10 Pediatric Radiology
Special Consideration of the Growing Skeleton and Normal Variants
Epiphyseal Ossification of the Proximal Humerus
Ossification Pattern
 Newborns: Ossification center rarely present, occasionally a faint calcific rim
Newborns: Ossification center rarely present, occasionally a faint calcific rim
 Fourth to eighth month: Medial ossification center along the fossa
Fourth to eighth month: Medial ossification center along the fossa
 First to second year: Lateral ossification center in the major tuberosity
First to second year: Lateral ossification center in the major tuberosity
 Third to fourth year: Ossification center in the minor tuberosity
Third to fourth year: Ossification center in the minor tuberosity
 Fifth to eighth year: Fusion of the tubercular ossification centers
Fifth to eighth year: Fusion of the tubercular ossification centers
 Thirteen to fourteenth year: Fusion of the tubercular ossification centers with the proximal humeral epiphysis
Thirteen to fourteenth year: Fusion of the tubercular ossification centers with the proximal humeral epiphysis
 Twentieth year: Osseous connection of the humeral epiphysis with the humeral diaphysis (Fig. 10.1).
Twentieth year: Osseous connection of the humeral epiphysis with the humeral diaphysis (Fig. 10.1).
Specific Findings
 Epiphyseal plate resembles a pitched roof; differential diagnosis (DD): epiphyseal fracture (rare)
Epiphyseal plate resembles a pitched roof; differential diagnosis (DD): epiphyseal fracture (rare)
 Crescentic vacuum phenomenon with the arms elevated and pulled: “True” joint space between glenoid and cartilage of the humeral epiphysis
Crescentic vacuum phenomenon with the arms elevated and pulled: “True” joint space between glenoid and cartilage of the humeral epiphysis
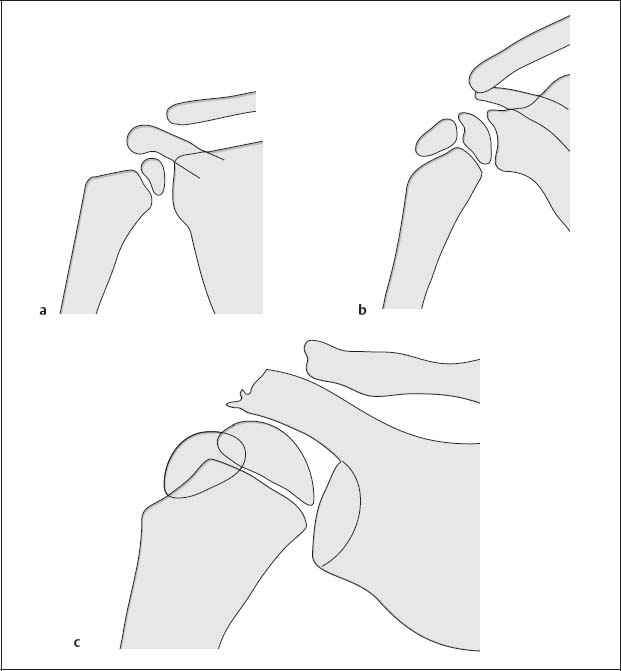
Fig. 10.1  Diagram of the epiphyseal ossifications at the proximal humerus
Diagram of the epiphyseal ossifications at the proximal humerus
a Fourth to eighth month
b First to second year
c Fifth to eighth year
Apophyseal Ossification of the Shoulder
Ossification Pattern
 First year: Apophyseal ossification center in the coracoid process:
First year: Apophyseal ossification center in the coracoid process:
– Isolated until the 15th-16th year
– Occasional ossification center at the tip of the coracoid (Fig. 10.2)
 Fifteenth to eighteenth year: Two to three or even more ossification centers in the lateral end of the acromion
Fifteenth to eighteenth year: Two to three or even more ossification centers in the lateral end of the acromion
 Around the twentieth year: Fusion of the apophyseal ossification centers with the scapular spine
Around the twentieth year: Fusion of the apophyseal ossification centers with the scapular spine
 Sixteenth to eighteenth year: Apophyseal ossification centers at the superior and inferior angle of the scapula
Sixteenth to eighteenth year: Apophyseal ossification centers at the superior and inferior angle of the scapula
Specific Findings
 Double contour of the intertubercular groove; DD: Neonatal periosteal reaction, nonossifying osseous fibroma (NOF; Fig. 10.3).
Double contour of the intertubercular groove; DD: Neonatal periosteal reaction, nonossifying osseous fibroma (NOF; Fig. 10.3).

Fig. 10.2  Apophyseal ossification center in the coracoid process (arrow)
Apophyseal ossification center in the coracoid process (arrow)
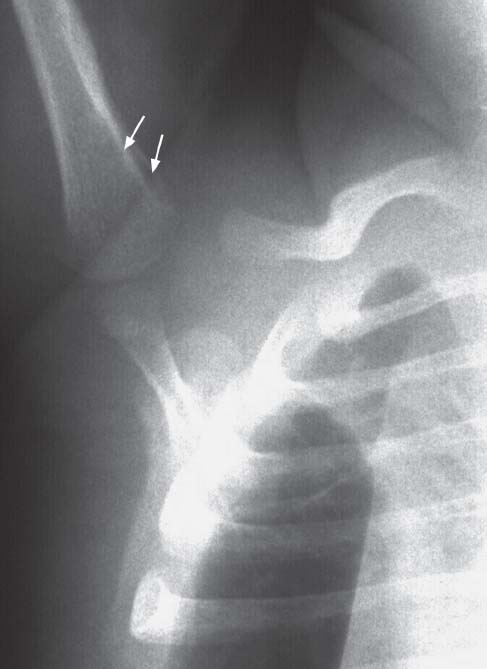
Fig. 10.3  Neonatal humerus
Neonatal humerus
Double contour of the intertubercular groove at the proximal humerus in the newborn (arrows).
Configuration of the Medial Clavicular End
 First decade of life: Mushroom-like, smooth, or torn contours
First decade of life: Mushroom-like, smooth, or torn contours
 Second decade of life: Cup-like, possibly irregularly outlined
Second decade of life: Cup-like, possibly irregularly outlined
 Thirteenth to fourteenth year: Appearance of the medial epiphysis
Thirteenth to fourteenth year: Appearance of the medial epiphysis
 At the end of the second decade of life: Fusion of the ossification center with the clavicle
At the end of the second decade of life: Fusion of the ossification center with the clavicle
 “Ligament grooves” at the medial end of the clavicle caused by impression of the costoclavicular ligament (Fig. 10.4)
“Ligament grooves” at the medial end of the clavicle caused by impression of the costoclavicular ligament (Fig. 10.4)
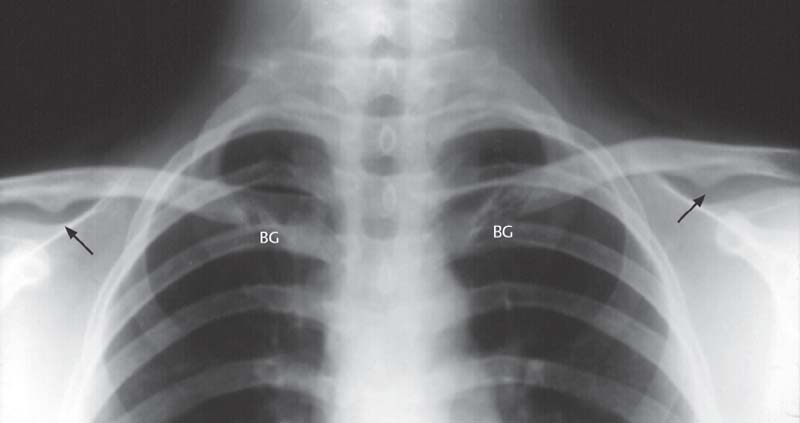
Fig. 10.4  “Ligamentous groove” (BG) at the medial end of both clavicles
“Ligamentous groove” (BG) at the medial end of both clavicles
Impression of the costoclavicular ligament as a linear radiolucency extending craniolaterally to caudalmedially. Incidental finding of a joint (arrows) forming between clavicle and coracoid process (clinically irrelevant anomaly).
