Trauma
Femoral neck fracture
Hip dislocation
Atraumatic
Alcoholism
Corticosteroids
SLE
Caisson disease
Coagulopathies
Sickle cell disease
Cushing disease
Gaucher disease
Pancreatitis
Chronic renal failure
Pregnancy
Smoking
Oral contraceptives
Hemoglobinopathies
Clinical Presentation
Atraumatic cases may be asymptomatic and may only be diagnosed when incidentally imaged, e.g., AVN femoral head/s identified during MRI examination for assessment of a pelvic renal transplant. Patients may complain of nonspecific groin pain, worse on weight bearing with progression over time. Larger infarcts may present with more severe pain. Clinical examination demonstrates a decreased range of motion. There is progressive disability with femoral head collapse and secondary degeneration.
Staging
There are multiple staging systems available. The most commonly used are detailed in Tables 12.2 and 12.3.
Table 12.2
Classification of AVN of the femoral head
Stage | Radiograph | Diagnosis | Clinical |
|---|---|---|---|
Stage 0 preclinical | Normal | Biopsy positive | Osteonecrosis suspected when definite disease in contralateral hip |
Stage 1 preradiographic | Normal or subtle loss of clarity trabecular pattern, patchy osteopenia | Biopsy, bone scan, MRIa positive | 50 % sudden pain in groin, limited range of motion |
Stage 2a precollapse | Changes in trabecular pattern, sclerosis may be localized or diffuse, cysts may develop, mixed pattern | Radiograph, bone scan, MRIa positive | Clinical signs persist or worsen over several months |
Stage 2b transition | Flattening, crescent sign (subchondral fracture) | Radiograph, bone scan, MRIa positive | |
Stage 3 collapse | Sequestrum, break articular margin on both sides of the affected bone followed by collapse, normal joint space | Radiograph, bone scan, MRIa positive | Progressive increase and more constant pain, functional incapacity |
Stage 4 osteoarthritis | Osteoarthritis superimposed on a deformed femoral head | Radiograph, bone scan, MRIa positive | Progressive decrease in range motion |
Table 12.3
ARCO classification system 1992
Stage | Imaging | Subdivisions |
|---|---|---|
Stage 0 | Positive biopsy, negative imaging | |
Stage 1 | Positive MRI +/− bone scan, negative radiograph, CT | Lesion location: medial, central, or lateral |
Stage 2 | Radiograph positive: sclerotic/cystic/osteopenia | % femoral involvement |
Stage 3 | Radiograph: crescent sign (subchondral fracture) | Head a <15 % b 15–30 c >30 % |
Stage 4 | Radiograph: flattening of the femoral head | |
Stage 5 | Radiograph positive: flattening of the femoral head and osteoarthritis | Depression femoral head when fracture present (stages 4 and 5) a <2 mm b 2–4 mm c >4 mm |
Stage 6 | Complete joint destruction |
Imaging
Radiographs (Fig. 12.1)
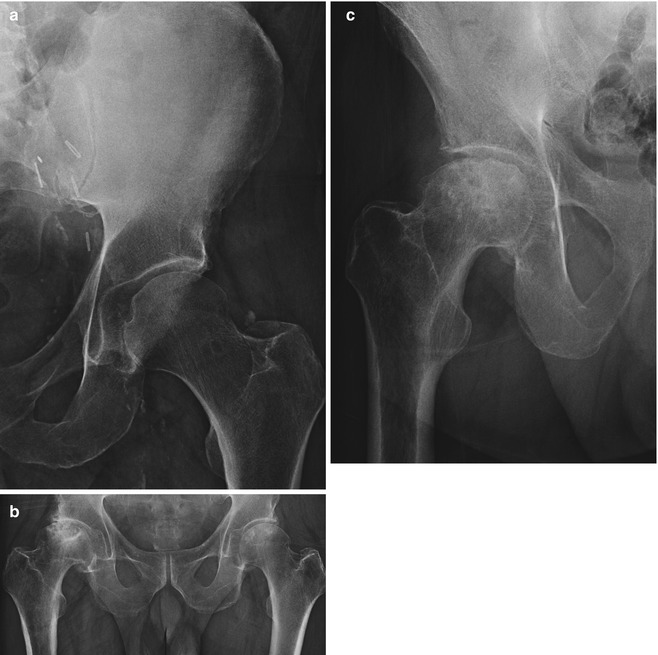
Fig. 12.1
(a) Modified AP radiograph of the left hemi-pelvis, surgical clips related to renal transplant, left hip pain, generalized osteopenia, no radiographic changes AVN, stage 1 AVN. (b) AVN of bilateral hips on AP radiograph, stage 4. The right hip demonstrates partial collapse of the femoral head and secondary degenerative changes, stage 2a; the left femoral head demonstrates localized sclerosis in a patient on long-term steroids. (c) AP radiograph of the right hip with stage 3 AVN, with collapse of the femoral head with maintenance of joint space. See Table 12.2 for detailed description of the staging of AVN
Radiographs may be normal or demonstrate only subtle changes. Radiographs have a low sensitivity in early disease. In patients with suspected AVN, MRI is advised.
Early changes include patchy osteopenia and loss of clarity of the trabecular pattern. This progresses to areas of ill-defined sclerosis. The subchondral region should be closely evaluated for development of a lucent line, the “crescent sign,” a subchondral fracture that heralds impending collapse. The convex outline of the femoral head should be maintained; any loss of convexity or flattening indicates early collapse. Collapse progresses with deformity of the femoral head and development of secondary degenerative changes such as joint space loss, osteophytes, subchondral sclerosis, and cyst formation. These latter changes may be more evident on the acetabular aspect of the joint as the femoral head collapses. Radiographic findings are detailed in Table 12.2.
MRI (Figs. 12.2, 12.3, 12.4, and 12.5)
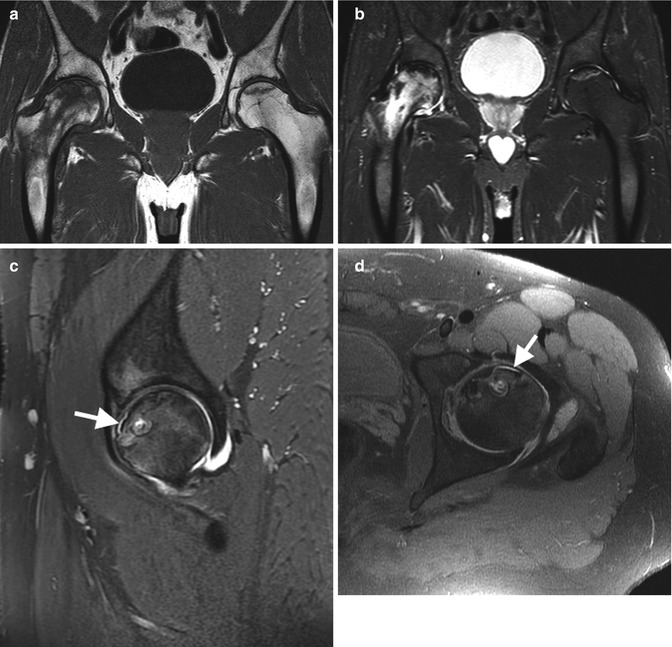
Fig. 12.2
(a, b) Cor T1 and T2FS, respectively, demonstrate bilateral AVN and chronic AVN of the left femoral head (note the double-line sign and acute AVN of the right femoral head with extensive bone marrow edema and small joint effusion). (c, d) Sag and axial T2FS, respectively, in a different patient, with subchondral fracture line (arrow), linear high signal intensity, and early cortical collapse

Fig. 12.3




(a) AP radiograph of the left shoulder demonstrating AVN of the humeral head, stage 2b, in a patient with Crohn’s disease. (b) Corresponding Cor T2FS MRI. (c) 6 years later, AP radiograph, stage 3 AVN. (d) AVN of the right humeral head in a different patient with subchondral fracture (black arrows) and early collapse with flattening cortical margin
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree