ORBIT: BLUNT FORCE, FRACTURES, AND PENETRATING INJURIES
KEY POINTS
- The imaging findings in orbital trauma are critical to treatment decisions, including precise surgical planning.
- Imaging can identify findings that are critical to the prognosis.
- Imaging can may help detect important complications such as infection or retained foreign bodies.
Blunt force and penetrating trauma may result in both soft tissue and bony injury. This chapter describes common patterns of orbital fractures. It also discusses the effects of penetrating trauma and the evaluation of possibly retained orbital foreign bodies. Such ocular injures are discussed in Chapter 51. Optic nerve/sheath trauma is discussed in Chapter 54.
Vascular malformations that affect the orbit and cavernous sinus that are caused by trauma are discussed in Chapters 59 and 75, respectively.
ANATOMIC AND DEVELOPMENTAL CONSIDERATIONS
Applied Anatomy
The relevant anatomy of the bony orbit, muscle cone, and related neurovascular structures is discussed in detail in Chapter 44.
IMAGING APPROACH
Techniques and Relevant Aspects
The orbit is studied with computed tomography (CT) and magnetic resonance (MR) techniques described in detail in Chapters 44 and 45. Specific CT protocols by indications are detailed in Appendix A. Specific MR protocols by indications are outlined in Appendix B. Almost all studies to investigate orbital trauma are done without contrast except if an infectious complication is suspected.
Pros and Cons
CT is done routinely for the evaluation of orbital injury and typically is sufficient for all medical decision making. Emergent evaluation with CT is indicated for possible associated tension orbit. Magnetic resonance imaging (MRI) is used occasionally to assess optic nerve compromise (Chapter 54) and in penetrating trauma to look for a retained foreign body.
Delayed complications such as hematic cysts in old subperiosteal or other hematomas or encephaloceles are more definitely diagnosed by MRI.
Ultrasound (US) may not be possible in a painful, swollen injured orbit; however, it can be used often and even in the face of open eye wounds. It is especially used to localize small anterior foreign bodies. It can also be helpful to identify ocular detachments and related fluid collections effusions that can be repaired and drained, possibly contributing to a better outcome (Chapter 51).
MR is used adjunctively in highly selected cases of penetrating trauma with possibly retained foreign bodies and in those complicated by orbital infection.
SPECIFIC DISEASE/CONDITION
Blunt Force Trauma and Orbital Fractures
Etiology
Acute trauma to the orbit may be blunt force or penetrating from a wide variety of untoward events. Both mechanisms can also occur during surgery, and both may result in the presence of retained foreign bodies. The chronic effects of orbital trauma due to those mechanisms are also discussed in this next section.
Clinical Presentation
Trauma may present with only soft tissue swelling or a hematoma. Facial deformity, either visible or palpable, suggests fractures. Each type of orbital fracture is generally associated with an expected possible array of signs and symptoms. These are discussed in the following section on patterns of disease. Since the fractures may be complex, such phenomena are possible in more than one specific type of fracture.
Loss of vision may be due to eye injury, optic nerve/sheath injury, and/or tension orbit. Associated retained foreign bodies may be suggested by the physical examination or mechanism of injury.
Pathophysiology and Patterns of Disease
The facial skeleton forms a series of struts in the vertical, horizontal, and sagittal planes discussed in Chapter 88. Fractures interrupt these struts, and the repair of facial injury aims at restoring the structural integrity of the struts toward creating a framework for optimal restoration of function with a good cosmetic result. Specific functional losses may be anticipated based on the pattern of injury. Orbital and other facial fractures in children may be buckled rather than frankly fractured. These may result from relatively minor trauma and tend to have a lesser association with complications than fractures in adults.
Le Fort, nasoethmoid, and other midface injuries involving the orbits are discussed in Chapter 88.
Blowout Fractures
Blowout fractures are commonly believed to be the result of blunt trauma to the eye, which raises the intraorbital pressure as the eye is displaced posteriorly into the orbit, compressing the rest of the soft tissues. Since the bony margins of the orbit are weakest along the orbital floor and medial wall, these structures preferentially fracture, creating inferior and medial orbital blowout fractures, respectively. Current thinking suggests that the main forces causing the fracture are transmitted to these weak areas from the thicker bone of the orbital rims.1 These tend to be single strut injuries, although floor and medial wall injuries frequently are the result of a single traumatic event.
The orbital floor is weakest where it is often dehiscent along the infraorbital canal and groove; the forces transmitted along this groove force bone fragments and soft tissues, including the infraorbital nerve, inferior rectus muscle, and orbital fat, into the superior aspect of the maxillary sinus (Figs. 63.1–63.6). Entrapment of the infraorbital nerve is manifest as maxillary region hypesthesia, while entrapment of the inferior rectus muscle results in restricted eye movement. Large-volume fractures can allow sufficient orbital fat to herniate into the defects and result in enophthalmos (Figs. 63.1, 63.4, and 63.5). This entrapped fat can become necrotic and fibrotic. Enophthalmos can lead to diplopia and is often cosmetically unacceptable. Necrosis and fibrosis of fat can result in delayed development of restricted eye movement as well as enophthalmos. It is for these reasons that most orbital floor blowouts are explored and reduced, even if gaze is normal. Methods of repair can also lead to scarring and abnormalities of eye movement (Fig. 63.6). Non- or minimally displaced fractures without muscle entrapment may not be explored. Imaging with CT is obviously crucial in this diagnostic approach. Some suggest that MR images may be useful.2 The cost of routine MRI does not seem justified, but it may be useful in selected cases.
The medial orbital wall floor is weakest where it is penetrated by the grooves of the anterior and posterior ethmoid arteries. The medial wall is normally composed of very thin, often dehiscent bone. The forces transmitted between the grooves force bone fragments and soft tissues, including the medial rectus muscle and orbital fat, into the ethmoid air cells. Medial blowout fractures are often not clinically significant even where there is considerable displacement of fat and the medial rectus muscle into the ethmoid air cells. Medial rectus dysfunction can result but is relatively uncommon (Fig. 63.7). Medial fractures may extend superiorly to involve the trochlea and superior oblique muscle and possibly the frontal sinus. Many of these fractures are seen as incidental findings on brain CT or MR studies done for other purposes long after the trauma has healed. Such deformity must be reported if sinus surgery is contemplated.
A medial blowout fracture may herald more severe injury to the ethmoid complex, which can, in turn, lead to cerebrospinal fluid leakage and/or meningitis; however, these complications are usually seen in the more complex midface injuries described in Chapter 88.
Orbital “Blow-In” Fractures
Orbital “blow-in” fractures are a result of a direct blow to the supraorbital or infraorbital rims. The force is transmitted to the orbital roof more posteriorly in supraorbital rim injury, resulting in displacement of bony fragments into the superior orbit1 or upward displacement of the orbital floor (Figs. 63.8–63.10). There may be an associated subperiosteal hematoma (Fig. 63.10). This fracture may be associated with globe injury or ocular mobility problems (Fig. 63.8). It can occasionally extend to the orbital apex and result in optic nerve injury (Fig. 63.9). There is a high incidence of intracranial abnormalities in patients with injuries to the superior orbital rim. The mechanism is not entirely understood, and a similar although usually less ominous situation may arise from inferior rim injury. The pattern of injury may be related to torque applied to the zygomatic complex along with compressive forces to the rim that may leave the rim not fractured but the energy applied expressed in terms of injury to the orbital roof and floor. Orbital blow-in fractures can result in chemosis, orbital hematoma, proptosis, tension orbit (Fig. 63.10), ptosis, and optic nerve contusion.
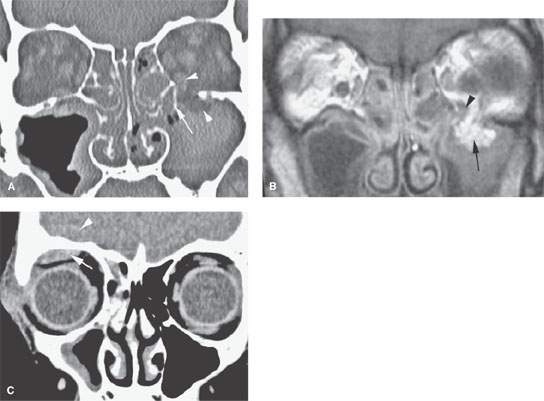
FIGURE 63.1. Computed tomography (CT) and magnetic resonance images of two patients with orbital fractures and restricted upward gaze. A, B: Patient 1. In (A), CT shows the fracture fragment (arrow) and both fat and inferior rectus muscle (arrowheads) herniated into the fracture site. In (B), T1-weighted image does not show the displaced bony fragment fracture but does show herniation of orbital fat (arrow) and possibly trapped inferior rectus (arrowhead). C: Patient 2. CT showed a nondisplaced superior orbital rim fracture (not shown) and a subperiosteal hematoma (arrow) that interfered with superior rectus function. There is also an epidural hematoma (arrowhead).
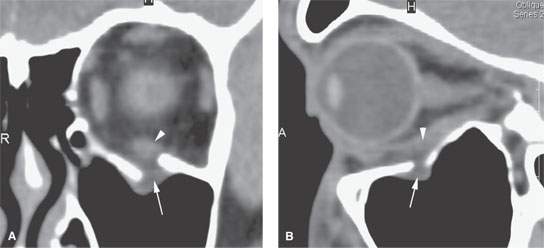
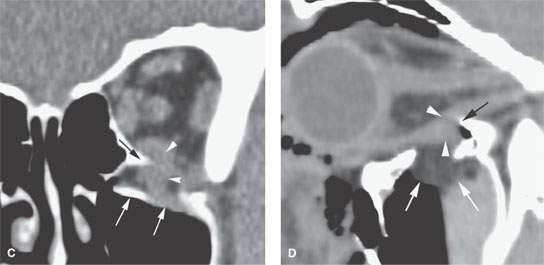
FIGURE 63.2. Computed tomography of two patients with orbital floor fractures and a question of inferior rectus entrapment. A, B: Patient 1. In (A), there is a minimally depressed floor fracture with trapping of a minimal volume of orbital fat (arrow). The inferior rectus does not appear to be trapped. In (B), sagittal reformations show the fracture and minimal fat herniation (arrow) and that the inferior rectus is not trapped (arrowhead). C, D: Patient 2. In (C), there is a displaced fracture of the orbital floor (arrows) and inferior rectus muscle entrapment (arrowheads); the muscle possibly is impaled on the bony fracture margin (black arrow). In (D), sagittal reformation confirms high-volume orbital floor injury with herniated fat (white arrows). The inferior rectus muscle (arrowheads) appears to be trapped between spicules of bone (black arrow).
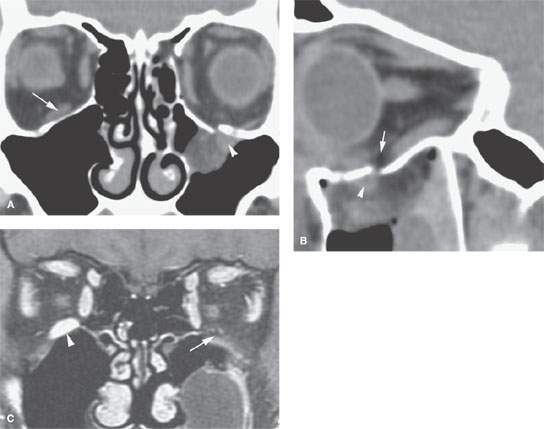
FIGURE 63.3. Computed tomography of a patient with an orbital blow fracture. A: There is a small fracture site and herniated orbital fat visible (arrowhead). The inferior rectus is not visible compared to the other side (arrow); this suggests a “trap door” fracture. B: This trap door mechanism is confirmed in the sagittal reformation where the inferior rectus muscle is segmentally absent (arrow) and that muscle segment and orbital fat are trapped in the maxillary sinus (arrowhead). (NOTE: This is referred to as a trap door injury since the bony defect is small, but the amount of trapped tissue is large due to transiently opening and then closing of the orbital floor during the injury.) C: This was repaired; however, the contrast-enhanced T1-weighted fat-suppressed image shows that the inferior rectus muscle was permanently injured and became atrophic because of it being trapped and devitalized (arrow) compared to the normal side (arrowhead).
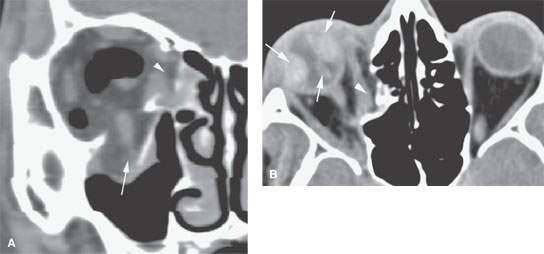
FIGURE 63.4. A: Computed tomography of a high-volume medial wall (arrowhead) and orbital floor (arrow) injury. B: Associated ocular injury with bilateral choroidal and a vitreous bleeds (arrows) and a displaced medial blowout (arrowhead).
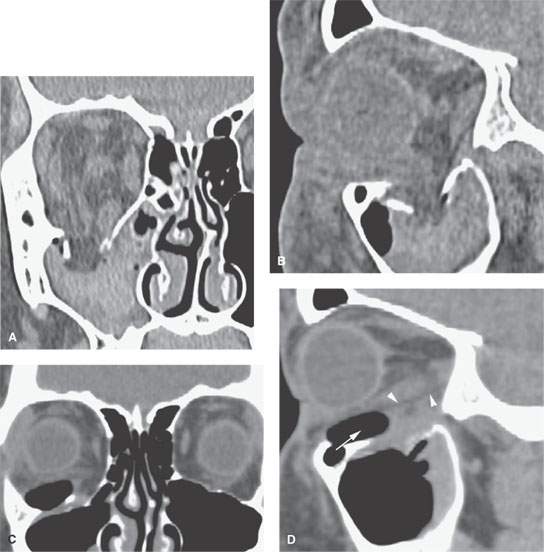
FIGURE 63.5. Patient with a high-volume orbital floor injury as seen in (A) and (B). In correlating images in (C) and (D), prosthesis restores this orbital floor. In the sagittal reformation (D), a fat plane is visible between the repair and the inferior rectus muscle. (NOTE: Ocular motility was normal. Contrast this result with that in Fig. 63.6.)
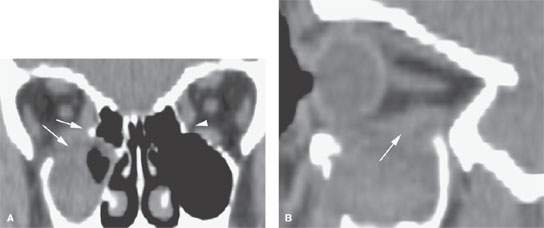
FIGURE 63.6. Patient suffering an orbital injury blowout that was repaired and had ocular motility problems following the repair. A: Coronal reformation shows the inferior rectus segmentally adherent to sinus contents as well as to the medial rectus (arrow) compared to the other side (arrowhead). B: Sagittal reformation also shows the inferior rectus segmentally adherent to sinus contents (arrow).
Long-term complications of these fractures may directly involve the visual pathways and include ocular pathology (Fig. 63.11) and optic nerve atrophy (Fig. 63.12). Delayed complications also include intraorbital mucocele (Fig. 63.13) due to entrapped sinus mucosa, cholesterol cysts from unresolved subperiosteal hematomas, and encephaloceles (Figs. 63.11–63.13).
An isolated subperiosteal hematoma may occur due to such a force, and that risk is increased if the patient is on anticoagulants. Such a hematoma may also be spontaneous or induced by a Valsalva (Fig. 63.14).
Orbitozygomatic/Zygomaticomaxillary Complex (Previously Known as Tripod and Trimalar) Injuries
The nasomaxillary, pterygomaxillary, and zygomaticomaxillary buttresses distribute forces of blunt force trauma of the cheek; thus, the zygomatic complex fractures mainly along the related suture lines. Fractures then involve the infraorbital rim, posterolateral orbital wall and course toward the inferior orbital fissure, the latter often with a significant orbital floor disruption (Figs. 63.15–63.17). The frontozygomatic suture is often disrupted, and there will often be a single zygomatic arch fracture. The sphenozygomatic junction part of the injury will express itself as a lateral orbital wall injury and will account for much of the lateral displacement present.
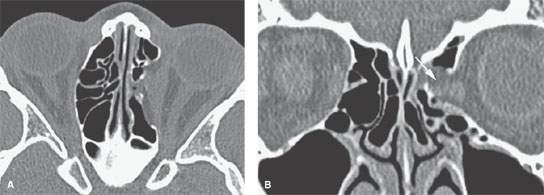
FIGURE 63.7. Computed tomography of a high-volume medial orbital wall injury with media rectus dysfunction entrapment (arrow). A similar imaging finding, however, might not be necessarily associated with an ocular motility problem.
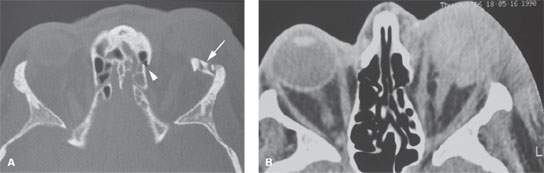
FIGURE 63.8. Computed tomography of an orbital blow-in fracture with displacement of the supraorbital rim (arrow in A) and a devitalized globe (B). (NOTE: Blow-in fractures have a relatively high rate of injury to the ocular apparatus and intracranially compared to other blunt force orbital fractures.)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








