KEY FACTS
Terminology
- •
Solid epithelial neoplasm from ductal epithelium of exocrine pancreas
Imaging
- •
US often 1st-line imaging to evaluate obstructive jaundice and level of obstruction
- ○
Not as sensitive as CT or MR for mass or staging
- ○
- •
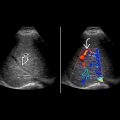
Hypoechoic, infiltrative mass or isoechoic mass with subtle focal contour deformity
- •
Variable size
- •
Pancreatic ductal dilation and bile duct dilation
- ○
Double duct sign: Dilation of both ducts
- ○
- •
Diffuse glandular tumor involvement can be difficult to differentiate from acute pancreatitis
- •
Atrophy or pancreatitis proximal to pancreatic ductal obstruction
- •
Typically hypovascular, but color Doppler may be helpful in assessing vascular encasement or venous obstruction
- •
Displacement/encasement of adjacent vascular structures, determines resectability (as well as metastases)
- •
Liver and regional lymph node metastases
- •
Ascites due to peritoneal metastasis
- •
Endoscopic US used to guide biopsy
Top Differential Diagnoses
- •
Chronic pancreatitis
- •
Other primary pancreatic tumors
- •
Metastases
- •
Lymphoma
Clinical Issues
- •
Mean at onset: 55 years; peak: 7th decade; M:F = 2:1
- •
Usually asymptomatic until late in course: Obstructive jaundice, weight loss
- ○
Pancreatic head tumor presents with obstructive jaundice
- ○
Body or tail tumor presents later with weight loss
- ○
- •
Most commonly presents with distant metastases (~ 65%); least likely to present with tumor confined to pancreas
- •
Poor overall prognosis; 5-year survival rate of ~ 5%
- •
Better long-term survival through complete resection
Scanning Tips
- •
Look carefully at site of transition of dilated bile or pancreatic duct to normal caliber
 in the pancreatic head partially obstructing the common bile duct
in the pancreatic head partially obstructing the common bile duct  and pancreatic duct
and pancreatic duct  . Superior mesenteric vessels are encased
. Superior mesenteric vessels are encased  . Celiac nodes
. Celiac nodes  are present.
are present.
 . There are multiple liver metastases
. There are multiple liver metastases  .
.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree