ORAL CAVITY: INFECTIOUS AND NONINFECTIOUS INFLAMMATORY CONDITIONS
KEY POINTS
- Imaging, especially computed tomography, is often useful in the management of acute pyogenic oral cavity infections.
- Computed tomography can provide a safe and rapid assessment of the airway in a patient who is stable and under the control of the treating physician for airway management decisions.
- Imaging in noninfectious inflammatory diseases is generally nonspecific for diagnostic purposes.
- Atypical clinical and imaging features of oral cavity pathology should raise the possibility of an inflammatory process.
- Relatively few people undergo imaging for this latter group of diseases.
The pathophysiology of the infections discussed in Chapters 13 through 16 and other inflammatory disease discussed in Chapters 17 through 20 as expressed on imaging studies is presented in detail in their respective chapters.
Most of the disease processes discussed in this chapter are held in common between the oral cavity, mandible and maxilla (especially with regard to dental infections), oropharynx, and submandibular and sublingual glands and spaces. This chapter will summarize in illustrative and text material those disease processes that have been discussed and illustrated more completely in previous chapters, namely:
- Mandibular and dental inflammatory diseases (Chapter 97)
- Oropharyngeal inflammatory diseases (Chapter 192)
- Submandibular space inflammatory diseases (Chapter 181)
- Sublingual space inflammatory diseases (Chapter 183)
Those chapters should be used as the main source of case material for the diseases presented in this chapter.
After physical examination, it may be difficult to decide whether an area of oral cavity swelling is inflammatory or infectious as opposed to neoplastic; however, the clinical presentation will often be very clear, especially in the case of acute pyogenic infections. In low-grade inflammatory processes, this distinction might remain unclear even after biopsy, so watchful waiting might become the default strategy, sometimes with imaging surveillance as an aid.
Much inflammatory swelling in the oral cavity will have a nonspecific imaging appearance when considered independent of the clinical setting. However, taken with clinical setting, the findings are often specific enough to confirm the etiology suspected clinically. Computed tomography (CT) and occasionally magnetic resonance imaging (MRI) are then used for their primary function of mapping the extent of the most commonly pyogenic, infectious inflammatory process.
For simplicity, this chapter is divided in two main sections: one dealing with infections and one with the much less common noninfectious inflammatory conditions.
ANATOMIC AND DEVELOPMENTAL CONSIDERATIONS
Embryology
Rarely, a developmental lesion such as a thyroglossal duct cyst (Chapter 170), epidermoid cyst (Chapter 8), or very rare duplication cyst will become infected and present as a primary oropharyngeal infection (Fig. 192.2). The embryology of those types of anomalies is discussed in the mentioned chapters and elsewhere.
Applied Anatomy
The critical anatomic knowledge necessary for the evaluation of inflammatory oral cavity processes is summarized here. The detailed anatomy of this region and the adjacent oropharynx and nasopharynx and related deep tissue spaces are reviewed in chapters indicated below. A detailed working knowledge of all of this anatomy is necessary to evaluate images of patients with known or suspected oral cavity infections and other inflammatory processes if the evaluation of the images is expected to contribute measurably to medical decision making.
The general anatomic knowledge necessary to evaluate infection and other inflammation of the oral cavity includes the following:
- Regional anatomy of the oral cavity, including the floor of the mouth, oral tongue, buccal mucosa, and related deep spaces (Chapters 142 and 190)
- Related regional anatomy of the structures adjacent to the oral cavity, including the oropharynx (Chapter 190) and nasopharynx (Chapter 184)
- Bony anatomy, including the hard palate, pterygoid plates, mandible, and maxilla (Chapter 196)
IMAGING APPROACH
Techniques and Relevant Aspects
Computed Tomography and Magnetic Resonance Imaging
Inflammatory conditions of the oral cavity are studied with CT and MRI in essentially the same manner as the benign and malignant oral cavity tumors, except the entire neck may not be included. The specifics and relative value of using these studies in this anatomic region are reviewed in Chapter 190. Problem-driven protocols for CT and MRI are presented in Appendixes A and B. In general, CT is more definitive than magnetic resonance (MR) in the evaluation of the oral cavity and deep space pyogenic infectious processes. A highly detailed study of the mandible (Chapter 96) and sometimes the maxilla may have to be included.
Other
Ultrasound may be used to show oral tongue and floor of the mouth soft tissue abnormalities, but it is very limited in the evaluation of mandibular abnormalities. Radionuclide studies used to evaluate infectious disease (Chapter 5) have limited diagnostic use in the evaluation of oral cavity conditions but may be used occasionally to monitor the response to therapy of a chronic infection. The normal anatomic variations in this region seen on fluorine-18 2-fluoro-2-deoxy-D-glucose positron emission tomography (FDG-PET) studies and its lack of specificity significantly limit any potential diagnostic value of that study.
Pros and Cons
Infections in this area may involve or arise in bone, predominantly the mandible; thus, CT becomes immediately preferable to MR. A patient might be very uncomfortable due to pain and unable to limit jaw motion, and MRI will be motion degraded. A definitive CT study providing all necessary information can be accomplished in about 5 to 10 minutes, making it a more sensible first choice. MRI can be used for problem solving, such as in chronic conditions where it might help in choosing the most productive biopsy site when it is difficult to differentiate tumor from a chronic inflammatory process.
SPECIFIC DISEASE/CONDITION
Acute and Subacute Pyogenic Bacterial Infections, Viral Infections, and Chronic Infections
Etiology
The vast majority of infections of the oral cavity that come to imaging are acute or subacute pyogenic bacterial infections, with these being mainly due to dental infections complicated by abscess formation (Chapter 97) and a few due to extension of pharyngeal infections (Chapter 192). Actinomycosis infection will most commonly be an extension of a periapical tooth infection. Fungal infection may come from the mandible as well. Some sporadic and relatively rare infections due to fungi may present in the oropharynx, usually from a site of origin in the jaw. Syphilis may cause an atrophic glossitis, and a mucosal gumma can mimic tumor until it is biopsied.
Viral infections are usually not so severe that they clinically mimic pyogenic infection enough to trigger imaging with CT or MRI. Epstein-Barr virus infection, including posttransplant lymphoproliferative disease (PTLD), may mimic lymphoma, and the related adenopathy may trigger imaging.
Prevalence and Epidemiology
Pyogenic bacterial infections occur sporadically, primarily in the pediatric and young adult populations. In the older age group, diabetes, especially when poorly controlled, is a predisposing factor. Human immunodeficiency virus and other immune-compromising conditions will predispose to fungal infections and tuberculosis.
Clinical Presentation
In infants, acute and subacute bacterial infections will present with fever and poor feeding and possibly lymphadenopathy. In older children and adults, these infections will cause fever, usually a very intense pain, altered speech and swallowing, and sometimes lymphadenopathy. In the more indolent infections and in immune-compromised patients, there may be little if any fever and local symptoms may be less prevalent.
Pathophysiology and Patterns of Disease
The morphology of infectious and inflammatory disease and related bone and vascular complications are discussed in detail in Chapters 13 through 16.
Manifestations and Findings
Plain Film
Plain films may show mandibular erosion, extraluminal gas, or secondary pharyngeal swelling. Such study may rarely reveal an otherwise unsuspected causative radiodense foreign body or a submandibular stone causing sialoadenitis that is mimicking disease of oral cavity origin. In general, this is a superfluous first step in a patient who requires a definitive imaging evaluation.
Computed Tomography
Contrast-enhanced CT will show a pyogenic process that has a typical cellulitis pattern, and it may show an associated contained or spreading abscess (Chapter 13). CT should almost always be able to differentiate “drainable” from “nondrainable” infectious processes. MRI may not always be able to differentiate drainable from nondrainable infectious processes. These findings will often have spread into the deep tissue planes around the oral cavity and adjacent regions.
Bone erosion (Chapter 14) and vascular complications (Chapter 15) may be present. Cortical bone erosion may not be as evident on MR compared to CT. More indolent infections may show a similar morphology but are less likely to show frank abscess cavities (Chapter 16). Most of these infections will enhance more than muscle. They replace fat and may spread along paths of least resistance. It is important to understand the differentiating features of the following conditions in this category:
- Subperiosteal mandibular and maxillary abscess (Fig. 198.1)
- Sublingual and submandibular gland/space abscess (Fig. 198.2)
- Spreading anaerobic necrotizing infection (Figs. 192.10 and 198.2C-E)
- Infection in the parapharyngeal space (Fig. 192.10)
- Infected developmental cyst (Fig. 192.2)
The details of how these conditions spread and tend to generally appear on contrast-enhanced CT and contrast-enhanced MR are discussed in Chapters 13 through 16.
Ultrasound
Ultrasound can be used to show the presence of an abscess collection in the oral cavity. However, its use in oral cavity infections is limited, as spread of disease to the surrounding structures, including the deep spaces of the neck, is difficult or impossible to evaluate on ultrasound and does not provide a thorough evaluation of the bone structures.
Differential Diagnosis
From Clinical Data
Differentiation is primarily from pharyngeal and salivary gland infections and inflammatory diseases on the basis of the clinical presentation and physical findings. Sometimes an infection will be diagnosed based on the response to a previous course of antibiotics. An infected or inflamed tumor might be obvious as a cause at physical examination rather than an isolated infectious process.
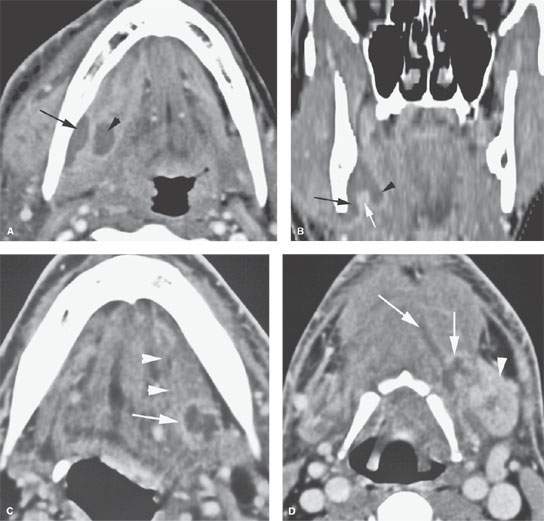

FIGURE 198.1. Three patients with purulent infections of the oral cavity of uncertain origin. In Patient 1, the source of the acute infection was suspected as dental, but in Patient 2, the source of a chronic infection was uncertain. In Patient 3, it was uncertain whether a likely dental abscess had spread to the floor of the mouth. A, B: Patient 1. In (A), there is a subperiosteal abscess (arrow) spreading along the mandible to the posterior aspect of the sublingual space (arrowhead). In (B), the coronal section shows how the subperiosteal component adjacent to the mandible (black arrow) communicates with the sublingual space (arrowhead) by way of its mylohyoid muscle (white arrow) attachment. C–E: Patient 2. Contrast-enhanced computed tomography (CT) study showing a localized abscess at the posterior edge of the mylohyoid muscle in the floor of the mouth (arrow) with associated edema spreading anteriorly in the sublingual space (arrowheads). In (D), tracts of pus spread within the spaces deep to the floor of the mouth (arrows) and are producing some obstruction of the left submandibular gland with secondary sialoadenitis. (NOTE: Clinically, it was uncertain whether this infection was primarily in the floor of the mouth or of salivary gland origin.) In (E), bone windows show an area of chronic bone infection that produced this abscess and other secondary changes, with the CT study allowing the differentiation of a chronic dental-related abscess from disease primarily within the sublingual gland or submandibular gland. F: Patient 3 shows a dental subperiosteal abscess (arrow) producing secondary reactive sialoadenitis in the sublingual gland (arrowheads). This study clearly defines that the drainable collection is limited to this subperiosteal space and does not involve the sublingual space and floor of the mouth.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