Diagnostic Guidelines for Variations of the Growing Skeleton
1 CR (method of choice)
 AP projection (comparison with contralateral side)
AP projection (comparison with contralateral side)
2 US (supplementary method)
 Occasionally the only suitable method, for example, for evaluation of the humeral epiphysis
Occasionally the only suitable method, for example, for evaluation of the humeral epiphysis
Therapeutic Principles
Conservative
 For minor findings, physical therapy
For minor findings, physical therapy
Surgical
 Distal displacement of the scapula (Green, Woodward) in the third to seventh year
Distal displacement of the scapula (Green, Woodward) in the third to seventh year
Malformations
Congenital High Position of the Shoulder (Sprengel Deformity)
Pathology
 Fifth week: Primordial scapula in the lower cervical region
Fifth week: Primordial scapula in the lower cervical region
 Tenth week: Descent of the scapula to posterior chest wall
Tenth week: Descent of the scapula to posterior chest wall
 If interrupted, “congenital undescended scapula”
If interrupted, “congenital undescended scapula”
 Usually unilateral
Usually unilateral
 Scapula wide and shortened
Scapula wide and shortened
 Omovertebral bone: Fibrous, cartilaginous, or osseous connection between cervical spine and scapula
Omovertebral bone: Fibrous, cartilaginous, or osseous connection between cervical spine and scapula
 Hook-shaped curvature of the mediosuperior angle
Hook-shaped curvature of the mediosuperior angle
 Combination with muscle anomaly
Combination with muscle anomaly
 In about 70% of cases, associated anomaly of the vertebrae and ribs (Klippel-Feil syndrome); spinal canal pathologies: diastematomyelia, syringomyelia
In about 70% of cases, associated anomaly of the vertebrae and ribs (Klippel-Feil syndrome); spinal canal pathologies: diastematomyelia, syringomyelia
Clinical Findings
 Asymmetry of the shoulder contour
Asymmetry of the shoulder contour
 Restricted mobility (abduction)
Restricted mobility (abduction)
Diagnostic Evaluation
 (→ Method of choice)
(→ Method of choice)
Recommended views
 Standard projections:
Standard projections:
– Anteroposterior (AP) projection of the shoulder joint
 Special projection:
Special projection:
– Oblique projection: omovertebral bone
 (→ Supplementary method)
(→ Supplementary method)
Indications
 Associated malformations of the spine and bony thorax
Associated malformations of the spine and bony thorax
Therapeutic Principles
Surgical
Indications:
 Pain
Pain
 Functional impairment
Functional impairment
 Cosmetic disfiguration
Cosmetic disfiguration
Congenital Clavicular Pseudarthrosis
Pathology
 Failed fusion of the clavicular ossification centers
Failed fusion of the clavicular ossification centers
 Intrauterine fracture
Intrauterine fracture
 Erosion: Pressure by the subclavian artery
Erosion: Pressure by the subclavian artery
Clinical Findings
 Congenital
Congenital
 Often only discovered in the fourth to sixth year
Often only discovered in the fourth to sixth year
 Usually unilateral
Usually unilateral
 Predominantly on the right
Predominantly on the right
 Medial fragment elevated
Medial fragment elevated
 Lateral fragment pulled down by the weight of the arm
Lateral fragment pulled down by the weight of the arm
 Cosmetic disfiguration
Cosmetic disfiguration
 Shoulder function usually not impaired
Shoulder function usually not impaired
 Rarely painful
Rarely painful
Diagnostic Evaluation

Recommended views
 AP projection of the shoulder
AP projection of the shoulder
Findings
 Interrupted contour of the clavicular shaft
Interrupted contour of the clavicular shaft
 Clubbing of the ends of the fragments
Clubbing of the ends of the fragments
 Fibrous connection (Fig. 10.5)
Fibrous connection (Fig. 10.5)
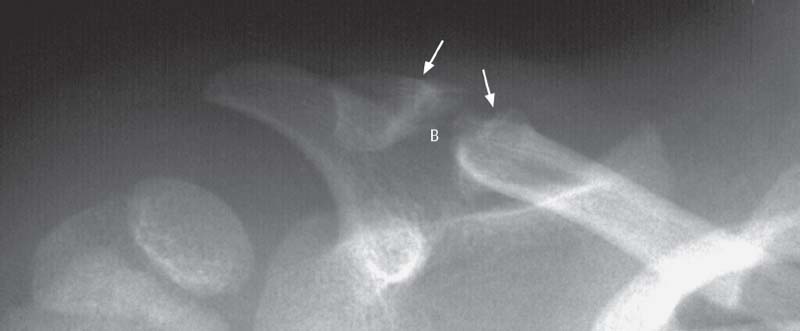
Fig. 10.5  Congenital clavicular pseudarthrosis
Congenital clavicular pseudarthrosis
Break in the lateral third of the clavicular shaft with terminal clubbing of the clavicle (arrows), with interposed fibrous bridging (B).
Shoulder Deformities in Osteochondrodysplasias
Cleidocranial Dysplasia
Pathology
 Generalized skeletal disease
Generalized skeletal disease
 Defect formation
Defect formation
 Impaired ossification
Impaired ossification
 Autosomal dominant inheritance
Autosomal dominant inheritance
 Numerous phenotypic variations
Numerous phenotypic variations
Clinical Findings
 Skull, thorax, and pelvis primarily involved
Skull, thorax, and pelvis primarily involved
 Bell-shaped thorax
Bell-shaped thorax
 Drooping shoulders
Drooping shoulders
 No palpable or visible normal clavicle
No palpable or visible normal clavicle
 Hypermotility of the shoulder girdle
Hypermotility of the shoulder girdle
 Shoulders can touch each other anteriorly
Shoulders can touch each other anteriorly
 Associated pectus excavatum
Associated pectus excavatum
 Diastatic sagittal suture
Diastatic sagittal suture
 Major and minor fontanelle wide open
Major and minor fontanelle wide open
 Short terminal phalanges
Short terminal phalanges
 Brachymesophalangy
Brachymesophalangy
 Impaired dentition
Impaired dentition
 Foot deformities
Foot deformities
 Abnormal gait
Abnormal gait
 Lower limit of body height
Lower limit of body height
 Normal life expectancy
Normal life expectancy
 Habitual dislocation of shoulder, hip, and radial head
Habitual dislocation of shoulder, hip, and radial head
 Vertebral deformities
Vertebral deformities
 Possibly maternal dystocia
Possibly maternal dystocia
Diagnostic Evaluation

Recommended views
 AP shoulder girdle
AP shoulder girdle
 AP pelvis
AP pelvis
 Skull in two projections
Skull in two projections
 AP hand and foot
AP hand and foot
 Lateral spine
Lateral spine
Findings
 AP shoulder girdle:
AP shoulder girdle:
– Complete or partial absence of the clavicle
– Thin, short, inferiorly deviated ribs
– Small hypoplastic scapulae
– Narrow tubular bones
 AP pelvis:
AP pelvis:
– Delayed ossification
– Hypoplastic iliac wings and pubic bones
– Wide cartilaginous pubic symphysis
– Wide sacroiliac (SI) joint spaces
– Wide acetabular Y-cartilage
– Valgus deformity of the femoral neck
– Narrow tubular bones
 Skull in two projections:
Skull in two projections:
– Delayed ossification of the calvarial ossification centers
– Numerous intercalary bones (“wormian bones”)
 AP hand and foot:
AP hand and foot:
– Pseudoepiphysis
 Lateral spine:
Lateral spine:
– Extended persistence of biconvex vertebral bodies (Figs. 10.6, 10.7)
Goals of Imaging
“Minimal bone program”:
 Lateral skull
Lateral skull
 Lateral spine
Lateral spine
 AP pelvis
AP pelvis
 AP hand
AP hand
 AP knee
AP knee
Possible supplementary views:
 Long tubular bone
Long tubular bone
 Foot
Foot
 Chest
Chest
Therapeutic Principles
 Symptomatic orthopedic and dental therapy
Symptomatic orthopedic and dental therapy
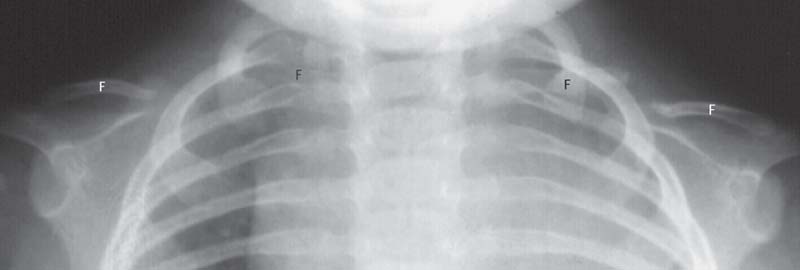
Fig. 10.6  Cleidocranial dysplasia
Cleidocranial dysplasia
Medial and lateral clavicular fragments (F), short, inferiorly deviated anterior ribs, short hypoplastic scapulae.

Fig. 10.7  Cleidocranial dysplasia
Cleidocranial dysplasia
F | Early ossification of the ossification centers of the femoral head |
I | Narrow hypoplastic ilium (I), wide sacroiliac joint space (IF), and Y-cartilage (Y) |
OP | Pubic bone that is not yet ossified |
SH | Varus position of the femoral neck |
Therapeutic Principles
 No causative therapy available
No causative therapy available
 Symptomatic therapy of joint contracture and spinal deformity
Symptomatic therapy of joint contracture and spinal deformity
Mucopolysaccharidoses (MPS) and Mucolipidoses (ML)
Pathology
 Mucopolysaccharidosis (MPS):
Mucopolysaccharidosis (MPS):
– Autosomal recessive
– Exception: Hurler II diseases (X-chromosomal recessive)
– Inherited lysosomal enzyme defect
– Disturbed breakdown of mucopoly-saccharides
 Mucolipidosis (ML):
Mucolipidosis (ML):
– Lysosomal storage disease
– Clinically and biochemically similar to MPS and sphingolipidosis
– Storage of mucopolysaccharides and lipids in bones, central nervous system (CNS), liver, and heart
Clinical Findings
 Strikingly coarse facial features
Strikingly coarse facial features
 Short stature
Short stature
 Mental retardation
Mental retardation
 Facultative: opacified cornea, deafness
Facultative: opacified cornea, deafness
Diagnostic Evaluation

Recommended views
 Lateral skull
Lateral skull
 Lateral spine
Lateral spine
 AP pelvis
AP pelvis
 AP hand
AP hand
 AP knee
AP knee
Findings
 Thickened, stubby scapulae
Thickened, stubby scapulae
 Shallow glenoid fossae
Shallow glenoid fossae
 Short and thickened clavicles and ribs
Short and thickened clavicles and ribs
 Constriction of the proximal humeri (Fig. 10.8)
Constriction of the proximal humeri (Fig. 10.8)
 (→ Supplementary method)
(→ Supplementary method)
Indications
 Storage processes in parenchymal organs
Storage processes in parenchymal organs
Findings
 Heart: thickened myocardium
Heart: thickened myocardium
 Liver: diffuse increase in echogenicity
Liver: diffuse increase in echogenicity
 CNS (in newborns): white-matter lesions
CNS (in newborns): white-matter lesions
 (→ Supplementary method)
(→ Supplementary method)
Indications
 Storage processes in parenchymal organs
Storage processes in parenchymal organs
Technical parameters
 T2-weighted spin-echo (SE)/fluid-attenuated inversion recovery (FLAIR) sequences:
T2-weighted spin-echo (SE)/fluid-attenuated inversion recovery (FLAIR) sequences:
 Axial and coronal sections
Axial and coronal sections
Findings
 Heart: thickened myocardium; diffuse signal alteration
Heart: thickened myocardium; diffuse signal alteration
 Liver: diffuse signal alteration
Liver: diffuse signal alteration
 CNS: white-matter lesions
CNS: white-matter lesions
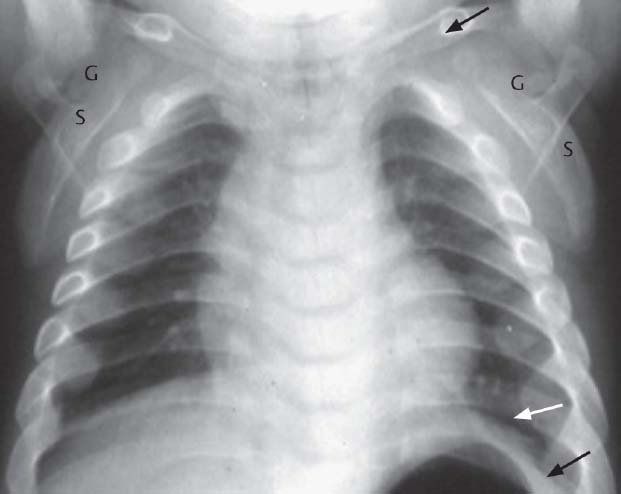
Fig. 10.8  Mucolipidosis II (type “l-cell disease”)
Mucolipidosis II (type “l-cell disease”)
S | Stubby scapula |
G | Shallow, hypoplastic glenoid fossa |
Black arrow | Thickened clavicle |
White and black arrows | Wide ribs with posterior tapering |

Fig. 10.9  Fibrous dysplasia
Fibrous dysplasia
Monomelic unilateral manifestation of the humerus. Cystic osteolytic lesions, thinning and bulging of the cortex (C), remaining in part only as osseous bridge.
O | Osteolyses |
Fibrous Dysplasia
Pathology
 Bone replaced with fibrous connective tissue
Bone replaced with fibrous connective tissue
 “Tumor-like lesion”
“Tumor-like lesion”
 Associated with precocious puberty and cutaneous pigmentation: McCune-Albright disease
Associated with precocious puberty and cutaneous pigmentation: McCune-Albright disease
Clinical Findings
 Preferred age: 5–15 years
Preferred age: 5–15 years
 Solitary lesions:
Solitary lesions:
– Maxilla, femur, tibia
– Can remain subclinical
 Multiple lesions:
Multiple lesions:
– Monomelic, unilateral, generalized
– Initially painful
– Later, spontaneous fractures
Diagnostic Evaluation

Findings
 Bone expansion with loss of normal modelling
Bone expansion with loss of normal modelling
 Cystic osteolytic patches
Cystic osteolytic patches
 Cortical erosions
Cortical erosions
 Scanty spongiosa: hourglass phenomenon
Scanty spongiosa: hourglass phenomenon
 Later, shepherd crook deformity of the proximal femur
Later, shepherd crook deformity of the proximal femur
 After cessation of growth, decreasing activity and increasing stability (Fig. 10.9)
After cessation of growth, decreasing activity and increasing stability (Fig. 10.9)
 (→ Supplementary method)
(→ Supplementary method)
Indications
 To address the question of possible malignant transformation
To address the question of possible malignant transformation
 For the differential diagnosis
For the differential diagnosis
Findings
 Hypointensity on T1- and T2 -weighted SE sequences: Fibrous tissue
Hypointensity on T1- and T2 -weighted SE sequences: Fibrous tissue
 Exception: Proliferative, expansile tissue:
Exception: Proliferative, expansile tissue:
– Hypercellular components
– Increased water content
Therapeutic Principles
 Surgical correction if stability at risk
Surgical correction if stability at risk
 In adults, filling with spongiosa
In adults, filling with spongiosa
 In children, frequent resorption of the filling material
In children, frequent resorption of the filling material
Osteogenesis Imperfecta
Pathology
 Impaired periosteal new bone formation
Impaired periosteal new bone formation
 Impaired collagenous production
Impaired collagenous production
 Decreased bone density
Decreased bone density
 Increased bone fragility
Increased bone fragility
Clinical Findings
 Frequent fractures (following inadequate trauma)
Frequent fractures (following inadequate trauma)
 Deformities
Deformities
 Dwarfism
Dwarfism
 Type I:
Type I:
– Blue sclerae
– Autosomal dominant (former type Lobstein)
 Type II:
Type II:
– Congenital form
– New mutation (former type Vrolik)
 Type III:
Type III:
– Progressive deformity: long tubular bones, skull, spine
 Type IV:
Type IV:
– Like type I but without blue sclerae
Diagnostic Evaluation

Findings
 Severe demineralization
Severe demineralization
 Thin cortex
Thin cortex
 Deficient trabeculation of the spongiosa
Deficient trabeculation of the spongiosa
 Slender tubular shafts
Slender tubular shafts
 Coexistent old and recent fractures
Coexistent old and recent fractures
 Deformity caused by healing of malaligned fractures (Fig. 10.10)
Deformity caused by healing of malaligned fractures (Fig. 10.10)

Indications
 Prenatal diagnosis of type II
Prenatal diagnosis of type II
Therapeutic Principles
 General goal: Upright position of the patient
General goal: Upright position of the patient
 Orthosis after age two years
Orthosis after age two years
 Stabilization with intramedullary fixation
Stabilization with intramedullary fixation
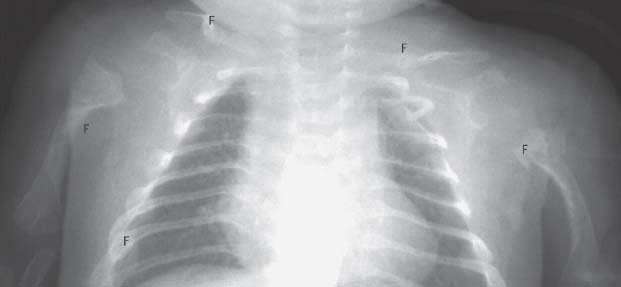
Fig. 10.10  Osteogenesis imperfecta
Osteogenesis imperfecta
Manifestation of osteogenesis imperfecta with extensive osteopenia. Multiple fractures (F) of humeri, ribs, and clavicles, partially healed in malalignment.
Diagnostic Guidelines for Malformations
1 CR (method of choice)
 In general AP projection (contralateral comparison)
In general AP projection (contralateral comparison)
 Specific projections depending on clinical question
Specific projections depending on clinical question
 “Minimal bone program” in osteochondrodysplasias
“Minimal bone program” in osteochondrodysplasias
2 MRI (supplementary method)
 Surrounding soft tissues
Surrounding soft tissues
 Associated malformations: Spine, spinal canal, CNS storage processes
Associated malformations: Spine, spinal canal, CNS storage processes
3 US (supplementary method)
 Storage processes: Heart, liver, CNS (newborns!)
Storage processes: Heart, liver, CNS (newborns!)
 Prenatal diagnosis
Prenatal diagnosis
Therapeutic Principles
Conservative
 Immobilization
Immobilization
 Positioning
Positioning
Surgical
 Internal fixation
Internal fixation
 Possibly rerotation osteotomy
Possibly rerotation osteotomy
Traumatology
Epiphyseal Separation Due to Birth Trauma
Pathology
 Mechanical separation and/or displacement of the cartilage epiphysis
Mechanical separation and/or displacement of the cartilage epiphysis
 Accompanying plexus palsy (Erb-Duchenne) possible
Accompanying plexus palsy (Erb-Duchenne) possible
Clinical Findings
 Painfully restricted mobility
Painfully restricted mobility
 Spontaneous rest position
Spontaneous rest position
Diagnostic Evaluation
 (→ Method of choice in the acute phase)
(→ Method of choice in the acute phase)
Recommended planes
 Coronal sections parallel to the humerus (contralateral comparison!)
Coronal sections parallel to the humerus (contralateral comparison!)
Indications
 Evaluation of epiphyseal displacement
Evaluation of epiphyseal displacement
 Assessment of perfusion with Doppler sonography
Assessment of perfusion with Doppler sonography
 Documentation of ossification centers (Figs. 10.11–10.15)
Documentation of ossification centers (Figs. 10.11–10.15)

Indications
 Selectively during follow-up
Selectively during follow-up

Indications
 Suitable for follow-up
Suitable for follow-up
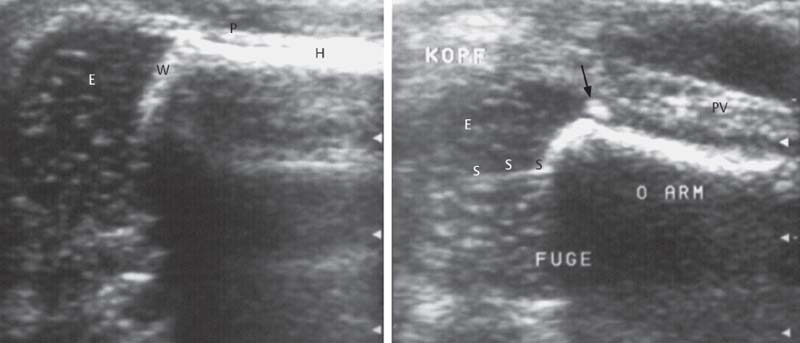
Fig. 10.11  Epiphyseolysis due to birth trauma (Aitken I)
Epiphyseolysis due to birth trauma (Aitken I)
Left image: Longitudinal sonographic section parallel to the proximal humerus, showing a normal finding. The preformed cartilaginous epiphysis is seen along the reflected sound waves, surrounded by the periosteal tube. Interposed growth plate.
Right image: Same section as on the left. Hematoma-induced periosteal thickening of shell-like configuration, small osseous metaphyseal avulsions (arrow), minimally residual epiphyseal displacement after reduction, and internal fixation of the epiphyses. The parallel echogenic structures in the center of the epiphysis correspond to the pin.
E | Epiphysis |
H | Humerus |
W | Growth plate |
E | Epiphysis |
PV | Periosteal thickening |
S | Pin |
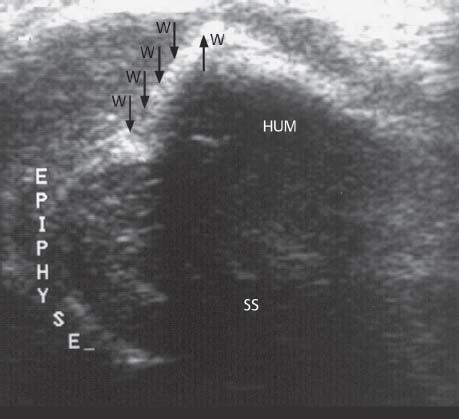
Fig. 10.12  Epiphyseolysis due to birth trauma
Epiphyseolysis due to birth trauma
Longitudinal sonographic section along the proximal humerus. Displaced epiphysis, partially immersed in the acoustic shadow (SS) of the osseous humeral shaft.
W | Growth plate |
SS | Acoustic shadow |

Fig. 10.13  Epiphyseolysis due to birth trauma
Epiphyseolysis due to birth trauma
Radiographic follow-up after reduction and internal fixation: Radiographically invisible epiphysis (!), early, barely discernible callus formation along the lateral border of the metaphysis. In contrast to sonography, the radiograph provides no relevant information for the follow-up at this stage.
E | Epiphysis |
K | Callus |
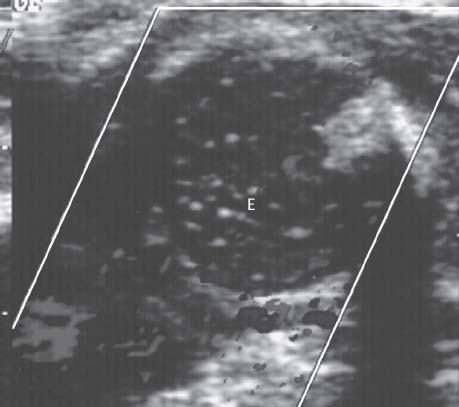
Fig. 10.14  Epiphyseolysis due to birth trauma
Epiphyseolysis due to birth trauma
Doppler sonography to visualize the cartilaginous epiphysis (E) and its perfusion, indicative of viability of the ossification center after reduction and internal fixation.
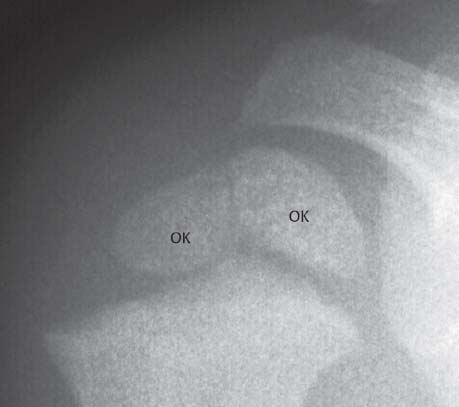
Fig. 10.15  Epiphyseolysis due to birth trauma
Epiphyseolysis due to birth trauma
Radiographic follow-up after one year. Confirmation of the Doppler sonographic finding of Fig. 10.14. Age-dependent development of both ossification centers (OK) in the proximal humeral epiphysis.
