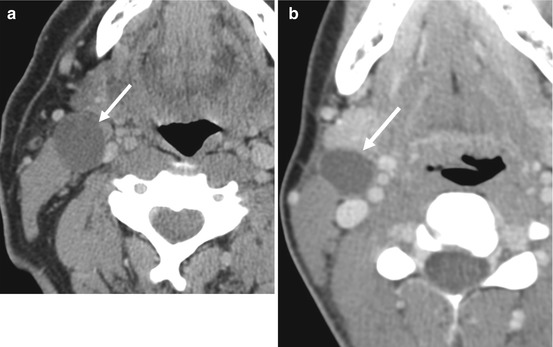
Fig. 4.4
Axial contrast-enhanced CT images from two different patients demonstrate an enlarged fluid density cystic lymph node in a patient with known tonsillar SCC and (arrow in a) a thin-walled fluid density lesion in the same location in a different patient (arrow in b) which was found to represent a type II branchial cleft cyst
4.3.1 Radiographic Staging
As with other head and neck SCCs, OC/OP SCCs are staged using the TNM classification system (Boxes 4.1a and 4.1b). Although much of the staging is accomplished by clinical exam and endoscopy, final staging is heavily dependent upon cross-sectional imaging. Issues of key importance to staging that are clarified or determined by imaging include extent of the primary lesion, invasion of nearby bone, neural and/or vascular involvement, and cervical nodal status, including subclinical cervical nodal metastases and extracapsular spread (ECS) beyond involved nodes. In this process, it is crucial to note involvement of structures that raise concern for resectability (e.g., carotid encasement, pterygoid involvement, skull-base involvement).
Box 4.1a. TNM Classification of Squamous Cell Carcinomas of the Oral Cavity and Oropharynxa
Disease category | Defining characteristics |
|---|---|
Primary tumor of oral cavity | |
Tx | Primary tumor cannot be assessed |
T0 | No evidence of primary tumor is seen |
Tis | Primary tumor is carcinoma in situ |
T1 | Primary carcinoma has a maximal diameter of 2 cm or less |
T2 | Primary carcinoma has a maximal diameter of 2–4 cm |
T3 | Primary carcinoma has a maximal diameter of more than 4 cm |
T4a | |
Lip | Primary tumor invades through cortical bone or involves inferior alveolar nerve, floor of mouth, skin of chin or nose |
Oral cavity | Primary tumor invades through cortical bone or involves extrinsic tongue muscles, maxillary sinus, skin of face |
T4b | Primary tumor involves masticator space, pterygoid plates, skull base, internal carotid artery |
Primary tumor of oropharynx | |
Tx | Primary tumor cannot be assessed |
T0 | No evidence of primary tumor is seen |
T1 | Primary carcinoma has a maximal diameter of 2 cm or less |
T2 | Primary carcinoma has a maximal diameter of 2–4 cm |
T3 | Primary carcinoma has a maximal diameter of more than 4 cm |
T4a | Primary tumor involves the larynx, extrinsic muscles of the tongue, medial pterygoid, hard palate, or mandible |
T4b | Primary tumor involves the lateral pterygoid muscle, pterygoid plates, lateral nasopharynx, skull base, carotid artery |
Box 4.1b. Oral Cavity and Oropharyngeal Squamous Cell Carcinoma Stage Grouping Based on TNM Classification
Cancer stage | T category | N category | M category |
|---|---|---|---|
0 | Tis | N0 | M0 |
I | T1 | N0 | M0 |
II | T2 | N0 | M0 |
III | T3 | N0 | M0 |
III | T1 to T3 | N1 | M0 |
IVA | T4a | N0 or N1 | M0 |
T1 to T4a | N2 | M0 | |
IVB | T4b | Any N | M0 |
Any T | N3 | M0 | |
IVC | Any T | Any N | M1 |
4.3.2 Routes of Spread
The general routes of spread of OC/OP SCC are the same for all subsites: (a) direct extension over mucosal surfaces, muscle, and bone; (b) lymphatic drainage pathways; and (c) extension along neurovascular bundles. However, the particular subsite of involvement of the oral cavity or oropharynx may dictate routine assessment of certain anatomic structures. The relevant imaging anatomy and the patterns of spread for each primary site are summarized in the Boxes 4.2a and 4.2b.
