OROPHARYNX: INTRODUCTION
IMAGING APPROACH
Techniques and Relevant Aspects
General Examination Technique
Patients should be positioned with the neck extended so that the mandibular body is perpendicular to the tabletop for either computed tomography (CT) or magnetic resonance (MR) study. When using multidetector computed tomography (MDCT), the data acquisition is best done with zero gantry tilt. This may cause problems when dental fillings or unremoveable appliances are present. If the images are severely degraded by these artifacts arising from dental appliances, one solution is to obtain a second series of CT images with the mouth opened.1 The CT gantry may also be angled, based on the planning digital radiograph, to minimize artifacts produced by dental appliances that cannot be removed and two separate data acquisitions done at the expense of some reirradiation of overlapping sections. Alternatively, a complementary MR study may be done.
Sections done through the nasopharynx should be optimally made or viewed parallel to the hard palate. Those through the oropharynx may be parallel to the hard palate or mandibular body. Steeper angulations can lead to diagnostic errors in evaluating primarily oropharyngeal pathology unless the data set can be reangled at the diagnostic interpretation workstation and/or the reader is aware of this pitfall. The importance of proper angulation of sections through the oropharynx cannot be overstated. Sections through the oropharynx viewed parallel to the body of the mandible make more anatomic sense given the relationships of the tongue base to the floor of the mouth and deeper structures of the neck. Very oblique section planes may lead to a confusing display of the pathology relative to surgical as well as radiotherapy landmarks. Such a confusing display can lead to serious errors in medical decision making, especially if surgery is contemplated.
Oropharyngeal CT and magnetic resonance imaging (MRI) always include axial views as a routine and only infrequently mandate use of coronal sections. Coronal and sometimes sagittal viewing is essential for some studies of cancer patients, mainly in those cases when there is a complex relationship between cancer or other pathologies and the floor of the mouth, tongue base, mandible, and spaces of the suprahyoid neck or in the unusual instances when tumors approach the skull base (Fig. 7.3). To be safe, coronals may be routinely included in MR protocols. The can always be reconstructed or reformatted retrospectively in a properly acquired volume CT data set.
On CT studies, axial sections are acquired and then these source images are archived. Volume CT data sets should be obtained with 0.5- to 1.0-mm sections suitable for the highest-resolution multiplanar reconstructions and/or reformations required for the diagnostic task at hand. Reconstruction of the images at 1- to 3-mm slice thickness (SLT) is, however, suitable for evaluating the soft tissue extent of cancers, and reconstructing at that larger SLT will improve low-contrast resolution considerably and will suffice when fine bone detail and reformations are not necessary (Appendix A).
Axial images are the mainstay for evaluating pathologic relationships in most critical anatomic zones. MDCT (especially $16 slice) makes it easy to obtain the axial images since such a volume data set can be routinely reconstructed and then viewed with multiplanar reformation tools in virtually any plane, as discussed in Chapter 2. These studies must be viewed at both bone and soft tissue windows. Additional reconstructions with a bone algorithm may be part of cancer protocols (Appendix A), but oropharyngeal cancer only infrequently involves bone. Keep in mind that significant bone changes can be missed when viewing bone windows only on images reconstructed with a soft tissue algorithm (Figs. 21.41 and 21.42 and Chapter 21); therefore, additional thinner reconstructions with bone windows may be necessary from saved raw data whenever bone is threatened.
Iodinated contrast is used on almost all oropharyngeal CT studies. If iodinated contrast cannot be used, then MRI should be done instead unless only bone information is the object of interest. It is very important not to begin scanning too early in the contrast injection. Peak enhancement of most cancers and other pathology not directly related to blood vessels relative to normal tissue may be missed if scanning is begun too early. Specific CT protocols are presented in Appendix A.
MRI should be done with 3- to 4-mm sections and a field of view of about 12 to 16 cm. All three orthogonal planes might be obtained, but axial and coronal sections almost always suffice. T1- and T2-weighted images should be obtained. Fat suppression may be used but may be unpredictably degraded by susceptibility artifacts in critical areas such as the mandible, usually due to dental appliances (Fig. 1.3). Non–fat-suppressed T1-weighted images before and after contrast and T2-weighted images are a safer choice, although the examination becomes lengthened. Intravenous contrast is used in most cases. MR protocols are presented in Appendix B.
MRI is primarily done in the axial plane, almost always parallel to the mandibular body. The axial images are the mainstay for interpretation. Coronal acquisitions may be done selectively whenever there is a complex relationship between the pathology and the floor of the mouth, tongue base, spaces of the suprahyoid neck, mandible, and skull base. Sagittal images are only occasionally useful or necessary, mainly to show spread of cancer and other pathology from the tongue base to the pre-epiglottic space or suprahyoid neck or for the soft palate pathology relationship to the midline hard palate and nasopharynx.
Pros and Cons
CT and MR are used for the majority of imaging in the oropharynx. Plain radiographs, orthopantomography, and occlusal views remain useful adjuncts for studying the teeth and mandible as discussed in Chapter 96. Dental-related artifacts can seriously degrade both CT and sometimes MR images through the mid oropharynx. This problem is generally worse on CT. The problem is accentuated on MRI when fat suppression is used. MRI is frequently significantly degraded by jaw and other motion as discussed in Chapters 1 through 3.
Ultrasound has a very limited, if any, role in oropharyngeal pathology. It has been used occasionally to evaluate tonsillar and potential retropharyngeal abscesses, but that practice has largely given way to CT in these usually acute, painful conditions in less than cooperative children.
Angiography is used occasionally in both diagnosis and treatment settings. Catheter angiography is necessary if angioarchitecture and temporal flow dynamics of a lesion or an active leak are in question. If not, then computed tomographic angiography and/or MR angiography will usually suffice, especially with the advent of 320 MDCT or its technical equivalent. Angiography is almost always used following imaging studies, although it is occasionally the primary examination for conditions such as intractable bleeding or as prelude to endovascular procedures.
Radionuclide studies, particularly single photon emission computed tomography (SPECT) gallium and bone scanning, are useful in highly selected cases of infectious disease. Fluorine-18 2-fluoro-2-deoxy-D-glucose positron emission tomography (FDG-PET) is used selectively in cancer patients. It should not be used routinely, as it will most often not alter management decisions or outcome. Specific radionuclide technique depends on the indications; this is discussed elsewhere and in general in Chapter 5.
Specific Areas of Interest
Developmental Abnormalities
Potentially cystic congenital lesions that primarily arise outside the oropharynx with potentially complex relationships to the floor of the mouth and deep spaces of the suprahyoid neck or even potential central nervous system connections are very effectively imaged with MR—especially in children, where one would like to limit exposure to ionizing radiation.
If MRI, CT, or the clinical evaluation suggests a venolymphatic or other vascular malformation, then angiography may be done to confirm this impression for potential high-flow lesions and is used to direct endovascular or direct injection as part of therapy. Such treatment may be definitive or an adjunct to surgical removal.
Inflammatory Disease
Complex inflammatory parapharyngeal disease, such as that associated with a high likelihood of associated abscess or when the source of the inflammation is uncertain, is studied with contrast-enhanced computed tomography (CECT) since dental disease and tonsillar pathology are very common sources of such pathology. MRI may be used very occasionally as a supplemental study.
Staging of Known Oropharyngeal Cancer and Related Regional Lymph Node Metastases and Evaluation of Masses of Uncertain Etiology
Both CT and MR can be used to demonstrate the presence, possible nature, and extent of a mucosal or submucosal mass lesion. In most cases, a CT study is usually adequate for all of these tasks. A variety of sometimes unusual lesions, either benign or malignant, can be encountered in this clinical context. As the initial biopsy results may be inconclusive or negative, MR may be used in an attempt to further characterize the lesion. In young patients, MR might be preferred because it does not use ionizing radiation.
Both CT and MR can supply information needed by the clinician for optimal treatment planning in known cancers. CT has a number of important advantages. The CT studies are much easier to execute and are much more reproducible than MRI because of the short data acquisition time that results in less image motion degradation. MDCT systems also now offer high-quality multiplanar imaging with the image quality equal to or exceeding that of multiplanar MR images when the superiority of bone-related information on CT is factored into this comparison. The evaluation of bone on CT is far superior to that on MRI. CT detects calcifications better than MRI. Also, CT is better and easier to perform and interpret than MRI with regard to the extent of metastatic adenopathy. Supplemental MRI is occasionally necessary in patients with tumors whose extent cannot be fully appreciated by a combination of the clinical examination and CECT; this occurs most often due to dental-related artifacts on initial CT studies. The MR in these cases is usually focused on clarifying specific issues that may critically alter patient management, including but not limited to (a) depth of invasion, (b) nature of an atypical mass lesion, and (c) presence and extent of perineural disease.
The qualities described in the previous paragraph make CT preferable for surveillance imaging including early detection of tumor recurrence and/or treatment complications such as osteoradionecrosis of the mandible. Problems such as osteonecrosis are more confidently diagnosed based on the CT pattern of disease as discussed in Chapter 21. Moreover, osteonecrosis due to radiation may mimic recurrence clinically; with MR, early bone invasion as a sign of actual tumor recurrence or persistence may go unnoticed. Recent developments in MRI, such as diffusion-weighted MRI and perfusion imaging, may increase the role of this imaging modality in cancer treatment decision making and surveillance imaging in future.2–4
FDG-PET should play a selective role but not a primary role in oropharyngeal cancers. It is most useful in looking for recurrence after treatment.
If MRI, CT, or the clinical evaluation suggests a vasoformative lesion or highly vascular tumor, then angiography may be done to confirm this impression. In the rare hypervascularor vascular-origin lesions, endovascular therapy may be used as a definitive treatment or adjunct to surgical removal.
Trauma
CT has replaced plain films for evaluating patients at risk or with complex injuries. Plain films may be used for confirmation of hardware placement and uncomplicated follow-up.
Controversies
There is some limited debate with regard to whether CT or MR should be the primary imaging tool for evaluating patients with oropharyngeal cancer. This discussion sometimes emphasizes which study is best at showing bone involvement. CT is far better than MRI at showing all stages of bone invasion except for unusual cases of spread within the marrow cavity. In the vast majority of cases, the bone information from imaging must exclude invasion with a high degree of confidence. That anatomic imaging study must then determine the amount of invasion precisely. MRI is not optimally suited to these tasks, as discussed in Chapters 1 through 3 and 21.
The nature of oropharyngeal cancer is that the area of bone destruction as seen on CT almost always geographically corresponds to the tumor involvement of the marrow cavity of the mandible or the discrete cortical defect that is visible along the posterior maxilla or border of the hard palate. It is only under unusual circumstances that the spread of cancer within the marrow space goes beyond the zone of obvious bone destruction seen on CT; thus, supplemental MRI for mandibular marrow space spread is only very infrequently or rarely necessary. The deficiencies of MR in this regard should obviate the use this imaging as the primary diagnostic study for oropharyngeal cancer in a rational practice of head and neck radiology unless CT is done whenever the primary approaches bone as seen on MRI. This still fails to address the competitive advantage of CT in evaluating regional nodal disease.
The standard or “routine” use of FDG-PET in head and neck cancer remains not yet clearly evidenced based, although its use is common. FDG-PET should be used with discernment by carefully considering its likelihood of contributing to medical decision making that might significantly alter the plan of therapy and/or improve patient outcome in any individual case.
NORMAL ANATOMY
General Description
The oropharynx begins at the anterior tonsillar pillars to its inferior limit at the pharyngoepiglottic folds. It is limited by the soft palate superiorly (Fig. 190.1A–C). The anterior and posterior tonsillar pillars surround the palatine tonsils (Fig. 190.1); the sulci between the lateral oropharyngeal wall and tongue base are known as the glossotonsillar sulci (Fig. 190.1A–D,G). The posterior third of the tongue, known best as the tongue base, begins at the level of the circumvallate papillae and extends to the valleculae (Fig. 190.1A–D,G,H). The mucosa of the valleculae and that of the lingual (anterior) surface of the epiglottis free margin is then in the oropharynx (Fig. 190.1A–C,H). Note that according to the current American Joint Committee on Cancer and International Union Against Cancer manuals of cancer staging, the entire epiglottis (including its free margin) is counted as a laryngeal structure; this has consequences regarding cancer staging.
The anatomy of the oropharynx as seen on CT or MRI is best organized into superficial and deep components. Its superficial morphologic features are formed by mucosal reflections over lymphatic tissue aggregates such as the lingual and palatine tonsils and muscle bundles that surround this part of the upper aerodigestive tract (Fig. 190.1). The deep morphologic features include the parapharyngeal spaces, carotid sheath, deep musculature, and other intervening tissue spaces, which are described in detail in Chapters 142 and 175. The surface structures show significant variation on images among individuals and from side to side in any particular person. This contrasts well with the deep anatomy that is much more constant in appearance both between patients and from side to side in individual patients.5
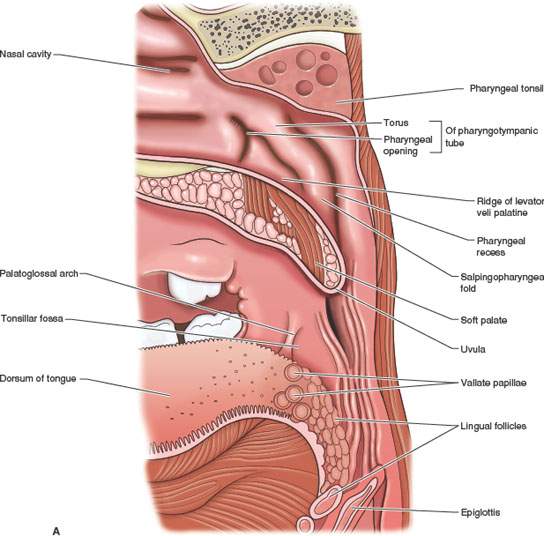
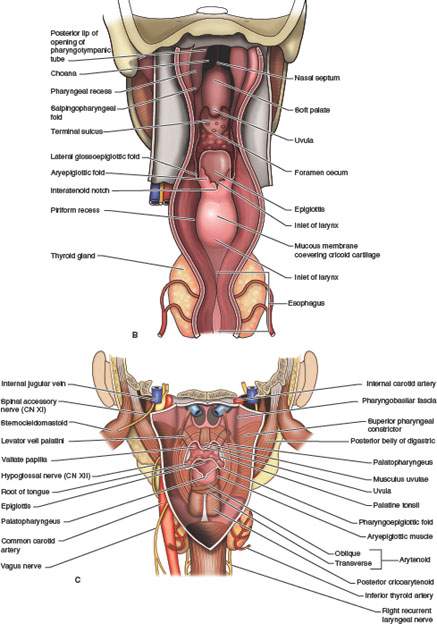
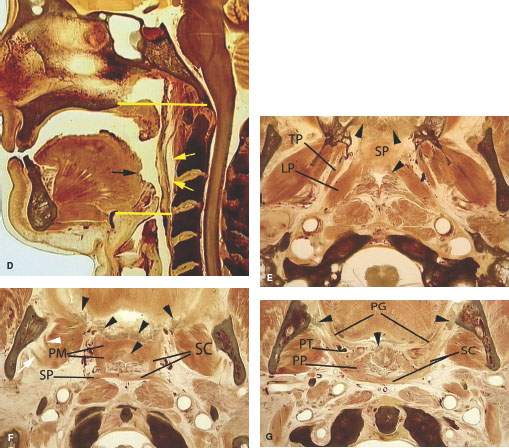
FIGURE 190.1. A series of anatomic diagrams and whole organ sections defining the limits of the oropharynx and important anatomic relationships in this region. A, B: Anatomic diagrams depicting the mucosal and related muscular layers of the oropharynx. Within each portion of the pharynx, there are signature anatomic landmarks that can be readily recognized on sectional images through this ever-changing anatomy; mucosal landmarks are emphasized in (A), while often-related musculature is shown in (B). C: This depiction of the pharynx shows it as essentially a muscular tube suspended from the skull base opened anteriorly to the nasal cavity, oral cavity, and larynx but kept functionally separate from those organ systems. D: Sagittal whole organ section showing the limits of the oropharynx as it extends from the point where the soft palate apposes the pharyngeal wall during swallowing and the vallecula inferiorly (yellow lines). The potential retropharyngeal space is shown by yellow arrows. The approximate of the foramen cecum is shown by the black arrow. The foramen cecum along with the row of circumvallate papillae marks the junction of the oral tongue and tongue base. E: Whole organ section at the lower nasopharynx junction with the oropharynx. The prominent landmark at this level is the soft palate (SP). Numerous minor salivary glands are present in the soft palate and submucosal within the lateral walls of the pharynx (black arrowheads). The tensor (TP) and levator (LP) muscles of the soft palate are important landmarks throughout the nasopharynx and at the junction of the nasopharynx and oropharynx. F: A whole organ section at the level of velopalatal closure, which is the physiologic boundary of the nasopharynx and oropharynx. The muscular boundary at this level is referred to as the Passavant muscle. In reality, that “muscle” is a sphincterlike zone composed of separate muscles that include the palatal muscles (PM), the superior constrictor muscle (SC), and the stylopharyngeus muscle (SP). From the diagram, it can be seen how contraction of these muscles in a coordinated way would act like a sphincter since they essentially border the entire airway at this level. Also note the extensive minor salivary glands present in the soft palate and anterior tonsillar pillars (black arrowheads). At this level, there is also a splitting of the mandibular division of the trigeminal nerve into its two major branches: the lingual nerve (white arrowhead) and the inferior alveolar nerve (white arrow). G: A whole organ section made through the upper oropharynx at the level of the palatine tonsils. The purpose of this illustration is to emphasize the relationship of the tonsils and tonsillar pillars to surrounding structures. At this level, the superior constrictor muscle (SC) surrounds the airway posteriorly and laterally. The posterior tonsillar pillar is formed by the palatopharyngeus (PP) muscle. The anterior tonsillar pillar is formed by the palatoglossus (PG) muscle. The palatine tonsils (PT) lie between the two pillars. As seen in this diagram, the palatine tonsils frequently have cystic zones and areas of dystrophic calcification. This section includes the level of the retromolar trigone, and there is minor salivary gland tissue adjacent to the bone of the retromolar trigone as well as within the uvula of the soft palate (black arrowheads). H: A whole organ section to emphasize the anatomy of the upper tongue base and the glossotonsillar sulcus and related lymphoid and glandular tissue. Primary muscular landmarks in the tongue base are the genioglossus muscles (white arrows) and the transverse intrinsic bundles of muscle in the tongue (black arrows). There are minor salivary glands (black arrowheads) just beneath the mucosa of the tongue base. Lymphoid tissue normally lies in the glossotonsillar sulcus and along the tongue base (white arrowheads). These multiple layers of tissues create the layered appearance of the oral tongue and tongue base as seen on computed tomography and magnetic resonance images. I: A whole organ section taken through the vallecula. The major muscular landmark at this level is the geniohyoid muscle (white arrows) and the intrinsic transverse layers of tongue musculature (black arrows). These muscle fibers are intertwined, and there is a variable amount of fat between them, with the amount of fat usually depending on body habitus. Minor salivary glands (black arrowheads) lie below the mucosa and therefore deep to the lingual tonsillar tissue (white arrowheads). The free margin of the epiglottis is the posterior boundary of the vallecula (E). It is at this level that the hypoglossal nerve (CN 12) enters the tongue base lateral to the hyoglossus muscle and the lingual artery enters the tongue base medial to that muscle (LA).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