Therapeutic Principles
Conservative
 Dressing for pain relief
Dressing for pain relief
 Desault bandage
Desault bandage
 For markedly overlapping fractures, knapsack dressing
For markedly overlapping fractures, knapsack dressing
Surgical
 For severely dislocated proximal fractures in older children, open reduction and internal fixation
For severely dislocated proximal fractures in older children, open reduction and internal fixation
Clavicular Fractures
Pathology
 Fracture usually occurs in the midshaft
Fracture usually occurs in the midshaft
 Greenstick fractures comprise 50%
Greenstick fractures comprise 50%
 Medial fractures (3%):
Medial fractures (3%):
– Usually with epiphyseolysis
– Growth disturbance due to premature closure of the growth plate
– No functional deficits!
 Lateral fractures (5%):
Lateral fractures (5%):
– Usually pseudodislocations
– Central fragment dislocated outside the periosteal tube
– Intact ligamentous connection between acromion, coracoid, and clavicle (Figs. 10.16–10.19)
Diagnostic Evaluation
 (→ Method of choice)
(→ Method of choice)
Recommended views
 AP projection as baseline documentation
AP projection as baseline documentation
 Generally no follow-up necessary
Generally no follow-up necessary
 (→ Supplementary method)
(→ Supplementary method)
Indications
 Substitute for conventional radiography (CR) in classical fractures
Substitute for conventional radiography (CR) in classical fractures
 No recollection of trauma
No recollection of trauma
 Painful swelling (Fig. 10.20)
Painful swelling (Fig. 10.20)
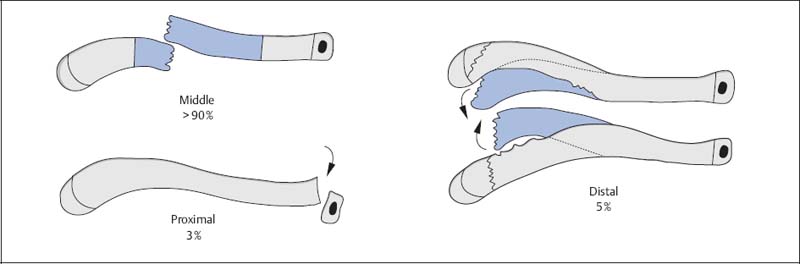
Fig. 10.16  Diagram of clavicular fractures
Diagram of clavicular fractures

Fig. 10.17  Greenstick fracture of the clavicle
Greenstick fracture of the clavicle
Typical manifestation of a greenstick fracture (F) of the clavicle.

Fig. 10.18  Lateral fracture of the clavicle
Lateral fracture of the clavicle
Lateral fracture (F) of the clavicle, also referred to as pseudodislocation. Incidentally visualized is an ossification center in the coracoid (arrow).
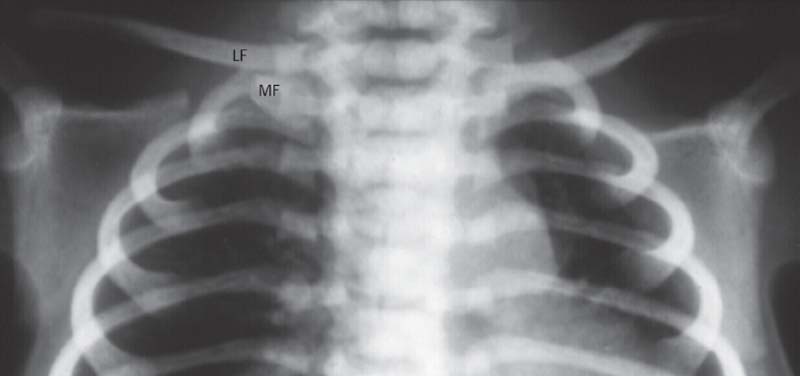
Fig. 10.19  Medial fracture of the clavicle
Medial fracture of the clavicle
Medial fracture of the clavicle with upward displacement of the lateral fragment (LF) by about one shaft width.
MF | Medial fragment |
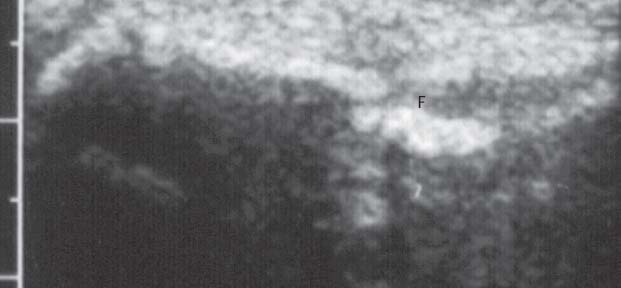
Fig. 10.20  Medial fracture of the clavicle, sonography
Medial fracture of the clavicle, sonography
Interrupted contour in the medial third without displacement.
F |



