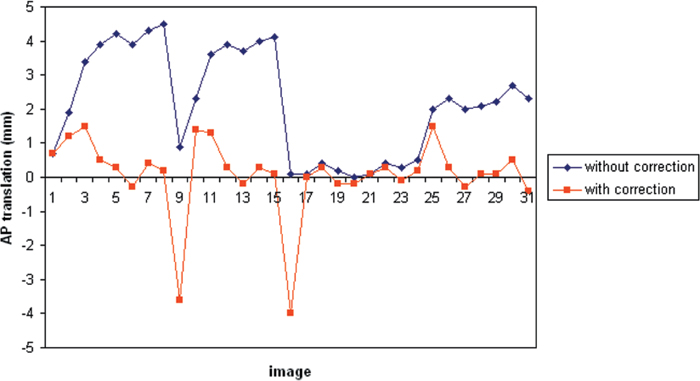
4 Patient immobilization is an important part of the spine radiosurgery procedure and directly influences the accuracy of target localization. Radiosurgical targeting accuracy has traditionally been obtained by rigidly immobilizing the patient in a stereotactic frame that defines a coordinate system for configuring the treatment beams and simultaneously positions the target site at the isocenter of the radiation delivery device. Frame-based treatment in the cranial site can achieve a targeting precision of 1 mm but has three shortcomings: (1) the frame is invasive, (2) fractionation is inhibited, and (3) treatment is restricted to sites amenable to frame fixation. Hamilton et al were the first to use an invasive spine immobilization frame, which rigidly attached to the spinal processes of a patient in the prone position, for spine radiosurgery.1 Target accuracy of 2 mm in the transverse plane and < 4 mm in the longitudinal direction was reported. However, due to its highly invasive nature, the technique was not widely adopted. Noninvasive stereotactic body frames had also been developed.2–4 However, due to the lack of rigid fixation to the vertebral column, the targeting accuracy solely based on the frame was not ideal. Image-guided target localization, in combination with proper patient immobilization, has been developed to overcome these limitations.4–8 The Novalis (BrainLab AG, Feldkirchen, Germany) and the CyberKnife (Accuray Inc., Sunnyvale, California) systems are currently two dedicated commercial radiosurgical units that have been widely used for image-guided spine radiosurgery. This chapter will discuss patient immobilization and potential motion during treatment specifically for these two units. The spine is an example of a site that is difficult to immobilize in a traditional frame and that also benefits from fractionated treatment. It was thus an early candidate for frameless radiosurgery using the CyberKnife.5,6 When the treatment site is not immobilized with a rigid frame, however, patient movement can occur and potentially affect dose alignment. Therefore, it is important to investigate movement during frameless radiosurgery. The CyberKnife is a frameless image-guided stereotactic radiosurgery system that uses x-ray radiographic imaging in the treatment room to locate and track the treatment site while controlling the alignment of radiation beams via a robot-mounted linear accelerator.9 This system is unique in the way it eliminates all three functions of the stereotactic frame: (1) the target reference coordinates provided by the external frame are replaced by reference coordinates in the patient’s anatomy; (2) the radiation delivery system has no isocenter but instead moves the beam to the position of the tumor; and (3) a real-time control loop between the imaging and beam delivery systems allows the beam to adapt to changes in the target position, eliminating the need for rigid fixation. The CyberKnife radiosurgery system is illustrated in Fig. 4.1. The system uses a robotic arm to direct the x-ray beam generated by an X-band 6 MV linear accelerator (linac). A pair of orthogonally positioned amorphous silicon diagnostic x-ray cameras is used to image the patient during treatment. The acquired radiographs are automatically registered to digitally reconstructed radiographs (DRRs) derived from the treatment planning computed tomography (CT) study to determine the patient’s position. A control loop between the imaging system and the robotic arm allows the pointing of the treatment beam to be adapted automatically to the observed position of the treatment site. This allows the system to monitor and adjust to patient movement during treatment. The CyberKnife maintains a quasi-continuous record of target position throughout each fraction, thus providing the data needed to assess patient motion during frameless spine radiosurgery. Because the CyberKnife can adapt to intrafraction movement during spine radiosurgery, it is possible to use comparatively nonrestrictive positioning restraints. It is important to recognize that the nature of the patient restraint will influence the residual intrafraction motion. CyberKnife treatments to the cervical spine rely on restraint of the head in an Aquaplast mask (Aquaplast Corp., Wyckoff, New Jersey; Fig. 4.2), whereas treatments to the thoracic and lumber spine are done while the patient lies supine in a conformable alpha cradle. The face mask constrains motion (but does not rigidly immobilize) in all directions, whereas the alpha cradle supports and stabilizes the patient without constriction. The movement data discussed here were observed for these two restraint methods. Figure 4.1 The CyberKnife Radiosurgery System. (From Accuray Inc., with permission.) Treatment sites along the cervical spine were located with reference to the nearest vertebral body. The image guidance system acquired orthogonal views of the neck at oblique angles and determined the position of the vertebral landmark by highlighting bony edges and registering them to the corresponding bony structures in the treatment planning CT study. Figure 4.3 illustrates a cervical spine DRR used for the position determination. Lesions along the thoracic and lumbar spine were also located with reference to the nearby spine, but in these cases the bony structures themselves were difficult to detect in the images, so stainless steel fiducials were implanted percutaneously in the bone for use as targeting landmarks. Intrafraction movement can consist of moment-by-moment random fluctuations, periodic respiratory movement, and systematic slow drifting in the mean position. The random, periodic, and systematic components will have different effects on the dose distribution. Figure 4.2 Using an Aquaplast mask to limit cervical spine movement. Figure 4.3 One of two orthogonal radiographs used to measure and monitor cervical spine position during a CyberKnife treatment. Image-guided frameless spine radiosurgery begins with orthogonal setup images to establish the initial target position. It then may or may not involve periodic corrections for movement during the fraction. If targeting is based solely on the initial setup position, the delivered dose distribution will be perturbed by the cumulative random and systematic shifts throughout the fraction. If intrafraction realignment is done, the systematic offset will be removed, and the dose distribution will be perturbed only by the net random fluctuations that occur between position corrections. These two scenarios have different dosimetric consequences. For spine radiosurgery with the CyberKnife, the target position is observed episodically rather than continuously during treatment. The imaging frequency for each patient is based on a combination of past experience and an assessment of the patient’s own particular movement patterns observed during setup and treatment. Typically, the imaging frequency is set at ~1 to 2 frames per minute. If at any time during treatment the patient appears to be moving more frequently than anticipated in the imaging duty cycle, the system can be reprogrammed to increase the frequency of position measurements. Intrafraction target position and movement data have been collected and analyzed for 17 cervical and 19 thoracic/lumbar sites treated with the CyberKnife.10,11 The movement data were analyzed in two ways: (1) as net translational offsets from the initial setup position and (2) as fluctuations in position from 1 minute to the next. The net translation from setup is the targeting error that perturbs the dose when periodic realignments are not employed during the fraction, and the periodic fluctuations represent the targeting perturbation when realignment is employed (because each new image acquisition effectively represents a new reference setup position). Figure 4.4 is an example of the anteroposterior (AP) position record for one patient, showing the combined random and systematic movement relative to the initial setup position (in blue) and relative to the most recent previous intrafraction measurement of position (in red). This patient showed a mean systematic drift of 2.2 mm in the AP direction. Figure 4.4 An example record of thoracic spine position in the anteroposterior direction at 1-minute intervals during delivery of a CyberKnife treatment. The blue curve measures absolute position relative to the starting setup; the red curve measures the change in position from 1 minute to the next. When all of the patient position records for spine treatment were analyzed, there was no evidence of respiratory movement of the spine itself at a level of 1 mm for patients treated in the supine position.10 No data were obtained for treatments in the prone position.
Patient Immobilization and Movement
 CyberKnife
CyberKnife



![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


