ORAL CAVITY: DEVELOPMENTAL ABNORMALITIES
KEY POINTS
- Imaging typically will make a precise diagnosis in developmental abnormalities of the oral cavity.
- Imaging will significantly affect medical decision making in these developmental conditions.
- Computed tomography and magnetic resonance imaging are typically the main and frequently the only studies required.
- Ultrasound may be sufficient in the evaluation of simple abnormalities such as a noncomplicated thyroglossal cyst. However, in more complex problems, it will not provide information definitive enough for medical decision making.
The most common developmental abnormality that affects the oral cavity and presents for imaging evaluation is likely a vascular malformation, typically those of the low-flow, venolymphatic variety. Other anomalies that present in or around the oral cavity generally arise or present in the sublingual and submandibular spaces and occasionally the upper neck. This chapter will summarize the diagnostic possibilities since these anomalies have been discussed in chapters about other anatomic sites. Those chapters may be referenced as necessary for more detail. Those chapters cover the natural history and imaging appearance of those anomalies.
As pathologic entities, these are discussed and presented in the following chapters and figure:
- Vascular abnormalities (Chapter 9)
- Epidermoids, dermoids, and related abnormalities (Fig. 8.3 and Chapter 8)
- Thyroglossal duct abnormalities (Chapter 170)
With regard to sites of origin, these are presented and discussed in the following figures and chapters:
- Submandibular space (Figs. 180.1–180.3 and Chapter 180)
- Sublingual space (Figs. 183.11 and 183.12 and Chapter 183)
One can also consider syndromic neurogenic (Fig. 183.13) and mandibular tumors as developmental; however, in this text, they are considered primarily in conjunction with benign neoplasms.
In general, developmental abnormalities present during childhood. Some manifest in infancy; however, the presentation is often delayed until sometime beyond infancy into the early adult years, second and third decades, and even into adult middle age. If they grow, it tends to be at the same rate of normal structures, including a rapid growth phase at times of accelerated growth of the individual—for instance, in adolescence. Some, such as hamartomas, tend to grow at the same rate as normal structures. Some, such as high-flow vascular malformations, have internal physiologic dynamics that will allow them to enlarge more rapidly than normal tissues rather than truly proliferate. Truly neoplastic conditions such as teratomas or proliferative hemangioma (Chapters 8 and 9) will manifest growth out of proportion to normal structures.
Developmental abnormalities are frequently discovered incidentally on imaging studies done for other purposes. Some developmental conditions present as masses or because they interfere with function. In the oral cavity, these would typically manifest as speech or chewing difficulties. If originating from the floor of the mouth or tongue, swallowing may be affected and that might manifest as poor feeding in an infant. They are typically not painful unless there is some complicating factor present. Developmental abnormalities may also become manifest because of complicating factors such as infection in a developmental cyst that connects to the oral cavity; bleeding, thrombosis, or infection of a vascular malformation; or tumor arising in benign ectopic tissue such as an adenoma or carcinoma in lingual thyroid tissue that may involve the floor of the mouth.
ANATOMIC AND DEVELOPMENTAL CONSIDERATIONS
Embryology
The embryology of the developmental conditions that affect the oral cavity as presented in the introduction is summarized in the dedicated chapters on those conditions.
Applied Anatomy
A thorough knowledge of oral cavity anatomy and anatomic variations in each of the following areas is required for the evaluation of developmental conditions of the oral cavity. This anatomy is presented in detail with the introductory material on the oral cavity (Chapter 196), oropharynx (Chapter 190), and related spaces of the neck (Chapters 142 and 149).
IMAGING APPROACH
Techniques and Relevant Aspects
The oral cavity is specifically studied in essentially the same manner for benign masses of known or uncertain etiology as it is for the evaluation of known or suspected oral cavity cancer. The principles of using these studies are reviewed in Chapter 190. Specific problem-driven protocols for computed tomography (CT) and magnetic resonance imaging (MRI) of the oropharynx are presented in Appendixes A and B, respectively.
Ultrasound may be sufficient in the evaluation of small, well-defined lesions but is often insufficient in defining the anatomic extent of larger lesions. However, it may provide useful information on the degree of vascularity of a lesion.
There is a limited role for catheter angiography in lesions where the physical examination and imaging with CT angiography and/or MRI suggests that they are vascular in origin or very hypervascular.
Radionuclide studies are generally not useful in these conditions except to confirm the presence of ectopic thyroid tissue and then confirm whether that ectopic tissue is the only functioning thyroid tissue present.
Pros and Cons
In general, these anomalies occur in younger age groups, so it is best to avoid radiation if possible. On the other hand, definitive MRI in children may require general anesthesia. These relative risks must be balanced. Either MRI or CT is usually definitive in the anatomic evaluation of these anomalies of development. One or the other may be more specific in some circumstances. MRI is more likely to be motion degraded.
Potentially developmental lesions that present as infections are better evaluated by CT. Such imaging is also more likely to show calcifications, if this is important for the differential diagnosis. MRI provides a better map of venolymphatic malformations and can especially help to determine if they involve the dental arches—an occurrence that can lead to unfortunate consequences during routine dental work if it goes unnoticed (Fig. 197.1). MRI might also help to characterize cystic masses with diffusion-weighted imaging.
There really is no generally correct or incorrect choice in this matter. The decision of which imaging study to use should be individualized based on age, likelihood of the correct diagnosis already being known from clinical information, availability of imaging equipment, and other factors just discussed.
Controversies
It might be argued that ultrasound should be used in the evaluation of these problems. It is frequently not definitive and cost additive, so its use in general seems unjustified. If it can obviate other more risky studies and provide all information necessary for medical decision making, then it would be of obvious benefit in such an unusual circumstance.
SPECIFIC DISEASE/CONDITION
Dermoids, Epidermoids, Teratomas, and Other Developmental Cystic and Related Abnormalities
Etiology
Dermoids, epidermoids, teratomas, and other cystic and related abnormalities tend to be spontaneous and developmental, and only uncommonly arise in or affect the oral cavity (Chapter 8). Oral cavity dermoids and epidermoids may occur as an extension from those originating in the submandibular space. They also originate above the mylohyoid in the sublingual and other unnamed floor of the mouth spaces (Fig. 197.2).
Branchial apparatus cysts will only rarely encroach on structures near the junction of the oral cavity and oropharynx, so they are not really a practical consideration in this region. Duplication cysts are very rare but will involve the oral tongue and floor of the mouth (Fig. 197.3).
Clinical Presentation
These anomalies will usually present as a palpable mass or become apparent because they interfere with chewing, swallowing, or speech in an adult, and feeding or the airway in an infant. Teratomas may be detected by prenatal ultrasound but eventually will be discovered at birth and can cause breathing as well as feeding problems.
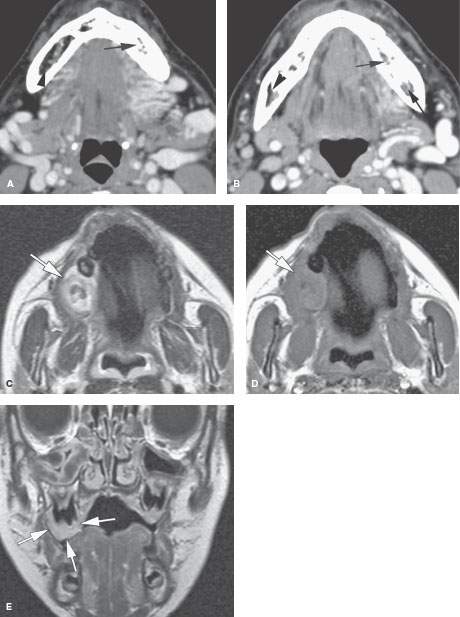
FIGURE 197.1. Two patients with vascular malformations that could result in excessive bleeding if a dental procedure were done without knowledge of the malformations involving the jaws. A, B: Patient 1. Contrast-enhanced computed tomography of a high-flow vascular malformation of the floor of the mouth and suprahyoid neck. Both images show the large inflow and outflow vessels. Both also show likely abnormal flow within the marrow space of the mandible with loss of normally fatty marrow space on the left (arrows) compared to the right (arrowheads). C–E: Patient 2. A 5-year-old child presenting with an easily bleeding maxillary gingival lesion. The lesion (arrow) appears relatively hyperintense on the T2-weighted magnetic resonance image (C). Axial T1-weighted images, before (D) and after (E) injection of gadolinium show pronounced, homogeneous enhancement (arrow). On the gadolinium-enhanced T1-weighted coronal image, the lesion (arrows) can be seen to cover an underlying tooth. The findings are compatible with a slow-flow vascular malformation. The lesion was resected, and histologic examination confirmed this diagnosis.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