Evaluation of direct extension is most effectively accomplished by direct visualization, particularly in the case of superficial lesions, but the overall extent of the a tumor is often underestimated by physical examination due to submucosal extension or direct invasion of adjacent structures. The radiologist report should describe in detail the entire extent of the tumor and address all the issues relevant to treatment planning.
Box 4.2a. Oral Cavity Subsites
Oral cavitysubsite | Imaging anatomy | Imaging patterns of tumor spread |
|---|---|---|
Lip | Most often arises along vermilion border | Laterally: Involvement of skin |
Only infiltrative lesions require imaging | Deep: Involvement of orbicularis oris muscle or osseous involvement of buccal surface of maxillary or mandibular ridge | |
Lymphatics: Primarily level I and II lymph nodes | ||
Buccal mucosaand gingiva | Buccal mucosa covers lips and cheeks and is continuous with the buccal aspect of the gingiva of the maxillary and mandibular alveolar ridge | Superficial spread most common along buccinator muscle |
Most commonly occurs on lateral walls | Deep: Osseous involvement of maxilla or mandible | |
Continuous with retromolar trigone | Posteriorly: To retromolar trigone and pterygomandibular raphe (see below) | |
Superiorly: Paranasal sinuses | ||
Lymphatics: Primarily level I and II lymph nodes | ||
Retromolartrigone | Triangular-shaped mucosa behind last mandibular molar | Anteriorly: Along alveolar ridge |
Either primary site of SCCA or secondarily involved | Posteriorly: Along masticator space, mandibular ramus, and perineural spread along V3 | |
Pterygomandibular raphe – fascial band extending from posterior mylohyoid ridge to medial pterygoid hamulus | Superiorly: Along pterygomandibular raphe to medial pterygoid plate | |
Provides pathway for tumor spread between buccal, masticator space, and floor of mouth. | Inferiorly: Along pterygomandibular raphe and mylohyoid ridge and muscle. Also osseous involvement of mandible and perineural spread along inferior alveolar nerve | |
Medial pterygoid involvement is heralded clinically by trismus | ||
Floor of themouth | Crescent-shaped mucosa supported by the mylohyoid, which separates it from the submandibular space | Inferior: Along mylohyoid muscle or along neurovascular bundles |
Divided in half by the lingual frenulum | Anterior and lateral: To gingiva and mandible. Assess for crossing of midline | |
Posterior border is tongue and anterior tonsillar pillars | Posteriorly: Along hyoglossus muscle | |
Lymphatics: Primarily levels I and II lymph nodes can be bilateral for lesions approaching midline | ||
Oral tongue | Consists of anterior and middle thirds of tongue | Laterally: Along gingiva and mandible. Assess for crossing of midline |
Mostly occur along lateral and ventral surfaces | Inferiorly: Along floor of mouth, intrinsic and extrinsic muscles of the tongue and along neurovascular bundles | |
Posteriorly: Along base of tongue and intrinsic/extrinsic muscles of the tongue | ||
Lymphatics: Primarily levels I and II but regional spread to levels III and IV can occur without involvement of higher levels | ||
Hard palate | Primary SCC of the hard palate is rare | Lateral: Maxillary alveolar ridge |
Most commonly represents direct extension | Superiorly: Into nasal cavity and maxillary sinuses. Perineural spread along greater and lesser palatine nerves which provide pathway to pterygopalatine fossa |
Box 4.2b. Oropharyngeal Subsites
Oropharynxsubsite | Imaging anatomy | Imaging patterns of tumor spread |
|---|---|---|
Base ofthe tongue | Extends from circumvallate papillae anteriorly to the vallecula inferiorly | Laterally: Along tonsillar pillars. Assess for crossing of midline |
Anteriorly: To the sublingual space and oral tongue | ||
Posteriorly/Inferiorly: Along intrinsic muscles of the tongue. Under valleculae and into preepiglottic space | ||
Lymphatics: Primarily to level II, III, and IV, tongue base has bilateral nodal drainage | ||
Tonsils | Anterior and posterior tonsillar pillars or palatine tonsils | Superiorly: Along palatoglossus muscle to hard and soft palates. Along tensor and levator palatini muscles and pterygoid muscles. Invasion of nasopharynx and skull base |
Most arise in anterior tonsillar pillar | Anteriorly: Along superior constrictor muscles to pterygomandibular raphe (may then involve skull base) |