OROPHARYNX: BENIGN NONINFLAMMATORY MASSES AND TUMORS
KEY POINTS
- Computed tomography and magnetic resonance imaging are very valuable diagnostic tools for the evaluation of submucosal oropharyngeal masses that are eventually shown to be benign.
- Such imaging can help to avoid possible complications such as excessive bleeding from endoscopic biopsy.
After physical examination, it is often difficult to decide whether an area of oropharyngeal swelling is neoplastic, inflammatory, traumatic, or degenerative. Even after biopsy, the etiology may remain obscure.
Most benign tumors or focal areas of swelling in the oropharynx will have a nonspecific imaging appearance. On occasion, imaging findings will be specific enough to allow an etiologic or, sometimes, a very likely specific tissue diagnosis.1–3 The most fitting and usual use of computed tomography (CT) and magnetic resonance imaging (MRI) is to show the extent of the lesion and identify the likely etiology of a submucosal mass. Some of these masses will be due to developmental lesions discussed in Chapter 191; all of the masses are very uncommon.
ANATOMIC AND DEVELOPMENTAL CONSIDERATIONS
Applied Anatomy
The critical anatomic knowledge necessary for the evaluation of oropharyngeal tumors is summarized here. The detailed anatomy of this region and the related nasopharynx, oral cavity, larynx and hypopharynx, and related deep tissue spaces is reviewed in chapters indicated in parentheses in the summary that follows. A detailed working knowledge of all of this anatomy is necessary to evaluate images of patients with known or suspected oropharyngeal benign tumors if the evaluation of the image is expected to contribute measurably to medical decisions.
The general anatomic knowledge necessary to evaluate benign tumors of the oropharynx includes the following:
- Regional anatomy of the oropharynx, including the tonsillar pillars, palatine tonsils, tongue base, glossotonsillar sulci, and valleculae (including the normal variation of lymphoid tissue lining the mucosal surfaces) and of the parapharyngeal space (Chapters 142 and 190)
- Related regional anatomy of the structures above and below the oropharynx, including the nasopharynx (Chapter 184), oral cavity (in Chapter 196, mainly the anatomy of the floor of the mouth and pterygomandibular raphe), larynx (in Chapter 196, the tongue base relationship to the pre-epiglottic space), and hypopharynx
- Bony anatomy, including the hard palate, pterygoid plates, and mandible (Chapter 196)
- Neurovascular bundles, including the lingual and hypoglossal nerves and greater and lesser palatine and posterior superior alveolar neurovascular bundles
IMAGING APPROACH
Techniques and Relevant Aspects
Computed Tomography and Magnetic Resonance Imaging
Benign lesions of the oropharynx are studied with CT and MRI in essentially the same manner as malignant oropharyngeal cancers, except the neck may not be included. The specifics and relative value of using these studies in this anatomic region are reviewed in Chapter 190. Problem-driven protocols for CT and MRI are presented in Appendixes A and B. In general, MRI is more definitive than CT in the evaluation of submucosal oropharyngeal and deep space masses at this level of the suprahyoid neck, as these images are usually of good quality above the hyoid.
Other Imaging
Ultrasound has no significant role to play in the evaluation of these masses. Radionuclide studies have little or no diagnostic use for the evaluation of benign oropharyngeal masses, and the normal variations in this region seen on fluorine-18 2-fluoro-2-deoxy-D-glucose positron emission tomography (FDG-PET) studies significantly limit any potential value. Catheter angiography is used rarely.
Pros and Cons
Evaluation of a Submucosal Mass or Other Mass of Uncertain Etiology
Benign masses limited to the oropharynx often mimic the initial presentation of oropharyngeal cancer. Any mass, regardless of etiology, that is suspicious for deep infiltration or cancer should be studied primarily with CT if imaging is desired as part of the evaluation (Figs. 194.1–194.3). MRI can be used initially if preferred. Supplemental magnetic resonance (MR) study, in the situations where it might add meaningful incremental data, is best directed by CT findings to a localized area of interest where its strengths related to better soft tissue contrast resolution may be exploited.
Integrity of the Airway
In any imaging study of the oropharynx, the diseased condition must be evaluated for its effect, or potential effects of diagnostic or therapeutic efforts, on the airway. The anatomic status of the airway as well as the risk of any acute adverse complication, such as the potential for rapidly progressive airway obstruction either by the mass or a potential airway complication that might arise as a result of biopsy, should be reported. For instance, biopsy of an unanticipated vascular malformation could lead to an unfortunate amount of hemorrhage and aspiration of blood or rapid airway compromise (Fig. 194.4).
Evaluation of Pharyngeal Dysfunction Possibly Due to Submucosal Masses
Some patients have processes predominantly occurring beneath intact oropharyngeal mucosa that cause dysphagia and/or odynophagia with no visible mass. Imaging is particularly valuable to the head and neck surgeon to detect or exclude a submucosal lesion that may spread underneath intact and normal-appearing mucosa causing such symptoms (Figs. 194.2–194.5).
BENIGN TUMORS OF THE OROPHARYNX
Etiology
Benign tumors of the oropharynx are rare and typically have no particular etiology. A neurogenic tumor might be associated with neurofibromatosis.
Prevalence and Epidemiology
Minor salivary gland tumors,1 rhabdomyomas, leiomyomas, lipomas,2 neurogenic tumors,3 and those of fibrous origin are all very rare lesions that may present in the oropharynx. Parapharyngeal masses that may cause bulging of the oropharyngeal wall are discussed in Chapter 143.
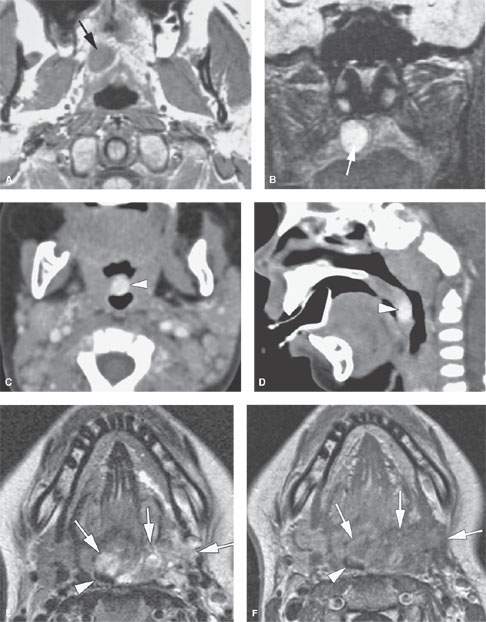

FIGURE 194.1. Three patients with submucosal oropharyngeal masses. A, B: Magnetic resonance imaging study of Patient 1, an adult with a submucosal soft palate mass with morphology and signal intensity characteristics consistent with the benign mixed tumor subsequently proven at surgery. T1-weighted (T1W) (A) and T2-weighted (T2) (B) images are shown. C, D: Patient 2, an 11-month-old child presenting with a reddish mass on the uvula. Axial (C) and sagittal (D) reformations of a contrast-enhanced computed tomography study show a strongly enhancing nodular lesion (arrowhead) in the uvula, compatible with proliferative hemangioma. The lesion slowly regressed over time. E–G: Patient 3, an adult suffering dyspnea and dysphagia. During childhood, she was surgically treated for a benign, congenital lesion in the neck. Clinical examination showed a submucosal oropharyngeal mass lesion on the left, severely narrowing the lumen. Axial T2W (E) and axial (F) and coronal (G) gadolinium-enhanced T1W spin echo images show a heterogeneous mass in the left oropharyngeal wall (arrows) narrowing the lumen (arrowhead). The mass contains liquid and solid components and shows moderate and heterogeneous enhancement. No signal voids are seen. The morphology, signal intensities, and enhancement pattern is compatible with a low-flow vascular malformation. The coronal image shows the extensive involvement of the oropharyngeal structures, including the tongue base, lateral wall, and soft palate; the lesion also extends in the lateral wall of the nasopharynx. (NOTE: Treatment was by laser debulking, increasing the oropharyngeal lumen. This treatment could be safely performed, as imaging showed the absence of large intralesional vessels.)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








