Tommaso Scarabino and Saverio Pollice (eds.)Imaging Spine After Treatment2014A Case-based Atlas10.1007/978-88-470-5391-5_1
© Springer-Verlag Italia 2014
1. Pathology
(1)
Department of Radiology—Neuroradiology, “Lorenzo Bonomo” Hospital, Andria, Bari, Italy
Abstract
Causes of surgery and interventional radiology on spine are represented largely by disk herniation (most commonly lumbar), which we will discuss further in this treatment. Stenosis of the vertebral canal, vertebral instability, and vertebral fractures will also be analyzed [1, 2]. The therapeutic treatment of spinal pathology initially includes conservative therapy and in case of failure a number of surgical procedures and/or interventional radiology approaches, with varying degrees of invasiveness, such as discectomy, vertebroplasty, and surgical stabilization. With recent advances of intervention techniques and devices used, minimally invasive approaches are becoming increasingly popular for the treatment of spine disorders. In particular, minimally invasive spine surgery attempts to: decrease iatrogenic muscle injury, decrease pain and speed postoperative course by the use of smaller incisions and specialized instruments.
Causes of surgery and interventional radiology on spine are represented largely by disk herniation (most commonly lumbar), which we will discuss further in this treatment. Stenosis of the vertebral canal, vertebral instability, and vertebral fractures will also be analyzed [1, 2]. The therapeutic treatment of spinal pathology initially includes conservative therapy and in case of failure a number of surgical procedures and/or interventional radiology approaches, with varying degrees of invasiveness, such as discectomy, vertebroplasty, and surgical stabilization. With recent advances of intervention techniques and devices used, minimally invasive approaches are becoming increasingly popular for the treatment of spine disorders. In particular, minimally invasive spine surgery attempts to: decrease iatrogenic muscle injury, decrease pain and speed postoperative course by the use of smaller incisions and specialized instruments.
1.1 Disk Herniation
Herniated disk is one of the most common diseases with very high social costs; it is the first cause for absenteeism from work and the second for permanent disability. 55 % of the population in European countries reports at least once in life a variable episode of low back pain and 80 % a simple low back pain [3]. Who is affected many times, unfortunately, begin a diagnostic and therapeutic route involving orthopedic, neurosurgeon, physiatrist, and neurologist. Its natural history provides for a first time period (of variable length between 3 and 6 weeks) characterized by pain (more or less intense) which is followed by a second phase in which the painful symptomatology is attenuated and then disappears leaving the place to symptoms of neurological deficit (decrease in strength of muscle innervated by the compressed root) [4–7]. Herniated disk, commonly lumbar, is the main cause for surgery on the spine, not always resolutive. In postoperative course may arise in fact a recurrence or a fibrous scar that if hypertrophic can compress and irritate the affected nerve and require a second operation (the rate of re-operation is around 3–15 %).
1.1.1 Lumbar Disk Hernia
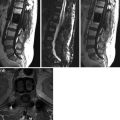
Lumbar disk herniation is a degenerative disease of the intervertebral disk that arises from the rupture of the annulus fibrosus and subsequent leakage of nucleus pulposus in spinal canal with compression on dural sack and nerve root. Especially in people of 30–50 years with low back pain, symptoms originate from radiculopathy due to compression of lumbosacral nerve roots (pain radiating along the course of the sciatic nerve, from gluteal region to the back of the thigh and posterolateral leg up the ankle) or crural suffering (pain along the anterior or anterior-medial thigh, along the course of the crural nerve), causing functional impairment. Radicular pain is caused by mechanical compression, inflammatory effects, vascular and biochemical modifications caused by the contact between the disk and nerve roots.
Diagnosis involves the collection of anamnestic data; physical examination and clinical trials to assess root involvement (irritative, deficit, paretic), diagnostic imaging (X-ray, computed tomography CT, magnetic resonance MRI), and instrumental examination (electromyography).
Treatment may be conservative or can contemplate surgical procedures and/or interventional radiology approach. The choice of treatment depends in general on two elements: the entity or the persistence of acute symptoms and the presence of a functional damage. This latter aspect is sometimes highlighted (in case of serious damage root) by the decreased (or absent) functionality of the muscles innervated by that root. In this case a great help is the electromyographic examination that tells us precisely the functional status of the root compressed by herniated disk. This test, performed by implanting small needles along the lower limb, records the electrical potentials sent along nerve roots to the muscles for their contraction. Compression (and inflammatory state that follows) alters the ability of conducting electrical stimulation along the nerve fibers and thus alters the electrical characteristics of these pulses. Recording these changes allows to obtain a quantitative assessment of root damage and also to determine whether the damage is recent or old.
Conservative therapy for at least 7–10 days, or until the disappearance of intense pain, consists of absolute abstention from even moderate physical actions, from assumption of incorrect positions, or from trunk flexion. Pharmacotherapy, recommended for a short time, involves administration of corticosteroids (betamethasone or methylprednisolone), nonsteroidal anti-inflammatory (NSAIDs), pain relievers (tramadol, paracetamol, paracetamol + codeine, morphine), muscle relaxants, and periradicular infiltration therapy. After the hyperacute phase, physiatric evaluation may be required to start postural exercises and neuromuscular electrical stimulation. In addition to standard medical treatments, several alternative treatments have also been shown to provide effective pain relief for many patients. Most common alternative care actually are chiropractic manipulation, acupuncture, and massage therapy.
Surgical options are: open surgery, microsurgery, and minimally invasive percutaneous surgery. These are used for different types of herniated disks: contained or extruded, with and without dislocated fragment, and with or without narrow canal. Criteria for elective surgical indication is the failure of conservative therapy; the presence of symptoms and signs of sensory or motor involvement in the corresponding dermatomer; electromyography positive for severe root damage and recent documentation of disk herniation on MRI or CT. The cauda equina syndrome from herniated disk is an absolute indication for surgery to be performed urgently.
< div class='tao-gold-member'>
Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree