, Joon Woo Lee1 and Eugene Lee2
(1)
Department of Radiology, Seoul National University College of Medicine, Seoul National University Bundang Hospital, Seongnam, South Korea
(2)
Department of Radiology, Seoul National University Bundang Hospital, Seongnam, South Korea
7.1 Epidural Abscess
7.2 Arachnoid Cyst
7.3 Arachnoiditis
7.4 Cysticercosis
7.5 Discal Cyst
7.6 Echinococcosis
7.14 Facet Synovial Cyst
7.15 Tuberculosis
7.15.1 Illustrations: Tuberculosis
7.1 Epidural Abscess
- 1.
Epidemiology
All age groups (peak incidence: 6th~7th decade)
M > F: 1: 0.56
0.2–2.8 cases per 10,000
- 2.
Location
Posterior (80%) and anterior (20%) epidural space
Lower thoracic and lumbar > upper thoracic and cervical
- 3.
Characteristic imaging findings
Peripherally enhancing fluid collection
Findings of spondylodiscitis with homogenous or heterogeneous enhancing phlegmon
Diffusion restriction (high signal on DWI, low signal on ADC map)
- 4.
Spectrum of imaging findings
Diffuse dural enhancement in extensive spinal epidural abscess
Spinal cord signal change due to compression, ischemia, or direct extension of infection
Enhancing prominent anterior epidural or basivertebral venous plexus adjacent to abscess
- 5.
Differential diagnosis
Herniated intervertebral disc (extruded or sequestered)
Adjacent parent disc degeneration or combined Herniated intervertebral disc
Iso to low signal on T2-weighted image
Intact vertebral endplate
Epidural hematoma
Heterogeneous high signal on T2-weighted image
Iso signal (acute stage) and high signal (subacute to chronic stage) on T1-weighted image.
7.1.1 Illustrations: Epidural Abscess

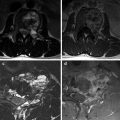
Fig. 7.1
Epidural abscess in a 71-year-old woman. T2-weighted axial MR image (a) shows a well-defined cystic mass-like lesion in the left posterior epidural space (white arrow). This lesion shows strong peripheral contrast enhancement with adjacent phlegmon formation (black arrow) on contrast-enhanced T1-weighted MR image (b). Additional diffuse signal change and enhancement of the bone marrow; paravertebral and bilateral psoas muscles are also noted

Fig. 7.2
Epidural abscess in a 74-year-old man. Postoperative lumbar spine MRI (a) reveals a right anterior epidural lesion with T2-hyperintensity (white arrow) at the level of L4 vertebral body. Peripheral enhancement was noted on sagittal and axial fat-saturated contrast-enhanced T1-weighted MR images (b, c)
7.2 Arachnoid Cyst
- 1.
Epidemiology
Any age
- 2.
Location
Extradural: posterior or posterolateral lower thoracic spine
Intradural: dorsal mid-thoracic spine
Anterior: uncommon
- 3.
Characteristic imaging findings
Well circumscribed, oval, elongated
Dumbbell shape: extension to neural foramen, bony canal expansion
CSF signal on T1- and T2-weighted image
No enhancement
- 4.
Spectrum of imaging findings
Cyst wall can be seen on extradural arachnoid cyst.
Low signal flow artifact on T2-weighted image.
Syringohydromyelia: may result from partial obstruction of CSF by arachnoid cyst.
- 5.
Differential diagnosis
Idiopathic spinal cord herniation
Upper to mid-thoracic level
Focal cord atrophy and ventral deviation to dural defect
Schwannoma
Heterogeneous T2 signal intensity with enhancing peripheral wall
Pseudomeningocele
Dural ectasia
Diffuse dilatation of thecal sac without cord distortion
7.2.1 Illustrations: Arachnoid Cyst

Fig. 7.3
Dorsal intradural arachnoid cyst in a 65-year-old woman. T2-weighted sagittal MR image (a) shows a focal cystic mass-like lesion with cord compression at T2 vertebral body level (white arrow). The lesion shows similar signal to CSF. On the axial scan (b), there is no evidence of herniated spinal cord outside the dura nor rotation of the spinal cord. Absence of CSF flow artifact is also noted

Fig. 7.4
Dorsal extradural arachnoid cyst in a 50-year-old man. T2-weighted sagittal (a) and axial (b, c) MR images show a well-defined cystic mass in the dorsal epidural space with dural sac and spinal cord compression. CSF flow artifact is noted (black arrow) inside the cystic mass. There is no definite solid portion with a relatively thick wall. CT myelography (d) clearly shows a dorsal dural defect at the left side (white arrow) with contrast media communicating between the subarachnoid space and cystic mass
7.3 Arachnoiditis
- 1.
Epidemiology
No gender prediction
Uncommon
6–16% of postoperative patients
- 2.
Location
Lumbar spine (especially cauda equina)
- 3.
Characteristic imaging findings
Intrathecal clumping of nerve roots causing enlarged cord
“Empty sac” appearance with peripheral nerve roots clumping to dura
Pseudomass filling the central portion of the thecal sac
Minimal to mild pial and dural enhancement
- 4.
Spectrum of imaging findings
Type 1: central nerve root clumping with only 2–3 nerve roots
Type 2: peripheral nerve root clumping, central CSF without nerve root (empty thecal sac sign)
Type 3: soft tissue mass filling most of the thecal sac, obliteration of subarachnoid space
- 5.
Differential diagnosis
Cauda equine neoplasms
Large nerve sheath tumor
Myxopapillary ependymoma
Paraganglioma
Carcinomatous meningitis
Intradural metastasis
7.3.1 Illustrations: Arachnoiditis

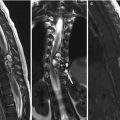
Fig. 7.5
Adhesive arachnoiditis in a 52-year-old woman. The patient has a history of endometrial cancer and underwent hysterectomy and CCRT. T2-weighted sagittal MR image (a) shows a large pseudomass filling the thecal sac in the lumbar spine. On the contrast-enhanced T1-weighted sagittal MR image (b), there is no definite enhancement of the central cystic portion. T2-weighted axial MR images show peripheral nerve root clumping (c) with central CSF flow artifact (d)
7.4 Cysticercosis
- 1.
Epidemiology
Most common worldwide parasitic infection
- 2.
Location
Parenchymal, leptomeningeal, intraventricular, and spinal
Rare spinal cysticercosis
- 3.
Characteristic imaging findings
Intradural cyst with evidence of similar lesion in the brain
Cyst with “dot” appearance
Subarachnoid
CSF signal cystic lesion, variable mass effect to cord and cauda equina
Peripheral cyst enhancement
Intramedullary
Focal cystic lesion with diffuse cord edema with or without syrinx
Peripheral cyst enhancement
May show only nonspecific sheet-like enhancement of subarachnoid space, cord pial surface
- 4.
Spectrum of imaging findings
Vesicular stage
CSF signal intensity.
Scolex appears as a high intensity nodule within the cyst: “hole-with-dot” pattern.
Colloidal stage
Thick, hypointense cyst walls, varied perilesional edema
Granular nodular stage
Areas of signal void on both T1- and T2-weighted images surrounded by edema or gliosis
Final involution stage
Calcified cysticerci: small hypointense area
- 5.
Differential diagnosis
Pyogenic abscess
Arachnoid cyst
Echinococcosis
Granulomatous osteomyelitis
Tuberculosis
Sarcoidosis
7.4.1 Illustrations: Cysticercosis

Fig. 7.6
Cysticercosis in a 47-year-old woman. T2-weighted (a) and contrast-enhanced T1-weighted (b) MR images show an intradural cystic mass with mild peripheral enhancement at L5 vertebral level (white arrows). There are multiple small calcifications in the CSF space at both frontal convexities on the gradient echo brain MR image (c) suggesting calcified cysticerci
7.5 Discal Cyst
- 1.
Epidemiology
Extremely rare
M >> F
- 2.
Location
L4/L5: most common
- 3.
Characteristic imaging findings
Minimal degeneration of the involved disc
Ventrolateral extradural cyst attached to a lumbar disc
Cyst containing bloody-to-clear serous fluid
Low signal on T1, high signal on T2 with cyst wall enhancement
- 4.
Spectrum of imaging findings
Occasional extension into the lateral recess
- 5.
Differential diagnosis
Ganglion or synovial cyst
Perineural cyst
Epidural abscess
Extradural arachnoid cyst
Peripheral nerve sheath tumor with cystic degeneration
7.5.1 Illustrations: Discal Cyst

Fig. 7.7
Discal cyst in a 29-year-old man. T2-weighted (a) and T1-weighted (b) sagittal MR image shows a 12 mm cystic lesion with a thin peripheral rim at L4 vertebral body level. T2-weighted axial MR image (c) shows that the cystic lesion is located in the anterior epidural space (right subarticular zone) with right L4 nerve root compression. On the contrast enhancement T1-weighted images (d, e), the cystic lesion shows peripheral enhancement without a definite solid portion
7.6 Echinococcosis
- 1.
Epidemiology
Any age
M = F (no gender predilection)
Disease caused by cyst stage of infestation by tapeworm Echinococcus spp.
- 2.
Location
Liver, lung involvement most common
Bone: 0.5–4%
Spine involvement in 50% of cases
Thoracic (50%), cervical (10%), lumbar (20%), sacrum (20%)
Extradural
Intradural extramedullary: rare
Intramedullary: extremely rare
- 3.
Characteristic imaging findings
Multiloculated multi-septated, T2 high signal intensity mass in vertebral body/posterior elements
Epidural extension with cord compression
Minimal or no contrast enhancement
Multiloculated osteolytic mass on CT
- 4.
Spectrum of imaging findings
Degenerated cyst
Iso signal to muscle on T1-weighted image
Low signal relative to CSF on T2-weighted image
- 5.
Differential diagnosis
Cystic metastasis (renal cell or thyroid carcinoma)
Cysticercosis
Primary bone tumor
Osteosarcoma
Chondrosarcoma
Aneurysmal bone cyst
Giant cell tumor
Chordoma
7.7 Extramedullary Hematopoiesis
- 1.
Epidemiology
More common in adults (3rd~4th decade)
Hemoglobinopathy
Sickle cell disease: African-Americans
Thalassemia: Eastern Mediterranean population
Myeloproliferative disease
- 2.
Location
Mid-thoracic > cervical, lumbar
Epidural, paravertebral
Multi-segmental
- 3.
Characteristic imaging findings
Minimally enhancing isointense thoracic intra- or paraspinal masses with associated diffuse marrow hypointensity
Well-circumscribed, homogenous, and lobular soft tissue mass
Iso signal (to spinal cord) on T1-weighted image
Iso to high signal (to spinal cord) on T2-weighted image
Diffuse vertebral marrow low signal on T1-weighted image
- 4.
Spectrum of imaging findings
Low signal on T2-weighted image due to increased iron content in hematopoietic tissue
Variable contrast enhancement
Variable spinal cord or nerve root compression
- 5.
Differential diagnosis
Spinal epidural lymphoma
Intense homogenous enhancement on Gd
Adjacent vertebral involvement
Epidural or paraspinal metastasis
Extension from adjacent vertebral lesions
Epidural hematoma
Peripheral nerve sheath tumor
Often single level
Widening of intervertebral foramen
Multiple neurofibromas with neurofibromatosis type 1
7.7.1 Illustrations: Extramedullary Hematopoiesis


Fig. 7.8




Extramedullary hematopoiesis in a 48-year-old man (known hereditary spherocytosis). Chest CT scan (a) shows a well-defined soft tissue mass in the right paravertebral space at T8 vertebral level (white arrow) with increased uptake on PET CT scan (b). This lesion shows T1-hyperintensity with mild inhomogeneous enhancement (c, d). T1-weight sagittal MR images (e, f) show diffuse bone marrow signal decrease in the axial skeleton without definite enhancement indicating an underlying bone marrow replacement disease
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree