and Clarisse Dromain2
(1)
Department of Radiology, San Giovanni Hospital, Roma, Italy
(2)
Department of Radiology, Institut de Cancerologie Gustav Roussy, VilleJuif – Paris, France
Abstract
Parks classification is a widespread classification system for fistula in ano proposed by Parks in 1976. Parks described four different types of perianal fistula considering the fistulous tract with respect to the anal sphincter complex. Crucial landmarks for this classification are represented by the external anal sphincter and by the levator ani muscle. Four types of fistulas are described by Parks: intersphincteric, transphincteric, extrasphincteric, and suprasphincteric. Parks classification is very useful since different types of fistulas categorized using Parks methods require different surgical approach. Basically the intersphincteric fistula (i.e., the more easy and common fistula) can be treated with surgical fistulectomy, whereas other types of fistulas in whom the fistulous tract involves the external anal sphincter or the levator ani muscle should be treated with surgical drainage by means of seton positioning in order to avoid iatrogenic damage to sphincter complex and possible fecal incontinence.
Parks Classification
Parks classification is a widespread classification system for fistula in ano proposed by Parks in 1976. Parks described four different types of perianal fistula considering the fistulous tract with respect to the anal sphincter complex. Crucial landmarks for this classification are represented by the external anal sphincter and by the levator ani muscle. Four types of fistulas are described by Parks: intersphincteric, transphincteric, extrasphincteric, and suprasphincteric. Parks classification is very useful since different types of fistulas categorized using Parks methods require different surgical approach. Basically the intersphincteric fistula (i.e., the more easy and common fistula) can be treated with surgical fistulectomy, whereas other types of fistulas in whom the fistulous tract involves the external anal sphincter or the levator ani muscle should be treated with surgical drainage by means of seton positioning in order to avoid iatrogenic damage to sphincter complex and possible fecal incontinence.
MRI of the pelvis is very useful in mapping noninvasively the fistulous tract and all possible distant abscess allowing an accurate surgical planning and reducing the rate of fistula recurrence after surgery. However in many centers fistula in ano is imaged by endorectal ultrasound (using dedicated endorectal probe with 3D capabilities). Nevertheless MRI is strongly recommended in Crohn’s disease patients presenting with anal fistula (complex fistulas) in diagnosis as well as in follow-up during medical treatment (infliximab therapy). In this last clinical setting as well as in complex fistulas, in recurrent fistulas, or in case of differential diagnosis between perianal abscess and mucinous tumor of the rectum and anal canal, the i.v. administration of Gd-chelates during MR exam may give additional information to conventional T2-weighted images study.
Pelvic Floor Dyssynergia
Pelvic floor dyssynergia refers to a failure to the normal relaxation of pelvic floor during defecation, leading to obstructed defecation syndrome. MR defecography is able to detect the lack of relaxation of pelvic floor as well as the paradoxical contraction of puborectal muscle when the patient attempts to defecate, leading to the closening of anorectal angle with outlet mechanical pelvic obstruction. Digital examination and anorectal manometry are important tests; however, MR defecography is extremely important in the differential diagnosis with other causes of obstructed defecation syndrome. Therapy of pelvic floor dyssynergia is represented by biofeedback training. Some authors proposed the injection of botulinum toxin type A into the puborectal muscle in conjunction with biofeedback training.
Perforation, GI Tract
Gastrointestinal perforation is a cause of acute abdomen.
Gastrointestinal perforation is defined as a complete penetration of the wall of the stomach, small intestine, or large bowel resulting in intestinal contents flowing into the abdominal cavity. Perforation of the intestines results in the potential for bacterial contamination of the abdominal cavity with peritonitis. Perforation of the stomach can lead to a chemical peritonitis due to leaked gastric acid. Perforation anywhere along the gastrointestinal tract is a surgical emergency. Underlying causes include gastric ulcer, diverticulitis, appendicitis, gastrointestinal cancer, acute mesenteric ischemia, trauma, nonsteroidal anti-inflammatory drugs, and ingestion of corrosives. Perforation may also be iatrogenic during endoscopic procedures (ERCP, colonoscopy) or during abdominal surgery.
Get Clinical Tree app for offline access
CT scan can easily detect also small amount of peritoneal free air as indirect sign of perforation (Fig. 1). However the exact identification of perforation site is less easy. The direct sign of bowel wall defect is not always detectable. While some indirect findings can suggest the site of perforation such as perivisceral focal fat stranding, focal bowel wall thickening or the localized presence of gas bubble surrounding the bowel. The site of free air accumulation is not always associated with the site of perforation because, also in case of sigmoid perforation, air accumulates progressively in the subphrenic space progressively. On the other hand, the presence of air in the retroperitoneal space suggests an extraperitoneal site of perforation (right pararenal space for duodenal perforation).
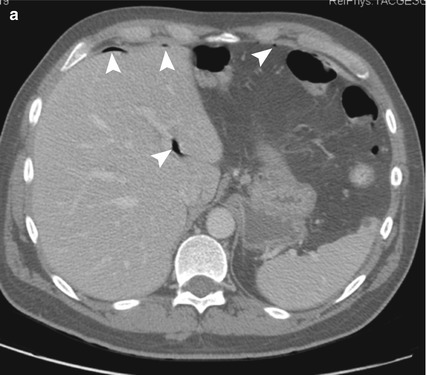

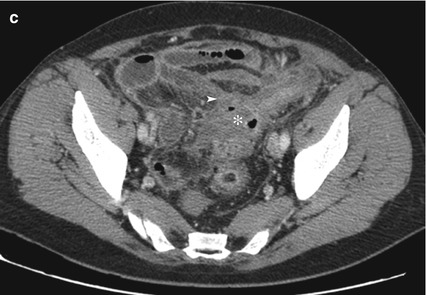
Fig. 1
(a) Shows small amounts of free intraperitoneal parahepatic air using lung windowing. In (b and c), a coronal MPR and axial pelvic scan are shown, respectively, showing sigmoid wall thickening with sign of diverticulitis (asterisk) and ileocolic fistula (arrowhead) and small extravisceral air pocket with associated ileus suggesting the sigmoid colon and complicated diverticulitis as site and cause of perforation, respectively< div class='tao-gold-member'>Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree