and Sofia Gourtsoyianni2
(1)
UOC Radiologia BR, Azienda Ospedaliera Universitaria Integrata Verona, Verona, Italy
(2)
Imaging 2, Level 1, Lambeth Wing St Thomas’ Hospital, London, UK
Pancreas Divisum
The most common anatomical variant of the pancreas, it is caused by failure of the ducts of the dorsal and ventral buds to fuse during embryologic development. The prevalence is between 4 and 15 %.
In the most common classic form of pancreas divisum, the small ventral duct (duct of Wirsung) drains via the major papilla and the large dorsal duct (duct of Santorini) drains via the minor papilla (Fig. 1).
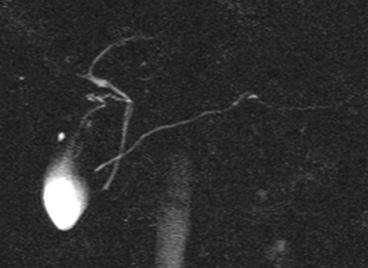
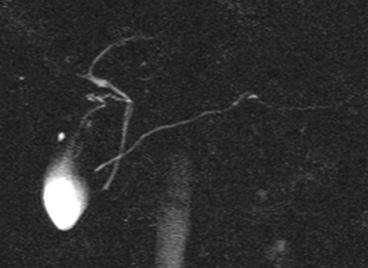
Fig. 1
Pancreas divisum. Coronal thick-slab MRCP image shows the classic form of pancreas divisum, with the large dorsal duct (duct of Santorini) draining via the minor papilla and crossing the choledochus
Other more rare variants include incomplete pancreas divisum, where a small branch connects the ventral and dorsal pancreas, pancreas divisum with nonpatent major papilla, where the entire pancreatic ductal system drains via the minor papilla, and reversed pancreas divisum, where the small dorsal duct drains through the minor papilla, while the large ventral duct drains through the major papilla.
Most patients with pancreas divisum are asymptomatic; however this abnormality is observed more frequently in patients with chronic abdominal pain and chronic pancreatitis than in the general population.
Pancreatoblastoma
Pancreatoblastoma is the most common pancreatic tumour in the paediatric population.
Pancreatoblastoma usually occurs in the 1st decade of life, with a mean age of 4.5 years at diagnosis. There is slight male predilection (1.3:1 to 2.7:1). It can be associated with Beckwith–Wiedemann syndrome.
Patients most commonly present with an asymptomatic, large abdominal mass; less commonly they present with non-specific complaints. Up to 1/3 of the cases have increased alpha-fetoprotein serum levels.
The tumour occurs most often in the head of the pancreas and tends to be large and solitary. Often at diagnosis the tumour is so large that defining its origin from the pancreas is difficult.
CT usually shows a relatively well-defined and heterogeneous mass. The tumour frequently appears multiloculated with enhancing septa. Small calcifications may be present (punctate, clustered or curvilinear).
At MRI, typically pancreatoblastomas have well-defined margins with low to intermediate signal intensity on T1-weighted images and heterogeneous high signal intensity on T2-weighted images. Necrotic areas appear hypointense on T1 weighted.
Local invasion and dissemination to distant organs may occur. Locally advanced tumours are poorly marginated and invade the surrounding pancreas, the peripancreatic tissues and the adjacent organs. Vascular invasion is rare. Liver and abdominal lymph node metastases are present in 35 % of the patients at diagnosis.
Paraduodenal Pancreatitis
Paraduodenal pancreatitis, previously known as groove pancreatitis, is an uncommon type of focal chronic pancreatitis affecting the potential space between the head of the pancreas, the duodenum and the common bile duct, known as the pancreaticoduodenal groove.
It is a rare disease, seen predominantly in males with a history of alcohol abuse; peak incidence is around 40–50 years.
Two forms of groove pancreatitis have been described: the “pure” form, which affects only the groove, sparing the pancreatic head, and the “segmental” form, which involves the pancreatic head with development of scar tissue within the groove.
CT typically shows hypodense tissue in the pancreaticoduodenal groove, which may demonstrate delayed enhancement. Small cystic lesions may be seen along the medial wall of the duodenum, which is thickened. Common bile duct dilatation may be present.
MR imaging may demonstrate a sheetlike mass in the pancreaticoduodenal groove, usually hypointense to the normal pancreas on T1-weighted images, and with variable intensity on T2-weighted image (hypointense, isointense to slightly hyperintense to the normal pancreas). This tissue, similar to what is observed at CT, may show delayed enhancement after gadolinium administration.
The differential diagnosis is different for the pure and the segmental form.
The pure form enters into differential diagnosis with groove carcinoma, duodenal or periampullary carcinoma, neuroendocrine tumours of the pancreatic groove and acute pancreatitis with inflammatory changes in the groove. A differential diagnosis with pancreatic groove carcinoma is hardly possible on the basis of clinical and imaging features alone, although the presence of cystic lesions within the mass or of a thickened duodenal wall would favour the diagnosis of groove pancreatitis.
The most important differential diagnosis for the segmental form is pancreatic adenocarcinoma: the imaging characteristics of these two diseases may overlap considerably, especially for the scirrhous variant of pancreatic adenocarcinoma, which may demonstrate delayed enhancement similar to groove pancreatitis. Vascular invasion is the most useful sign in differentiating pancreatic adenocarcinoma and groove pancreatitis. MRCP also may reveal a smooth stricture of the distal intrapancreatic portion of the common bile duct in case of groove pancreatitis, while the stricture is abrupt and irregular in case of pancreatic carcinoma.
Peliosis Hepatis
Peliosis hepatis is a rare benign disorder with sinusoidal ectasia and small blood-filled lacunar spaces present in the liver parenchyma. It is usually associated with chronic wasting and infectious diseases (TBC, AIDS), malignancies (HCC, metastases), drugs (steroids, oral contraceptives) or post-transplant immunodeficiency conditions.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree