Fig. 20.1
The figure demonstrates the MRI findings of an 80-year-old male patient, initially presenting with recurrent abdominal pain and pain in the upper lumbar spine from lumbar vertebrae L1 to L3 without neurological deficit. (a) The T2-weighted axial MRI shows multiple small hyperintense lesions in the right psoas muscle (arrows). The corresponding fat-suppressed T1-weighted image after gadolinium administration (b) confirmed the diagnosis of a multicystic mass and delineated the thickened, contrast-enhancing septations around the cystic components (arrow). T1-weighted image (c) and T2-weighted STIR image (d) of the lumbar spine show the bone marrow replacement within the first, second, and third lumbar vertebrae (arrows). The lesions comprise of cystic and solid components
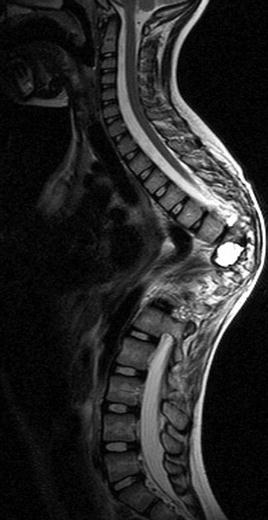
Fig. 20.2
The figure presents the MRI of a 6-year-old girl with primary Echinococcus granulosus infection of the spine being treated with various interventions. Now presenting recurrence of infection due to incomplete cyst resection and inappropriate surgical measures causing progressive kyphoscoliotic deformity, spinal stenosis, cord compression, and neurologic injury. At the presentation at our institution, she was wheelchair bound. The clinical investigation revealed gibbus in the middle thoracic spine with a Cobb angle of 110°, cord compression at the apex, and paraplegia with Frankel Grade C
Localization
The outcome of hydatid disease significantly depends on the location of the lesions. In this context the classification of Braithwaite and Lees provides an initial reference for the expected outcome (Braithwaite and Lees 1981). According to their anatomic location, cysts can be divided into intramedullary, intradural-extramedullary, extradural, spinal (vertebral), and paraspinal lesions extending into spinal structures. Besides these anatomic references, especially the spinal level influences the neurologic outcome. There is a remarkable difference regarding the outcome between cervical, thoracic, lumbar, and sacral manifestations of the spinal hydatid disease, especially in advanced stages when irreversible nerve tissue damage exists.
Aftercare
Surgical decompression and chemotherapy are the principal forms of treatment in pediatric and adolescent cases of spinal hydatidosis. Unfortunately even with extensive surgery, results are far from being curative. The recurrence and mortality rates for intraspinal hydatid disease range up to 50 and 15 %, respectively (Taratuto and Venturiello 1997; Toussaint et al. 2001; Wang et al. 2009). Up to 40 % of patients are reported to have recurrent symptomatology within 2 years after the initial operation (Spies et al. 2008; Takci et al. 2008; Taghipoor and Razmkon 2009). As the recurrence rate is high, adjuvant anthelmintic agents are recommended following surgery. Anthelmintic drugs are strongly recommended in case of recurrence, systemic disease, intraoperative rupture or puncture, poor suitability for surgery, and prophylaxis (Papagelopoulos et al. 1997; Schnepper and Johnson 2004; Romig 2009; Sharma et al. 2011). However, a clearly structured aftercare and follow-up calendar including physical examination, imaging, as well as serologic testing is mandatory. In parallel to the aftercare of soft tissue sarcoma, we recommend restaging every 3 months for the first 2 years. This should include CT scans of the abdomen and MRI of the spine. In the following the intervals can be reduced to twice a year up to year 5 and once a year until year 10 after onset of the disease.
The imaging features of intraspinal hydatid cyst usually comprise multiple spherical lesions with clearly defined borders, containing fluid with similar CSF intensity on both CT and MRIs. Though, due to the need for repetitive scanning on a regular basis, we regard MRI for several reasons as the best imaging technique, since it allows early diagnosis of spinal cord compression and more accurate localization of intra- and paraspinal manifestation if multiplanar images are acquired. On MRI it is possible to detect the exact anatomical location of the lesion and to show the viability of the hydatid cysts. On T2-weighted images, a cystic lesion has a high intensity, and a decrease in signal indicates a necrotic cyst. Thus, a decreased signal in this sequence is a characteristic indicator of a necrotic cyst. Furthermore, the layers of the cyst can only be demonstrated by MRI, and the pericyst may show enhancement after contrast material administration due to its rich vascularization. In particular positron emission tomography scanning in combination with CT scan or MRI might show active lesions at a time when clinical symptoms are absent or unspecific and recurrence of parasitic tissue is not detectable by conventional imaging (Brunetti et al. 2010). Imaging of spinal hydatid disease is discussed in Chap. 12.
Blood tests should include benzimidazole blood levels as well as serological tests (Nell et al. 2011). Determination of benzimidazole blood levels, 4 h after the morning dose, is recommended 1, 4, and 12 weeks after initiating drug therapy. Detection of antibody directed to echinococcal polypeptide antigens has the highest degree of specificity. Enzyme-linked immunosorbent assay (ELISA), indirect hemagglutination, and complement fixation tests are reported to be 80–100 % sensitive and 88–96 % specific in abdominal disease. However, the sensitivity decreases abruptly to 25–56 % in extrahepatic disease which limits their use in the diagnosis or follow-up for primary bone disease. Second-line tests like immunoblotting (antigen 5 precipitation: arc-5 test) may be used for confirmation after ELISA and hemagglutination. Laboratory findings of patients with spinal hydatidosis are discussed in Chap. 10.
Benzimidazole Treatment
Albendazole should be administered orally at a dose rate of 10–15 mg/kg/day divided into two doses (WHO 1996). In practice a daily dose of 800 mg is applicable to adults. Intermittent or cyclic treatment is no longer necessary, since albendazole treatment is well tolerated and it has been reported that a dose rate of 20 mg/kg/day is tolerated for up to 5 years. Alternatively if albendazole is not enough tolerated or available, mebendazole could be administered at a daily dose rate of 40–50 mg/kg/day. Benzimidazoles are generally well tolerated. Adverse reactions include hepatotoxicity, alopecia, gastrointestinal disturbances, and leucopenia (Vuitton 2009). Moreover the only contraindication for benzimidazoles is pregnancy. Albendazole is the most widely used benzimidazole worldwide. Benefits of albendazole are a better bioavailability to achieve higher plasma levels, an easy administration, and an overall better efficacy. However, benzimidazoles in general are only parasitostatic and do not erase E. multilocularis metacestodes.
Cystic Echinococcosis
Neurological Deficit
The neurological and orthopedic symptoms can often be reduced or eliminated by surgery and/or anthelmintic treatment for a certain time, but very often only a short follow-up is reported, and it remains doubtful if the patient was cured (Arif and Zaheer 2009; Kotil et al. 2010; Thaler et al. 2010; Scarlata et al. 2011). In recurrent cases multiple interventions can be reasonable to preserve or even improve the spinal stability and the neurological status, but cure of disease is usually not possible (Keller et al. 1997).
Treatment Characteristics
Benzimidazole treatment is recommended for a period of at least 3 months. Although these drugs are well tolerated, Pamir et al. (1984) do state that there is no clear evidence that further administration is lowering the recurrence rate. Nevertheless, Turgut (1997) report that the drugs could effectively keep the disease asymptomatic for a prolonged time.
Several authors stress that imaging should not be the only means for diagnosing a recurrent disease, because a residual cavity is very hard to differentiate. In this regard symptoms seem to have a certain impact. Lawn et al. (2004) found that during post-surgical follow-up, the immunoglobulin G subclass IgG2 antibody response provides a reasonable correlate of disease activity, and Nouir et al. (2008) found that immunoblotting can be a useful approach for monitoring posttreatment follow-up.
Recurrence Rate
Recurrence During Anthelmintic Therapy
Conservative treatment seems to be effective and the recurrence rate of conservatively treated patients is significantly lower than the rate of surgically treated patients without chemotherapy. Nevertheless, very often patients present with neurological symptoms that urgently require surgical decompression.
Recurrence After Surgery
Total excision of the cysts should be the aim of treatment, but in the majority of cases, this cannot be obtained and recurrence is reported. Therefore up to 40 % of cases show recurrence within 2 years of initial operation (Turtas et al. 1980). Nevertheless, the excision of intradural and extradural lesions without osseous involvement could theoretically be curative when the cysts remain intact (Bettaieb et al. 1978; Pamir et al. 1984). But in most cases a complete removal of cyst cannot be performed without damaging the nerve roots (Turgut and Turgut 2010). Osseous involvement causes a multivesicular and diffuse infiltration of the vertebrae (Ozek 1994). Due to this fact the surgery at the vertebrae will lead to spillage of the scolices (Baysefer et al. 1996; Islekel et al. 1998). In this context Turgut (1997) were able to show that the recurrence rate of spinal lesions is significantly higher (33 %, n = 41) than the rate of intraspinal lesions without or minor bone involvement (<6 %, n = 27). Both surgery and anthelmintic therapy should be considered. Some authors recommend administering lifelong chemotherapy. Most patients suffer from multiple recurrences, worsening of disease, and very often restoration of the spine to improve and preserve neurological status and spine stability.
Prognosis
The recurrence rate is reported in up to 40 % of all cases, but the recurrence probability for a single case depends very much on the localization of the lesion and in case of a surgery on the progress of the intervention. The literature does provide case reports and reviews, but larger studies on echinococcosis of the spine are scarce. Most publications only report on a period of a few years post operation, and reliable data on, e.g., the survival time for cases with spine affection, is missing.
Alveolar Echinococcosis
Treatment Characteristics
Although postoperative benzimidazole therapy is obligatory in all cases, generally accepted guidelines concerning presurgical anthelmintic treatment and the duration of treatment after surgery are not available. Brunetti et al. (2010) recommended temporary treatment after complete resection. Reuter et al. (2000a, b) require a benzimidazole treatment for a period of at least 2 years post surgery, since residual echinococcosis might remain undetected and follow-up of patients should be at least 10 years. In cases of a subtotal surgery or in inoperable cases, long-term or even lifelong benzimidazole therapy is necessary. Ammann and Eckert (1996




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree