Grade
Injury
Description
a.
V
Laceration
Massive destruction of the pancreatic head
b.
I
Hematoma
Minor contusion without injury
c.
II
Hematoma
Major contusion without duct injury or tissue loss
d.
III
Laceration
Major laceration without duct injury or tissue loss
e.
IV
Laceration
Proximal transection or parenchymal injury involving the ampulla
6.
What is the most common pancreatic complication after surgical injury repair?
a.
Retroperitoneal abscess
b.
Stenosis of the pancreatic duct
c.
Acute pancreatitis
d.
Pancreatic fistula
e.
Chronic pancreatitis
Answers: 1. a; 2. c; 3. e; 4. c; 5. d; 6: a
18.2 Introduction
Pancreatic trauma is uncommon.
Pancreatic injuries in adults occur nearly exclusively in severe polytrauma.
Source of significant morbidity and mortality.
Blunt pancreatic injury may be overlooked in patients with extensive multiorgan trauma.
Blunt pancreatic trauma occurs when high-energy force is applied to the upper abdomen, crushing the retroperitoneal structures against the vertebral bodies.
The pancreatic injuries secondary to blunt trauma have a spectrum from a minor contusion to complete transection.
18.3 Etiology
In adults about 60 % of pancreatic injuries are caused by motor vehicle accidents and consequent impact with the steering wheel.
In children the most common mechanism is a direct blow to the epigastrium from bicycle handlebars.
In a stab wound, the weapon damages the pancreatic tissue along the tract of injury.
In a gunshot wound, the passage of the projectile and the associated pressure waves cause a wider area of injury.
Isolated pancreatic injuries are rare, because of the proximity of the pancreas to multiple important structures.
After blunt trauma, injuries of the pancreas are commonly associated with injuries of the:
Duodenum, liver, and spleen
After penetrating trauma, concomitant injuries of the:
Stomach, major vascular structures, liver, colon, spleen, kidney, and duodenum
Outcome:
The integrity of the main pancreatic duct is the most important determinant of outcome.
Associated morbidity after pancreatic injuries is 45 %.
If the treatment is delayed, it may increase to 60 %.
A delay in diagnosis of a pancreatic injury associated with duct disruption leads to:
Secondary infections, fistulas, fluid collections, and prolonged stays in the intensive care unit and hospital
18.4 Grading System: Organ Injury Scale (OIS)
Grade 1
Hematoma
Minor contusion without injury
Laceration
Superficial laceration without duct injury
Grade 2
Hematoma
Major contusion without duct injury or tissue loss
Laceration
Major laceration without duct injury or tissue loss
Grade 3
Fig. 18.1
Pancreatic fracture, macroscopic appearance. A 32-year-old male with history of blunt abdominal trauma. Intraoperative photograph shows a complete transection of the body of the pancreas (arrowheads). Note the separation of the pancreatic fragments
Laceration
Distal transection or parenchymal injury with duct injury
Grade 4
Laceration
Proximal transection or parenchymal injury involving the ampulla
Grade 5
Laceration
Massive destruction of the pancreatic head
Practical Pearl
Injuries of the pancreatic head are twice as likely to be fatal as those to the body and tail.
18.5 Clinical Diagnosis
In a patient with trauma from anterior-posterior force vector with deceleration and anterior truncal seat belt mark, the possibility of an aortic, small bowel, as well as pancreatic injury should be considered.
In penetrating abdominal trauma patients, pancreatic injury is more rapidly diagnosed.
While the immediate mortality of blunt pancreatic trauma might not be as high as with penetrating injury, diagnosis and management can present a challenge.
Isolated pancreatic injuries may present with few abnormal physical findings; early diagnosis may be delayed. Abdominal pain is the most common finding.
Most patients with penetrating abdominal trauma associated with hypotension, peritonitis, or evisceration proceed to the operating room without much diagnostic workup.
18.6 Laboratory Evaluation
Serum levels of amylase are neither sensitive nor specific for predicting an injury of the pancreas.
Up to 35 % of patients with complete transection of the main pancreatic duct may have normal serum amylase levels.
If the serum amylase level is abnormal and the patient is hemodynamically stable, further investigation with imaging studies is recommended.
18.7 Imaging
CT and ERCP are the preferred modalities to evaluate patients with suspected pancreatic injury.
The recommended CT phases to evaluate pancreatic injuries are the arterial (20–30 s) and portal (60–80 s) after the administration of intravenous contrast.
CT images should be reconstructed at 3 mm for interpretation, 1.5 mm for multiplanar reconstructions (MPRs), and with 3D post-processing.
18.7.1 Contrast-Enhanced Computed Tomography (CECT) (Figs. 18.2–18.13)
Findings
They are classified as indirect and direct signs.
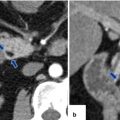
Fig. 18.2
Pancreatic fracture secondary to blunt trauma. A 3-year-old male with history of child abuse. This child was struck in the abdomen 4 weeks prior by his mother’s boyfriend. This patient was complaining of abdominal discomfort and difficulty breathing. At physical examination a prominent abdomen was noted. Photograph of the patient (a) demonstrates a markedly distended abdomen. Supine plain abdominal film (b) demonstrates a large mass displacing the transverse colon inferiorly (arrows). CECT axial (c–f) and coronal (g, h) images demonstrate a pancreatic fracture plane through the neck of the pancreas (e–h) (arrowheads) associated with a very large pseudocyst (c–h) (arrows). Additionally, note the presence of multiple lacerations in the right lobe of the liver (c, d, g, h) (curved arrows). Single-shot fast spin echo T2 weighted axial (i, j) and coronal (k, l) images confirm the presence of a pancreatic fracture (arrowheads) associated with a large pseudocyst (arrows) and the presence of hepatic lacerations. Patient was clinically stable, therefore managed conservatively. Under endoscopy guidance, two plastic stents were placed transgastrically in the large pseudocyst. Supine film of the abdomen (m) demonstrates the two stents placed endoscopically (arrows). Follow-up abdominal ultrasounds (not shown) showed significant decrease in size of the pseudocyst. Patient was discharged 3 weeks after his admission
Fig. 18.3
Pancreatic fracture secondary to blunt trauma on CT. A 19-year-old female with history of blunt abdominal trauma secondary to a motor vehicle accident. CECT axial (a–c) and coronal (d) images reveal a fracture plane in the neck separating the body and tail of the pancreas (c–d) (arrowheads) associated with liver lacerations (a–b) (curved arrows) and multiple fluid collections in the lesser sac and both anterior pararenal spaces (a–c) (arrows). Because the patient was hemodynamically unstable, she was taken to the OR where a distal pancreatectomy and splenectomy was performed
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree