, Prashant Raghavan2, Max Wintermark3, Steven A. Newman4 and Sugoto Mukherjee5
(1)
Department of Radiology and Medical Imaging, University of Virginia Health System, Charlottesville, VA, USA
(2)
Division of Neuroradiology, Department of Diagnostic Radiology and Nuclear Medicine, University of Maryland School of Medicine, Baltimore, MD, USA
(3)
Department of Radiology and Medical Imaging, University of Virginia Health System, Charlottesville, VA, USA
(4)
Department of Ophthalmology, University of Virginia Health System, Charlottesville, VA, USA
(5)
Division of Neuroradiology, Department of Radiology and Medical Imaging, University of Virginia Health System, Charlottesville, VA, USA
Abstract
This chapter describes the imaging characteristics of the more common orbital lesions. Although a specific imaging diagnosis of orbital pathology may not always be possible, a combination of clinical information and imaging features can enable a relatively short list of differential diagnoses to be formulated in most instances.
7.1 Introduction
This chapter describes the imaging characteristics of the more common orbital lesions. Although a specific imaging diagnosis of orbital pathology may not always be possible, a combination of clinical information and imaging features can enable a relatively short list of differential diagnoses to be formulated in most instances.
7.2 Anatomy
The orbit is a pyramidal-shaped cavity formed by seven bones. The roof is formed by the orbital process of frontal bone and the lesser wing of sphenoid. The floor is formed by the orbital plates of the maxilla, zygoma, and the palatine bone. The medial wall is formed by the frontal process of the maxilla, the lacrimal bone, and the gracile lamina papyracea of the ethmoid bone. The greater wing of sphenoid, the zygoma, and the zygomatic process of frontal bone form the lateral wall (Figs. 7.1, 7.2, and 7.3).
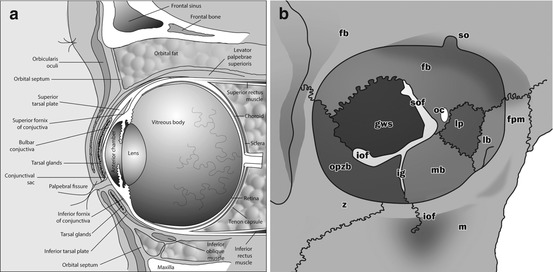
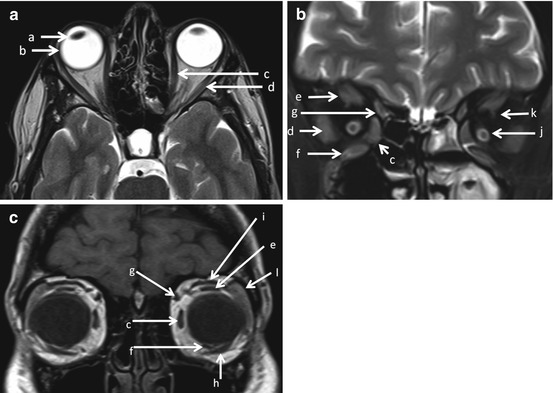
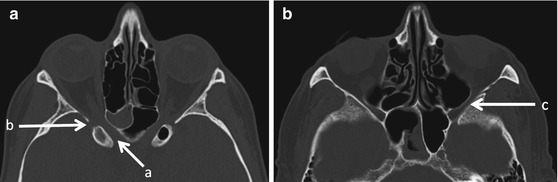
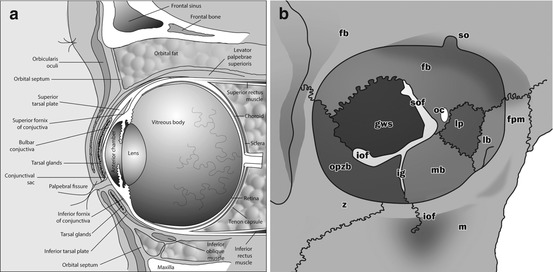
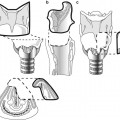
Fig. 7.1
Sagittal graphic (a) showing the gross anatomy of the globe and the orbit. Note the three layers of the globe consisting of retina, choroid, and sclera. The bony orbit (b) shows the relationships of the various foramina and fissures including the superior orbital fissure (sof), inferior orbital fissure (iof), and the optic canal (oc), as well as the superior (sf) and the inferior orbital foramina (iof). The bones forming the bony orbit include frontal bone (fb), greater wing of sphenoid (gws), orbital plate of the zygomatic bone (opzb), lacrimal bone (lb), frontal process of maxilla (fpm), supraorbital notch (so), infraorbital groove (ig), maxillary bone (mb), and lamina papyracea (lp). Other abbreviations in the figure include m maxilla, z zygomatic bone
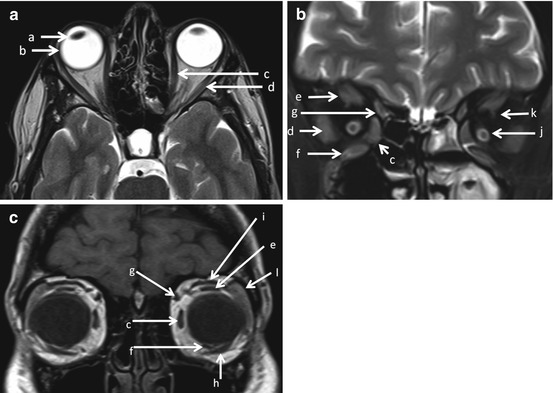
Fig. 7.2
Axial T2WI (a) and coronal T2WI with fat saturation (b) and coronal T1WI (c) show the easily identifiable intraorbital structures and extraocular muscles on MR. These include (a) lens, (b) globe, (c) medial rectus, (d) lateral rectus, (e) superior rectus, (f) inferior rectus, (g) superior oblique, (h) inferior oblique, (i) levator palpebrae superioris, (j) optic nerve sheath complex showing optic nerve surrounded by fluid in the optic nerve sheath, (k) superior ophthalmic vein, and (l) lacrimal gland
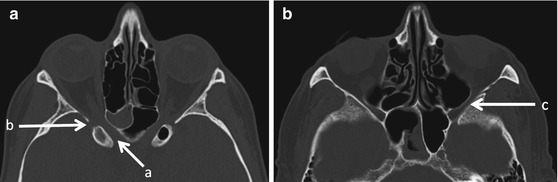
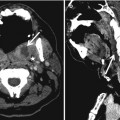
Fig. 7.3
Axial CT images (a, b) show the interrelationships of (a) optic canal, (b) superior orbital fissure, and (c) inferior orbital fissure
The contents of the orbit include the globe, the external ocular muscles (EOM), the optic nerve, cranial nerves III and IV, the first (ophthalmic, V1) division of V and VI, the ophthalmic artery, the superior and inferior ophthalmic veins, fat, the lacrimal apparatus, and the orbital septum (Figs. 7.1, 7.2, and 7.3).
The contents of the various channels of the orbit are summarized in Box 7.1.
7.3 Imaging Modalities
7.3.1 Ultrasound
Ultrasound of the orbit is best performed with a high-frequency linear transducer, ideally 10 MHz or higher. US is used to evaluate the eye and superficial structures and provides limited evaluation of deeper intraorbital structures. It is particularly useful when ophthalmoscopic examination is limited due to the presence of opaque ocular media such as by cataract or vitreous hemorrhage. US is commonly performed by the ophthalmologist as an office procedure for evaluating a mass seen during ophthalmoscopy, to look for a mass underlying a retinal detachment, to evaluate ocular trauma, and for biometry. Color Doppler can be used to evaluate lesional vascularity.
7.3.2 Cross-Sectional Imaging
CT is the modality of choice in suspected orbital trauma, in orbital infection in the setting of sinusitis, and in the initial evaluation of an orbital mass. In patients with trauma, an unenhanced scan is sufficient. CT demonstrates bony changes and calcifications better than MRI. However, it must be employed judiciously in children and young patients where radiation exposure to the lens is a legitimate concern. CT scan and MRI can both provide complimentary information in the evaluation of orbital masses. A standard orbit MR study comprises of axial and coronal thin section unenhanced non-fat-suppressed T1-weighted images (the hyperintense fat provides excellent background contrast), a coronal fat-suppressed T2W sequence (for evaluating the optic nerve), and post-contrast fat-suppressed axial and coronal T1W images. CTA and MRA are useful when a vascular process such as a carotid-cavernous fistula or AV malformation is suspected.
The primary role of the radiologist is to precisely localize the lesion, estimate its site of origin and describe its extent. An attempt should be made to describe the lesion as focal or multispatial (Box 7.2), whether it involves intra or extraconal compartments, and its origin from the globe, optic nerve, lacrimal gland, vascular structures, extraocular muscles or the bony orbit.
7.4 Congenital/Developmental Anomalies
7.4.1 Coloboma
A coloboma is a focal discontinuity in the structure of the globe resulting from the failure of closure of the embryonic choroid fissure between the 5th and 7th weeks of life. Posterior colobomas, which include choroidoretinal, and optic disc colobomas are the more common type. They can occur as isolated lesions or as a part of a more widespread syndromic process. Isolated colobomas are usually unilateral, while syndromic forms tend to be bilateral. They appear as focal protrusions isodense to the vitreous on non-enhanced CT (NECT) scan and isointense to the vitreous of MRI, unless complicated by retinal detachment and hemorrhage (Fig. 7.4). A large coloboma may also present as an intraorbital cyst associated with a small globe (microphthalmia).


Fig. 7.4
Coloboma and lacrimal abscess. Axial contrast-enhanced CT scan showing incidental finding of coloboma of the right eye (long arrow). The patient was imaged for the left lacrimal gland abscess (short arrow)
7.4.2 Persistent Hyperplastic Primary Vitreous
Persistent hyperplastic primary vitreous results from failure of regression of embryonic ocular blood supply. There are three types—posterior, anterior, and mixed. In posterior PHPV, there is an enhancing retrolental soft tissue with a stalk, representing the remnant of the primitive hyaloid artery, extending from the posterior surface of the lens to the head of the optic nerve (Fig. 7.5). Retinal detachment is frequently present and the globe is small. In anterior PHPV, the anterior chamber is shallow, the lens is thin and dysplastic, and an abnormal enhancing tissue is present in the region of the ciliary body and lens. The mixed type demonstrates features of posterior and anterior PHPV.
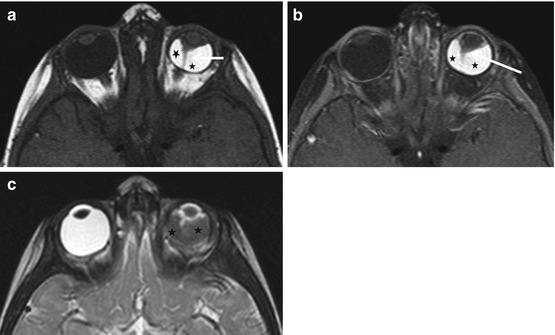
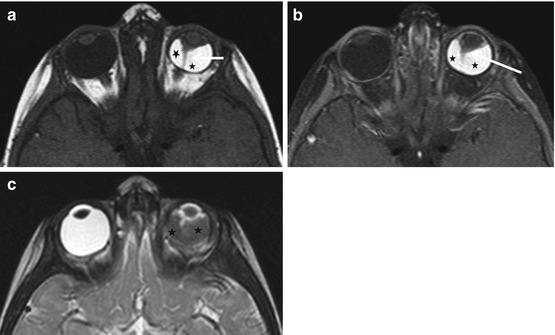
Fig. 7.5
Persistent hyperplastic primary vitreous (PHPV) in a 1-year-old patient. Axial T1 (a), axial fat-sat T1 post-contrast (b), and axial T2 (c) showing small left globe, stalklike hyaloid remnant extending from the posterior surface of the lens to the head of the optic nerve (short arrow), enhancing retrolental soft tissue (long arrow), and associated retinal detachment with hemorrhage (black star)
7.4.3 Coats’ Disease
Coats’ disease, seen in children, usually boys, under the age of ten, is caused by retinal telangiectasias and a leaky blood retinal barrier, which results in subretinal exudate accumulation. Coats’ disease is usually unilateral and results in retinal detachment. The exudate appears hyperdense compared to vitreous on CT. The exudate, comprised mainly of cholesterol, is hyperintense on T1W MR images. Patients usually present with leukocoria and vision loss. The most important differential is retinoblastoma. On CT, the lack of calcification of the exudate of Coats enables differentiation from retinoblastoma. Also, post-contrast studies show no enhancement of the subretinal collection. Linear enhancement of the retinal detachment may however be present.
7.4.4 Dermoids/Epidermoids
A dermoid is a congenital inclusion cyst occurring near suture lines, adjacent to the periosteum. The most common site is the superolateral portion of the orbit. Dermoid cysts commonly result in bony remodeling. They may be exophytic or endophytic. Exophytic cysts grow externally and are discovered early in childhood, while endophytic cysts grow internally and are encountered later in youth or early adulthood. Exophytic dermoids are usually small as they are identified earlier. Endophytic cysts are larger and may be associated with extensive bony changes. Other cystic lesions are summarized in Box 7.3.
They appear on unenhanced CT as well-defined fat density lesions (Fig. 7.6). The fat density is by no means universal, and it is not uncommon for them to present as fluid-containing lesions with no fat density. On MRI, the high T1 signal on fat, when present, is characteristic. Occasionally a heterogeneous appearance due to intracystic debris may be encountered (Fig. 7.6). Sometimes, thin marginal enhancement on CT and MRI may be present. Irregular margins and perilesional inflammatory changes indicate rupture.
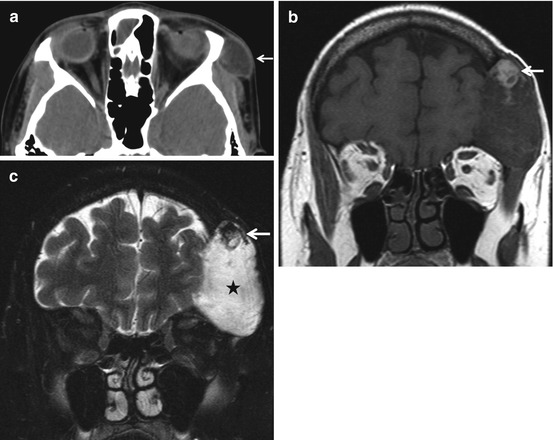
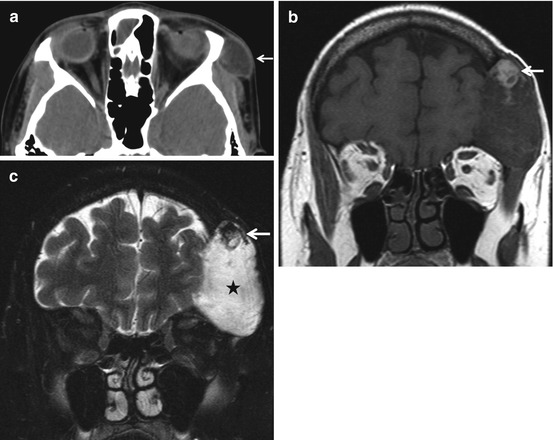
Fig. 7.6
Orbital dermoid. A 12-year-old patient presenting with gradually progressive, painless left periorbital swelling. Axial CT (a) showing cystic lesion without fat density along the superolateral margin of left orbit (white arrow). A 54-year-old patient, with long-standing history of left frontal swelling. Coronal T1WI (b) showing mixed signal intensity lesion with prominent fat nodule in its superior aspect (white arrow) with left frontal calvarial involvement. Coronal T2 fat-sat image (c) showing fat suppression in the superior nodular lesion (white arrow) and the hyperintense cystic component (black star). Compared to (a), this lesion is much bigger, with extensive lytic area in the frontal bone, related to the chronicity. The presence of fat within the lesion helps in diagnosis
Epidermoid cysts demonstrate fluid signal/density on MRI and CT. A characteristic finding on MRI is restricted diffusion.
7.4.5 Neurofibromatosis Type 1
The ocular and orbital manifestations of NF1 include sphenoid wing dysplasia, plexiform neurofibroma, optic nerve glioma, buphthalmos, and optic nerve sheath ectasia. Sphenoid dysplasia, thinning, remodeling, or deficiency of the greater sphenoid wing, can result in the “bare orbit sign” on a frontal radiograph of the skull. Plexiform neurofibromas appear as variably enhancing infiltrative soft tissue masses on cross-sectional imaging. The target sign produced by foci of central T2 hypointensity is a typical finding. Perioptic dural sheath ectasia is an uncommon benign finding in patients with NF1. The distended CSF-filled sheaths are easily recognized on T2W MRI. Optic nerve gliomas are characterized by expansion of the nerve itself. They may be limited to the nerve or extend substantially along the visual pathway to involve the chiasm and hypothalamus (Fig. 7.7). They are low-grade neoplasms (pilocytic or fibrillary astrocytomas) and are frequently bilateral. No calcification is present on CT. They are of intermediate signal intensity and enhance variably on MRI.
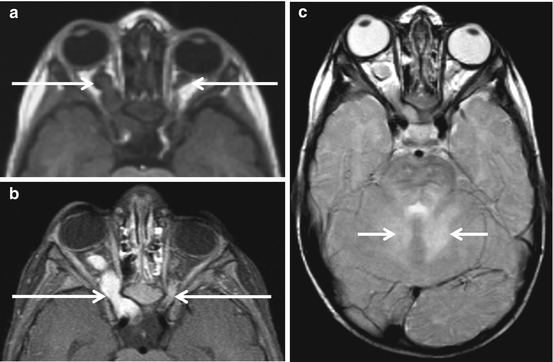
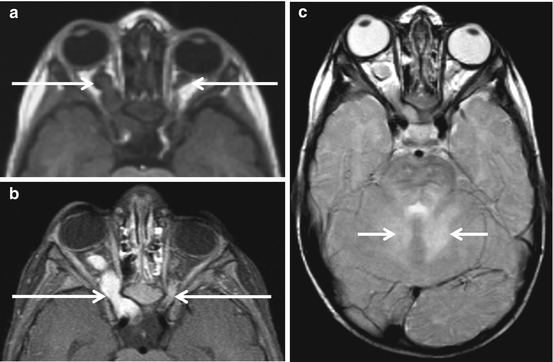
Fig. 7.7
Optic nerve gliomas in NF1. Axial T1-weighted images (a) showing bilateral optic gliomas (long arrows), right worse than left in a patient with NF1. Post-contrast axial T1 fat-sat image (b) shows enhancement of these lesions (long arrows). Axial T2-weighted sequences (c) show characteristic lesions of FASI (foci of abnormal signal intensity). These appear as non-enhancing foci of T2 prolongation and are thought to represent areas of myelin vacuolization (short arrows in c)
7.5 Vascular Anomalies
7.5.1 Orbital Venous-Lymphatic Malformation (Lymphangioma)
Venous-lymphatic malformations are poorly marginated frequently trans-spatial multicystic lesions comprised of variable amounts of dysplastic lymphatic and venous elements. These lesions are best characterized on MRI. Cystic areas may show fluid-fluid levels and can contain blood products (Fig. 7.8). Enhancement is variable and is a function of the proportion of the venous component. Phleboliths, which appear on CT, as well-defined rounded calcific foci are a useful clue when present.
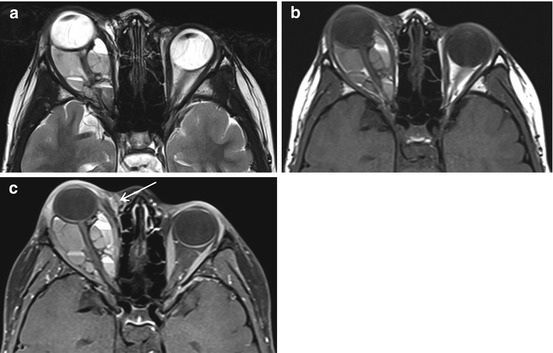
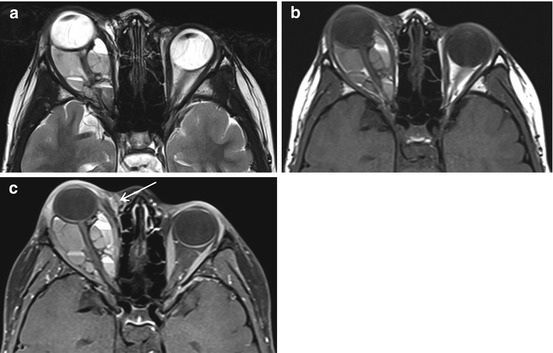
Fig. 7.8
Orbital venolymphatic malformation. Axial T2WI (a) showing complex multispatial lesion with multiple blood fluid levels in the right orbit in a 6-year-old patient. Axial precontrast TIWI (b) and post-contrast T1 fat-sat image (c) show a small enhancing portion (arrow in c) along the medial canthus of right eye
7.5.2 Venous Varix
An orbital venous varix is a distensible low-flow venous malformation connected with the systemic circulation. When large enough, it can result in intermittent reversible proptosis. Varices increase in size when systemic venous pressure increases, such as with coughing, straining, or compression of the jugular vein. Occasionally thrombosis, calcification, or hemorrhage can occur. Uncomplicated lesions appear as tubular soft tissue densities that enhance intensely with contrast. Patent varices can be made more conspicuous with the Valsalva maneuver. On MRI complex signal intensities due to slow flow and thrombosis may be present (Fig. 7.9).
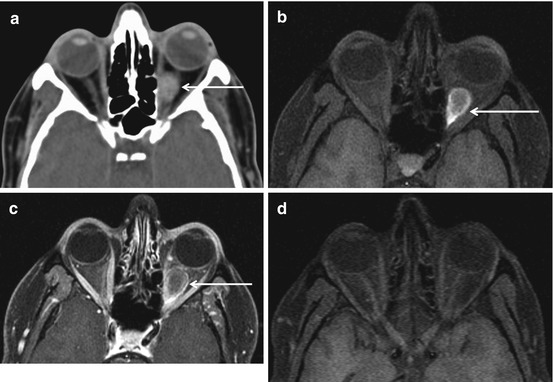
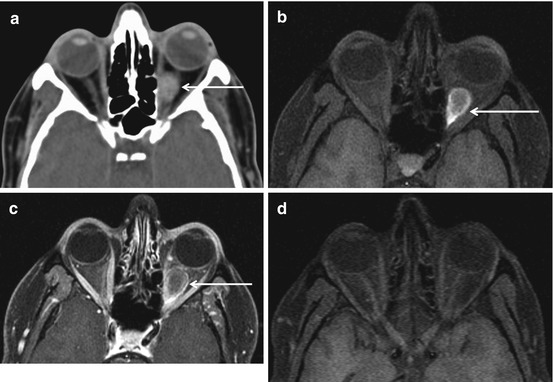
Fig. 7.9
Thrombosed venous varix. Axial CT scan (a) in this 42-year-old patient presenting with sudden onset left eye pain shows a well-defined hyperdense intraconal lesion (arrow). Axial T1 fat-sat image (b) also shows the T hyperintense intraconal lesion (arrow in b), without enhancement in post-contrast axial T1 fat-sat image (arrow in c). Follow-up axial T1 fat-sat image (d) after 3 months showing complete resolution of the lesion. The important pediatric lesions are summarized in Box 7.4
7.5.3 Cavernous Hemangioma
Cavernous hemangiomas, the most commonly encountered orbital masses in adults, are vascular malformations comprised of endothelial-lined cavernous spaces with a pseudocapsule of compressed normal orbital tissue. They are often incidentally detected on imaging but can present with slowly progressive painless proptosis. They are typically located in the intraconal compartment. They appear as well-defined homogeneous, noncalcified round or oval masses that exhibit progressive enhancement on delayed scans (Fig. 7.10).
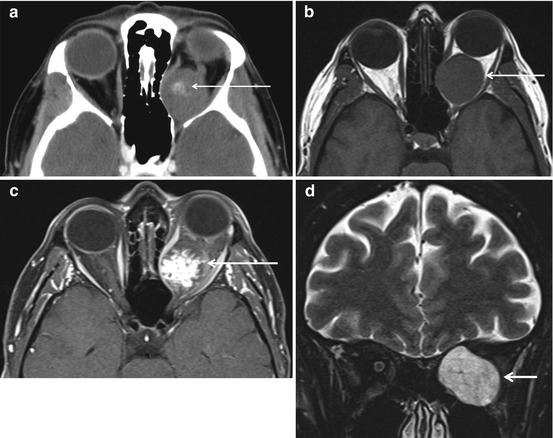
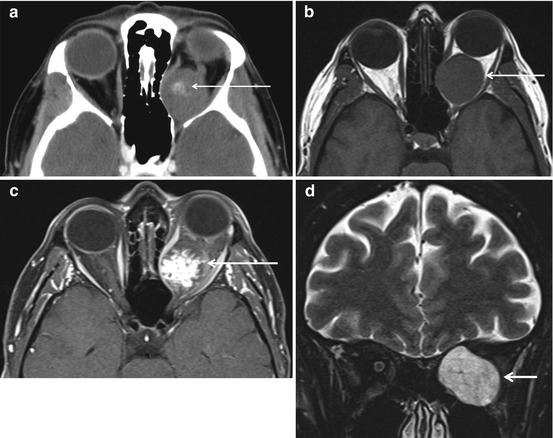
Fig. 7.10
Cavernous hemangioma. Axial CECT (a) showing central patchy enhancement in a well-defined intraconal lesion. In (b and c), the lesion is of intermediate signal intensity and enhances in a centripetal fashion. Coronal T2 fat-sat image (d) shows the characteristic T2 hyperintense nature of the lesion (arrow)
7.6 Infectious and Inflammatory Disorders
The orbital complications of sinusitis are discussed in detail in Chap. 9.
These along with trauma and hemorrhage are the most common cause of acute proptosis (Box 7.5).
7.6.1 Idiopathic Orbital Inflammatory Disease
Idiopathic orbital inflammatory disease (orbital pseudotumor) is a poorly understood non-granulomatous steroid responsive disorder that can afflict any structure in the orbit. IOID occurs in five forms—anterior (globe and retrobulbar soft tissues), lacrimal, myositic, apical (involvement of the orbital apex and cavernous sinus, Tolosa-Hunt syndrome), and diffuse and sclerosing (bilateral affliction of the orbits and paranasal sinuses) (Figs. 7.11 and 7.12). Painful unilateral ophthalmoplegia is the most common presenting feature. The myositic form, which on imaging is characterized by uniform enlargement of one or more extraocular muscles and their tendon sheaths, is the most frequently encountered variety of IOID. Involvement of the tendon sheaths is a typical finding in IOP and enables differentiation from thyroid ophthalmopathy, where despite smooth enlargement of the muscle belly, the tendon is unaffected. IOID may also occur as a diffusely infiltrative relatively T2 hypointense enhancing process. When fibrosis is marked, the lesion may be profoundly T2 hypointense. Orbital lymphoma, sarcoidosis, and Wegener’s granulomatosis can have very similar imaging appearances (Box 7.6), and one may have to rely on clinical data to arrive at the correct diagnosis. IgG4-related sclerosing disease is a type of orbital pseudotumor characterized by lymphoplasmacytic tissue infiltration with a predominance of IgG4-positive plasma cells, usually accompanied by fibrosis, and elevated serum levels of IgG4. IgG4-related sclerosing disease radiologically is indistinguishable from IOID.
Get Clinical Tree app for offline access
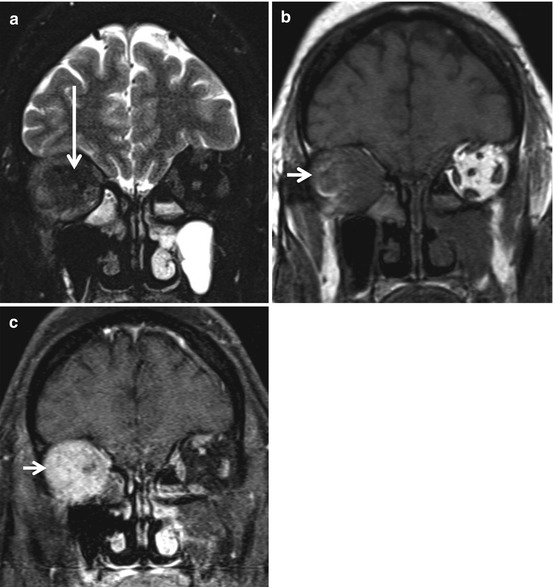
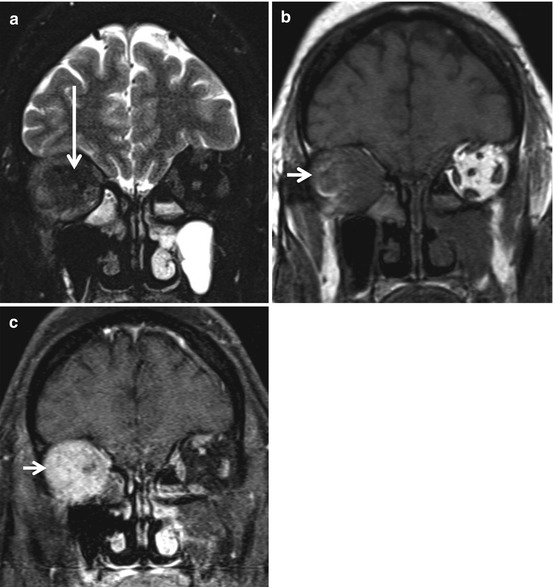
Fig. 7.11
Idiopathic orbital pseudotumor. Coronal T2 (a), precontrast T1 (b), and post-contrast T1 fat-sat (c) images, in a 42-year-old with painful slowly progressive proptosis, demonstrate an ill-defined T2 hypointense (compared to the extraocular muscles) (long arrow in a), enhancing lesion (short arrow in b and c




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree