Case 2-01. Scaphoid fracture. Fall on an outstretched hand. PA, oblique, and lateral radiographs of the wrist. There is linear lucency (arrow) through the waist of the scaphoid evident on the oblique view, consistent with fracture. The fracture is not visible on the other views.

Scaphoid view of the wrist. There is a transverse fracture (arrow) across the waist of the scaphoid. The scaphoid view is obtained by placing the wrist in ulnar deviation and angling the x-ray beam towards the forearm, in order to project the scaphoid longitudinally onto the x-ray detector. The scaphoid view is the best projection for scaphoid waist fractures [1]. Waist fractures constitute 70% of scaphoid fractures [2]. Fall on an outstretched hand with dorsiflexion is the mechanism of injury. Delayed union, non-union and osteonecrosis of the proximal pole are potential complications and depend on how proximal the fracture site is relative to the entrance of the artery at the waist of the scaphoid which is somewhat variable. For this reason, in general more proximal fractures are likely to develop more complications. To illustrate this, 30% of waist (middle third) fractures develop delayed or nonunion, however proximal pole fractures develop these complications in the majority of cases [3-4]. Non-displaced scaphoid waist fractures can be treated conservatively with good result [5].



Case 2-02. Scaphoid fracture. PA, Oblique, and Lateral views of the wrist. The fracture is difficult to see.

Scaphoid view shows the fracture through the waist of the scaphoid. Fractures of the scaphoid usually occur at the waist and may require ulnar deviation for detection on x-ray. Due to the extensive articular cartilage, vascular supply can be more easily compromised and result in osteonecrosis of the proximal pole. This same principle can be applied to the femoral head and talus. A type of scaphoid malunion is the humpback deformity which occurs when there is increased flexion angulation of the scaphoid; this results in poorer clinical outcomes.
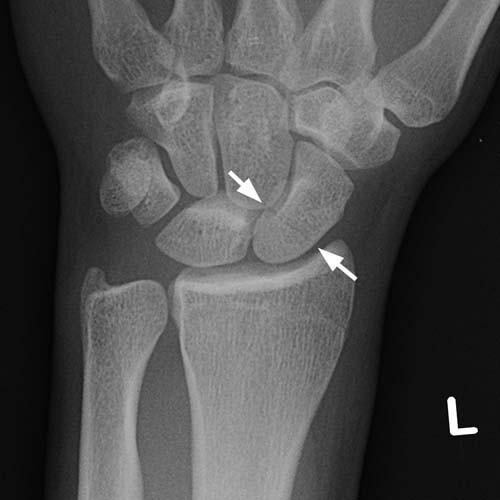


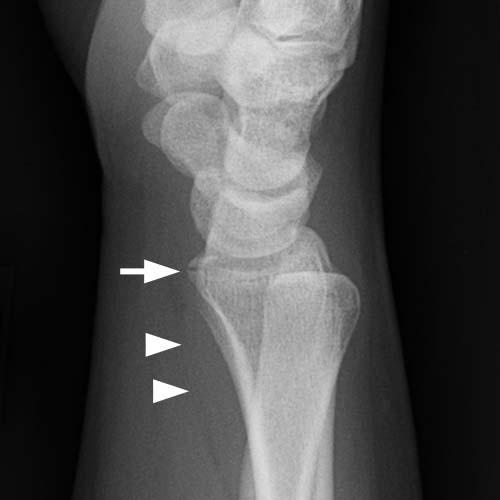
Case 2-03. Scaphoid fracture. PA, lateral and oblique views of the wrist. There is a subtle minimally displaced fracture (arrows) just proximal to the waist of the scaphoid, seen only on the PA projection.

Scaphoid view of the wrist does not show the fracture. Although not helpful in this case, the scaphoid view should be routinely obtained when scaphoid fracture is suspected.


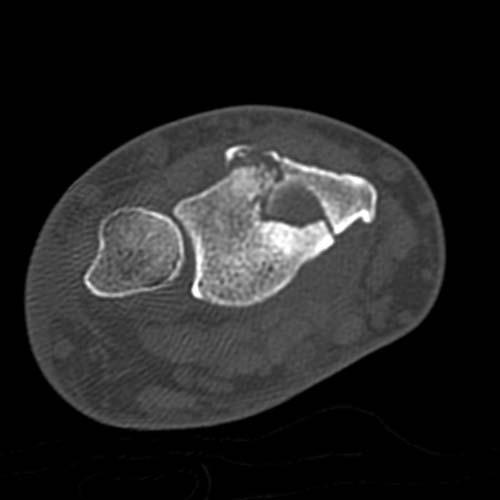
Coronal CT images definitively show the scaphoid fracture traversing the waist. When radiographs are normal or equivocal, and scaphoid fracture is still suspected, CT may be a useful next step. MRI is a reasonable alternative, particularly when soft tissue injuries are also suspected. Fractures of the proximal pole constitute 10% of all scaphoid fractures and have the highest complication rate of non-union and proximal pole AVN. The scaphoid bone is the most commonly fractured of the carpal bones, and constitutes 68.2% of carpal fractures [6].




Case 2-04. Scaphoid fracture in child. PA, oblique, lateral, and scaphoid views of the wrist of a child. There is a non-displaced waist of scaphoid fracture (arrow) seen only on the PA projection. Scaphoid and other carpal bone fractures are infrequent in children, possibly because the bones are incompletely ossified and are cushioned by cartilage. In the immature skeleton, distal radius fractures are the predominant fractures of the wrist [7].

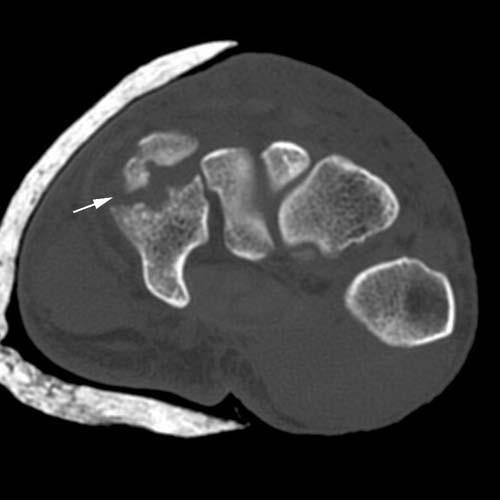
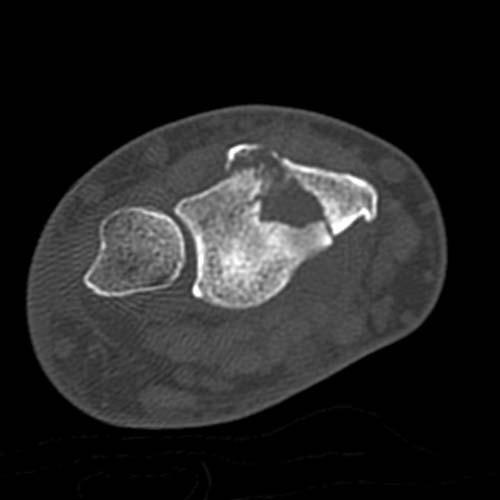
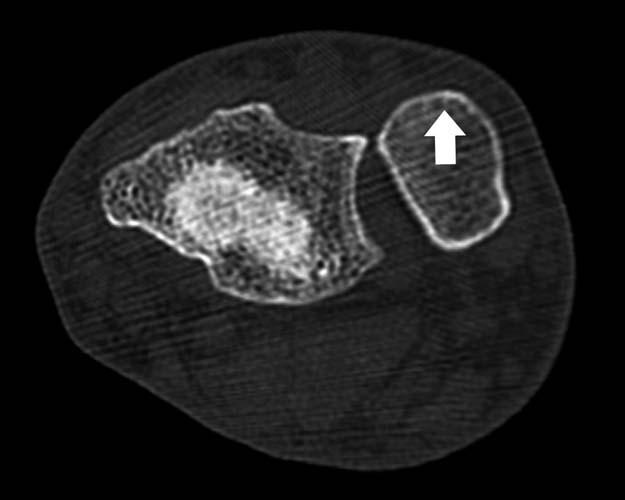
Case 2-05. Hamate fracture-dislocation. Oblique view of the wrist and axial CT scan of the wrist. There is fracture of the hamate with dorsal dislocation of the dorsal fragment. Hamate fractures are subdivided into 2 types, hook (type 1) and body (type 2) fractures. Type 2 can be further subdivided into coronal (2a) and transverse (2b) fractures [8]. This is a type 2a fracture of the hamate. The dorsal fragment has a tendency to dorsally sublux along with the base of the fourth and fifth metacarpals, as seen here.



Case 2-06. Hamate body fracture. PA, oblique and lateral views of the wrist. The joint spaces at the fourth and fifth CMC joints appear narrowed (short arrows). There may be a fracture (long arrow) at the base of the fourth metacarpal base. The overlying soft tissues are swollen (arrowheads). Hamate fractures can be occult in 60% of cases by radiography alone, and may necessitate CT scanning if clinically warranted. Hamate body fractures are commonly associated with fourth and fifth metacarpal base fractures [9].



Sagittal CT images through the hamate. There is a fracture (arrow) at the base of the fourth metacarpal (4). There is dorsal subluxation of the fourth CMC joint (long arrow). There is a fracture through the hamate body in the coronal plane. The hook of the hamate (H) is intact. The base of the fifth metacarpal (5) has displaced into the hamate fracture (*), separating the dorsal and volar fragments.

Case 2-07. Hook of hamate fracture. Carpal tunnel view of the wrist. There is a fracture (arrow) at the base of the hook of the hamate. The carpal tunnel view and axial CT scanning facilitates detection of fractures at the hook of the hamate (H). The trapezium (T), scaphoid (S), and pisiform (P) bones may be identified. The carpal tunnel (arrowheads) is also demonstrated. The carpal tunnel view is obtained by dorsiflexing the wrist and aligning the x-ray beam tangentially along the volar aspect of the wrist.
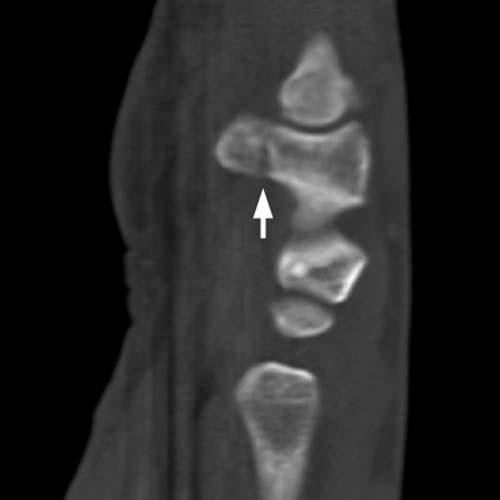

Sagittal CT images of the wrist. The fracture (arrow) at the base of the hook of the hamate is well-demonstrated. The carpal tunnel view and axial CT scanning facilitates detection of fractures at the hook of the hamate [10-11]. Direct force incurred to the hypothenar eminence is a common the mechanism of injury. Such an injury might occur in golfers from the impact of the handle of the golf club, or in baseball players from the impact of the handle of the bat. Hamate fractures in general are uncommon. Symptomatic non-union is a frequent complication of these fractures when treated conservatively. Nonunion can be treated with ORIF or fragment excision [12].



Case 2-08. Trapezium fracture. PA, oblique and lateral views of the wrist. Subtle vertical linear lucency (arrow) through the trapezium is consistent with minimally displaced intra-articular fracture. Trapezium fractures represent only 3-5% of carpal fractures [13]. Typically this involves the radial margin. Dorsal-ulnar tubercle fracture, as seen here, has been described in a series of 4 cases [14].



Case 2-9. Comminuted trapezium fracture. PA, oblique and lateral views of the wrist. The trapezium has compressed between the scaphoid and the first metacarpal base, resulting in multiple fractures (arrows).


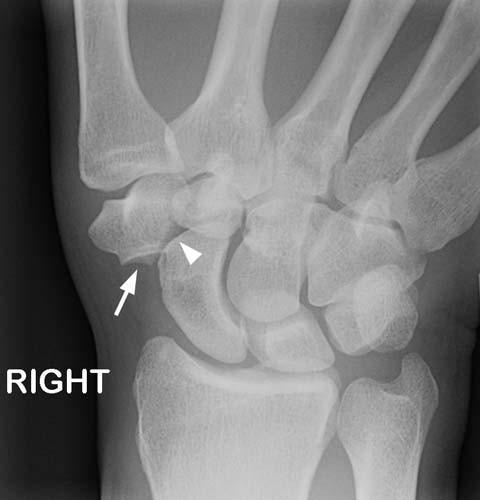
Case 2-10. Trapezium dislocation. Injury sustained in a motor vehicle crash. PA, lateral, and scaphoid radiographs. There is a laterally dislocated trapezium (arrow) relative to the scaphoid. The joint space between the trapezium and trapezoid is abnormally increased, and the lateral portion of the articular surface of the distal scaphoid is bare (arrowhead). These findings are indicative of dislocation of the trapezium from the scaphoid. This is an unusual high energy injury that has the clinical presentation of the much more common scaphoid fracture.
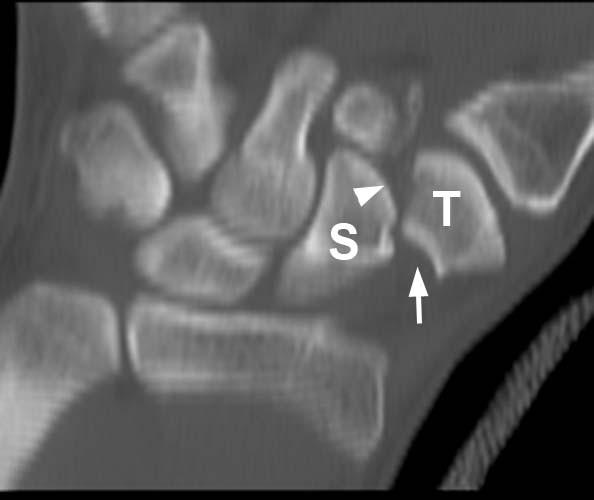
Coronal CT image shows the abnormal relationship between the trapezium (T) and the scaphoid (S). The articular surfaces of the scaphoid (arrowhead) and trapezium (arrow) are dislocated from each other. The thumb has its normal articulation with the trapezium distally, but the trapezoid is separated from the trapezium medially.
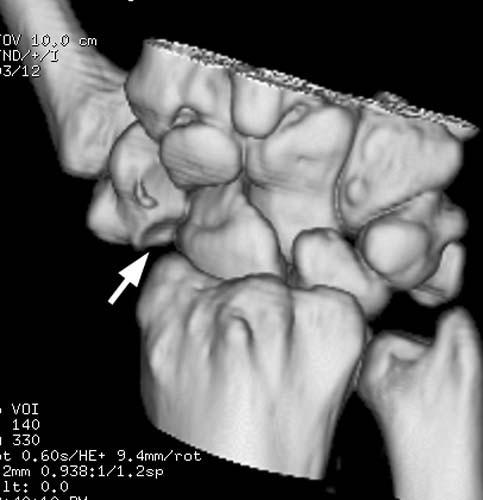
Surface-rendered 3D CT reconstruction shows the bare articular surface of the trapezium (arrow), not articulating with the scaphoid.



Case 2-11. Trapezium fracture-dislocation. PA, oblique and lateral views. There is a laterally dislocated trapezium relative to the scaphoid and fracture fragments consistent with trapezium fracture-dislocation.

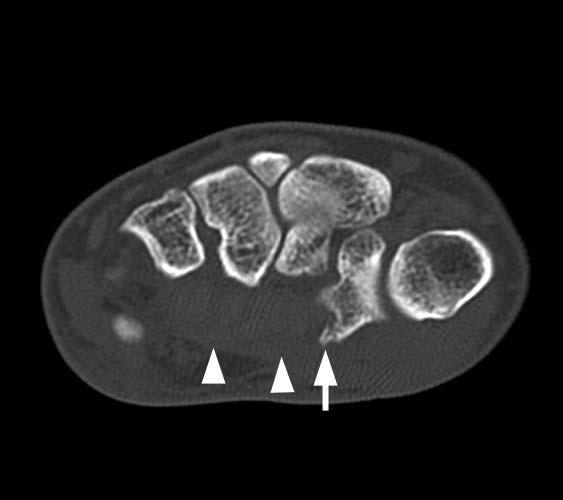
Case 2-12. Trapezium avulsion fracture. Adult injured in a fall on an outstretched hand; the patient’s doctor suspected a scaphoid fracture, but radiographs were normal, and CT was performed. Axial CT image through the tapezium. The first metacarpal is seen as the round structure. There is an avulsion fracture of the volar ridge of the trapezium (arrows), the site of attachment of the transverse carpal ligament (arrowheads). The transverse carpal ligament forms the anterior floor of the carpal tunnel.



Case 2-13. Triquetral fracture. PA, oblique and lateral views of the wrist. There is an avulsion fragment of bone (arrow) at the dorsal aspect of the proximal carpal row seen on the lateral view consistent with triquetral avulsion. This is the second most common carpal fracture, after scaphoid fractures, ranging from 7-20% [15]. Radiotriquetral and ulnotriquetral ligament avulsion produces this injury, typically seen only on the lateral view and can be missed if not sought on the lateral view.




Case 2-14. Pisiform fracture. Construction worker who fell one story off scaffolding, landing on his hands and knees. PA, oblique, lateral, and scaphoid views of the wrist. There is a subtle fracture line through the pisiform bone (arrow), visible only on the lateral view. The wrist is otherwise intact. Isolated fractures of the pisiform bone are rare.


AP and oblique lateral radiographs of the wrist, four weeks later, Bone resorption around the fracture site and displacement of fragments renders the fracture more evident (arrows).


Case 2-15. Gunshot wound. PA and oblique views of the wrist. Numerous metal fragments obscure the bones and carpal bone fractures are difficult to define but are undoubtedly present. Fractures of the fourth and fifth metacarpals are evident. The carpal arcs are not clearly delineated and there is some overlap of the proximal and distal carpal row on the PA projection and some ulnar shift of the proximal carpal row as well, which suggests dislocation. Subtle vertical lucencies are seen in the distal radius on the lateral view, indicating additional fractures. Tissue damage sustained by a projectile is governed by several factors, including the kinetic energy of the projectile, propagation of secondary missiles, and cavitation of tissue. The denser the tissue impacted, the greater the transfer of kinetic energy from the projectile, with greater damage to the tissues. Bone, having a relatively high density for biological tissue, sustains greater damage. Fragmentation of the bullet and of the bones, as seen here, releases secondary missiles, which in turn can increase the volume of damage and in some instances cause worse injuries than the primary missile. Low energy projectiles create cavities only mildly larger than themselves. High energy projectiles have the capacity to create large cavities and tissue damage and can increase in size even after the projectile has exited. One of the complications with gunshot wounds is infection, a complication seen in about 8% of civilian gunshot wounds to the hand [16].



Case 2-16. Gunshot wound. PA, oblique and lateral views of the wrist. There is a bullet lodged in the dorsal soft tissues with associated soft tissue swelling and air. There are fracture fragments dorsally. The distal radial and ulnar physis are not yet fused.


Case 2-17. Rotary subluxation of the scaphoid. PA and lateral views of the wrist. The scaphoid appears almost round on the PA view, and there is an abnormally wide gap between the scaphoid and the lunate. On the lateral view, the angle between the axis of the scaphoid and the axis of the lunate is approximately 90 degrees. These findings indicate that the scaphoid is abnormally rotated along its short axis, assuming a nearly vertical orientation relative to the coronal plane, rather than a 45 degree orientation. This condition is called rotary subluxation of the scaphoid. It is also called scapholunate dissociation, in reference to the cardinal anatomic abnormality, loss of the scapholunate ligament. This lesion falls in the spectrum of carpal instability. The three most common patterns of carpal instability are: scapholunate dissociation, dorsal segmental intercalated instability, and volar intercalated segmental instability, in order of frequency [17-19]. Tear of the scapholunate ligament contributes to scapholunate instability (dissociation). The scaphoid assumes a flexed position and is foreshortened such that a cortical ring outline is seen representing the distal pole. Widening of the scapholunate distance over 4 mm is diagnostic of ligament tear. Increased palmar angulation of the scaphoid leads to widening of the scapholunate angle on the lateral view to over 60 degrees (normal=30-60). The term dissociation applies to misalignment within the same carpal row. Lack of tendinous attachments of the proximal carpal row makes this an intercalated segment, such that alignment is dependent on the radius below it and the distal carpal row above it. Intercalated instability involve misalignments between the carpal rows. DISI occurs when the lunate rotates dorsally and the lunato-capitate angle exceeds 20-30 degrees on the lateral view. Scapholunate dissociation and DISI result from radial-sided ligament injuries. VISI occurs when the lunocapitate angle exceeds 20-30 degrees and the lunate is in volar disposition. This results from ulnar-sided abnormalities, typically lunotriquetral ligament tear/dissociation and also demonstrates a diminished scapholunate angle (less than 30 degrees).


Case 2-18. Transscaphoid perilunate dislocation. PA and lateral views of the wrist. The scaphoid is fractured through its waist. The capitate, with attached neighboring structures, including the hand, distal carpal row, distal pole of the scaphoid, and triquetrum, is dorsally dislocated relative to the lunate. The lunate, with adjacent proximal pole of the scaphoid, is normally located within the distal radial articular surface. This injury is called a transscaphoid perilunate dislocation. If the scaphoid is not fractured, the injury is called a perilunate dislocation, and the scaphoid remains attached to the capitate. An incidental ulnar styloid fracture is present.



Case 2-19. Perilunate dislocation. PA, lateral and oblique views of the wrist. The distal carpal row overlaps the proximal carpal row on the PA view, with disruption of the first and second arcs. The lunate maintains its collinear relationship with the radius, however, the capitate is dorsally dislocated relative to the lunate. The mechanism of injury is fall on an outstretched hand with dorsiflexion. Greater and lesser arcs that course perpendicular to the arcs of Gilula have been devised to explain the patterns of carpal trauma. The lesser arc travels from the distal radius around the perimeter of the lunate and terminating at the distal ulna and essentially delineates the various ligamentous connections of the lunate. The greater arc is wider and passes from the radial styloid through the waist of the scaphoid and proximal capitate and hamate and triquetrum to terminate at the ulnar styloid. Perilunate dislocation is a greater arc injury and most cases demonstrate scaphoid fractures. It is not surprising that these injuries are often seen with scaphoid fractures, since the waist of the scaphoid lies within the arc of injury.


Case 2-20. Perilunate dislocation. PA and lateral views of the wrist. The capitate is proximally displaced and dorsally dislocated relative to the lunate. These are usually accompanied by scaphoid fractures, with only 25% manifesting as isolated dislocations without fracture [20]. Perilunate dislocations outnumber lunate dislocations by 2 or 3:1 [21-22]. There is widening of the distal radioulnar articulation on the PA view and dorsal positioning of the distal ulna on the lateral view, suggesting distal radioulnar dissociation.




Case 2-21. Transscaphoid midcarpal dislocation. PA and lateral and oblique views of the wrist. The articulations between the forearm and wrist and the articulations between the first and second carpal row normally form smooth arcs, the first and second carpal arcs (arcs of Gilula) [23]. These arcs are interrupted, suggestive of ligamentous injury or carpal dislocation. The radius, lunate and capitate do not demonstrate their normal collinear relationship on the lateral view. The lunate is tipped volarly and no longer articulates with the capitate. The capitate is perched over the dorsal radial lip and the lunate is perched over the volar radial lip, with neither complete volar lunate dislocation nor complete dorsal perilunate dislocation. These findings constitute a midcarpal dislocation and is postulated to represent an intermediary point in a continuum of injuries ranging from lunate to perilunate dislocations [23]. The proximal carpal row is secured more adherently to the distal radius by radiocarpal ligaments than is the distal carpal row to its neighbors. Therefore, dislocations tend to occur more frequently between the proximal and distal carpal rows at the midcarpal articulations. A further point of weakness in the midcarpal region is the space of Poirier which lies between the volar radiocapitate and radiotriquetral ligaments, making the lunocapitate articulation a vulnerable area. This case constitutes a midcarpal dislocation. There is a fracture through the waist of the scaphoid and a small fragment of bone is seen at the dorsal lip of the radius. Therefore, this is a transscaphoid midcarpal dislocation with avulsion fracture of the dorsal lip of the radius.


Case 2-22. Midcarpal dissociation (midcarpal dislocation). PA and lateral views of the wrist. There is lunato capitate dissociation with neither completely dislocated from the distal radius, consistent with midcarpal dislocation pattern. A radial styloid fracture is seen.


Case 2-23. Lunate dislocation. PA and lateral views of the wrist. There is an isolated volar lunate dislocation. This represents a high grade lesser arc injury as all the attachments to the lunate are severed. Recall that the lesser arc travels from the distal radius around the radial, distal, and ulnar borders the lunate and terminates at the distal ulna, an is essentially an inner loops that follows the same shape as the greater arc. Stage 1 injury affects the scapholunate ligament, stage 2 affects the lunato capitate joint, stage 3 affects the lunotriquetral articulation (midcarpal dislocations with volar tilt of the lunate), and Stage 4 with no intact ligamentous fixation at all and volar lunate dislocation, as seen here.


Case 2-24. Lateral perilunate dislocation. Fisherman injured while handling crab pots off Alaska. PA and oblique views of the wrist. There is lateral dislocation of the scaphoid and entire distal carpal row relative to the radius and lunate and triquetrum. The lunate and triquetrum maintain articulation with the radius and no longer articulate with the laterally dislocated scaphoid and distal carpal row. There is a displaced fracture fragment from the radial styloid. This is a lateral perilunate dislocation. Dorsal perilunate dislocations are the most common, and volar perilunate dislocations are second. Radial perilunate dislocations are the least common. All three share in common disruption of the lunato-capitate articulation. In lateral perilunate dislocation the capitate is dislocated lateral to the lunate.




Case 2-25. Complex carpal fracture-dislocation. Oblique, lateral and PA view of the wrist. The lunate is volarly dislocated out of the radial fossa. The scaphoid is fractured with the proximal pole dislocated as well.


Case 2-26. Lunate extrusion. Oblique and lateral views of the wrist. The carpus and hand are dorsally displaced relative to the radius and the lunate is not seen. Soft tissue deformity and defect at the volar aspect of the wrist is noted. This is an open lunate dislocation, with complete extrusion of the lunate from the body through the volar soft tissue wound.





Case 2-27. Multiple carpal bone dislocation. Worker whose hand was caught between a wall and a truck slowly backing up. Oblique and lateral views of the wrist. There is radial and volar dislocation of the scaphoid (S). The lunate (L) is perched on the dorsal lip of the radius and dorsally dislocated from the capitate and the capitate is perched on the volar lip of the radius, reminiscent of a midcarpal dislocation. The triquetrum (T) is dislocated volarly. Scaphoid dislocation is rare, however, when they occur tend to be volar as a result of acute ulnar and dorsiflexion while holding steering wheel or handlebars of motorcycle in a high speed crash [24]. Rotation of the scaphoid results in its lateral border facing anteriorly. These injuries are usually treated with closed reduction. A missed case of volar scaphoid treated 2 weeks later with open reduction had a good functional long-term outcome [25].

Case 2-28. Traumatic trans-carpal hand amputation. PA view of the hand and wrist. There is complete carpal amputation with only the radial styloid remaining of the forearm. A piece of the lunate and triquetrum are also missing. Mechanisms for carpal amputation include rotary saw, guillotine-like, and local crush mechanisms, and are seen most often in the setting of industrial trauma [26]. Replantation of the hand may be successfully performed in some cases [27-28]. Therefore, it is important to retrieve the amputated parts.




Case 2-29. Radial styloid fracture. Oblique, lateral and PA views of the wrist. There is a minimally displaced oblique fracture (long arrow) of the radial styloid radius extending to the joint surface at the scapholunate level. The so-called chauffeur fractures may manifest as small avulsion injuries of the radial styloid or oblique fractures of the styloid extending up to the articular surface of near the scapholunate joint. The mechanism of injury is direct impaction of the radial styloid by the scaphoid. These are classically non-displaced as seen here, and best seen on the PA view [29]. Small ulnar styloid avulsion is also seen (short arrow). Ulnar styloid fractures are associated with distal radial fractures and when present, ulnar styloid avulsions bode a worse prognosis due to its impact on distal radioulnar function [30].


Case 2-30. Radial styloid fracture. PA, lateral and oblique views of the wrist. The pronator fat pad is displaced. There is a subtle non-displaced oblique fracture of the radial styloid radius extending to the joint surface at the scapholunate level.



Case 2-31. Radiocarpal fracture-dislocation. PA, obilque and lateral views of the wrist. There is a displaced fracture (arrow) of the radial styloid process. The radiocarpal joint is dislocated, with the carpus and hand dorsally dislocated as a unit from radial articular surface. Radiocarpal dislocations result from high energy trauma and typically include a combination of injuries to the ligaments and bones that hold the wrist to the forearm [31]. In this case, the ligaments on the radial side are intact but attached to the displaced radial styloid fragment, while the other ligaments are torn.

Case 2-32. Comminuted intra-articular distal radius fracture. PA view of the wrist. There is a comminuted fracture of the radial styloid with a vertical component extending into the joint and an ulnar styloid avulsion. Positive ulnar variance and overlap of the distal ulna onto the medial margin of the distal radius suggests distal radioulnar joint disruption.



Case 2-33. Comminuted intra-articular distal radius fracture. PA, lateral and oblique views of the wrist. There is a comminuted fracture of the distal radius with intra-articular component and some dorsal displacement. The distal radial articular surface has assumed a dorsal tilt. Note the blurring of the pronator quadratus fat pad. Colles fractures may have an intra-articular component in 70% of cases. The Frykman classification emphasizes the distinction between intra-articular fracture patterns and extra-articular fractures with and without involvement of the ulnar styloid [32]. The Frykman classification scheme of Colles fractures is as follows: I is extra-articular, II is I plus distal ulnar fracture, III involves the radiocarpal joint, IV is III plus distal ulnar fracture, V involves the distal radioulnar joint, VI is V plus fracture of the distal ulna, VII involve both radiocarpal and radioulnar joints, and VIII is VII plus distal ulnar fracture. The pattern seen here is III.


Case 2-34. Impacted distal radial metaphyseal fracture (Colles fracture). Lateral and PA views of the wrist. There is pronounced demineralization. A fracture of the distal radial metaphysis here shows impaction and dorsal angulation. A relative ulnar plus has been produced. There is intra-articular component to the fracture. The bones are demineralized. This fracture is called a Colles fracture. It has been shown that decreased bone mineral density is a contributor to severity of distal radial fractures [33]. Restoration of alignment and volar inclination of the articular surface and restoration of length are the primary focus of surgical treatment [34].


Case 2-35. Die-punch distal radial fracture. Coronal and sagittal reformation and axial CT images of the wrist. Comminuted fracture of the distal radius demonstrates a discrete depressed segment consistent with die-punch fracture. This pattern occurs when a fracture fragment involving the articular surface is driven into the subchondral bone producing a depressed fracture. This is typically seen at the lunate fossa, when it occurs in the distal radius. A more common location for this fracture pattern is the tibial plateau. Displaced articular fractures more commonly demonstrate osteoarthritis as a sequela. Some authors advocate surgical correction for intra-articular fractures of the radius with as little as 1 mm step-off at the articular surface [35].




Case 2-36. Impacted distal radial metaphyseal fracture (Colles fracture). PA, lateral and oblique views of the wrist. The bones are demineralized. There is a fracture of the distal radial metaphysis with dorsal angulation consistent with a Colles fracture. Note the increased convexity of the pronator fat pad. The common mechanism of injury is falling on an outstretched hand, with volar tension and dorsal impaction. Dorsal impaction fracture and volar transverse fracture and loss of ulnar and volar tilt of the distal radius are typical sequela. Traction forces transmitted through the TFC may result in an ulnar styloid fracture, as seen here. About 70% of Colles fractures have an intra-articular component. With greater degrees of compression, a secondary ulnar positive variance may be created which can induce ulnar impaction syndrome. This is the most commonly encountered fracture in mid to older ages and particularly associated with elderly women, with osteoporosis playing a role [36].




Case 2-37. Intra-articular distal radial fracture. PA, lateral and oblique views of the wrist. There is a comminuted transverse fracture of the distal radius with a vertical component reaching the articular surface and resultant dorsal tilt and angulation. Ulnar styloid avulsion is noted. Fernandez and Jupiter divided distal radial fractures into 5 types. Type I is a metaphyseal fracture from bending of the bone, the mechanism seen in a Colles or reverse Colles fracture. The volar metaphyseal cortex fractures in tension and the dorsal cortex fails in compression. Type II is a shear fracture of the articular surface (Barton fracture). Type III is an intra-articular compression fracture and Type IV is an fracture/avulsion. High energy produces a Type V fracture which is comminuted and may result from several different mechanisms [37].




Case 2-38. Salter I fracture of the distal radius. PA, oblique and lateral views of a youngster’s wrist. There is widening of the distal radial physis laterally consistent with a Salter I injury. The bones tend to be stronger in adolescents compared to young children, therefore while younger ages show radial metaphyseal buckle fractures, adolescents tend to more often show fractures involving the growth plate rather than the bone, with the majority of wrist fractures in adolescents being Salter I (22%) or Salter II (58%) injuries [38]. A chronic stress injury seen in gymnasts can produce a Salter I injury, however is accompanied by irregularity and sclerosis [39].



Case 2-39. Buckle fracture of the distal radius. PA, oblique, and lateral views of a child’s wrist. There is buckling of the cortex (arrows). On the PA and oblique views, this deformity encircles the distal radial metaphysis, constituting a torus fracture. A buckle fracture is an incomplete fracture, while a torus fracture is a complete fracture involving the circumference of the cortex; however, they are frequently used synonymously. Children’s bones are more pliable, and therefore are more prone to incomplete fractures. Buckle fracture, greenstick fracture, and plastic bowing deformity represent incomplete fractures unique to children. Greenstick and plastic deformity occur from bending (angulation) forces. Fracture occurring on the tension (convex) side of the bone and not the compression side (concave) gives rise to the greenstick fracture. The tension side would be expected to fail first, as bone is weaker to tension forces compared to compression forces. The mechanism of injury for buckle and torus fractures is compression from axial loading [40].
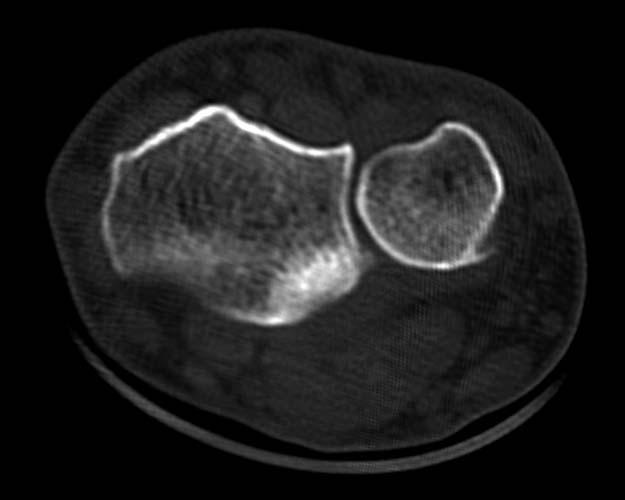
Case 2-40. Distal radioulnar joint subluxation. Axial CT images of the distal radioulnar joint. The second image shows dorsal displacement of the ulna relative to the sigmoid notch of the radius consistent with DRUJ subluxation. Usually associated with distal radial fractures, isolated distal radioulnar joint disruption is rare [41]. The dorsal TFC is the main contributor to stability of this joint. Axial CT scan is diagnostic and supination of the arm will elicit dorsal dislocation, while pronation of the arm will elicit volar dislocation. Distal radioulnar joint incongruity can also be assessed with CT.
Chapter 3. Forearm, Elbow, and Upper Arm
by Catherine Maldjian, M.D., and Felix S. Chew, M.D.



Case 3-01. Galeazzi fracture-dislocation. PA, lateral, and oblique views of the wrist. There is a fracture at the mid to distal thirds of the radial shaft with overriding of the fragments. There is widening of the distal radio-ulnar joint with dorsal displacement of the ulna on the lateral view and a prominent ulnar plus produced by the injury, consistent with distal radio-ulnar dissociation. This is a Galeazzi injury pattern. Isolated radial fracture in this location is accompanied by distal radioulnar dislocation in most instances [1-2] A complication is chronic instability of the distal RU joint. The fracture pattern is also known as a Piedmont fracture, as it was described in the Piedmont Orthopedic Society and published in 1957, eight years prior to Galeazzi’s large series was published [3-4]. It is also known as a reverse Monteggia. Radial fractures that are in closer proximity to the distal radioulnar joint are more often associated with instability of the joint and have been classified into type 1 and type 2 [5]. If the fracture is less than 7.5 cm from the radial articular surface then it is type1 and over 7.5 cm from the distal articular surface is type 2. Treatment usually involves compression plating. The distal radioulnar instability may be occult and close inspection may be required to detect it at the time of surgery.



Case 3-02. Galeazzi fracture-dislocation. PA, lateral, and oblique views of the wrist. There is a fracture of the mid to distal radial shaft with some overriding and with volar angulation. Some overlap of the distal radius and ulna on the frontal projection and dorsal positioning of the distal ulna which overlies the posterior radial cortex on the lateral view imply distal radio-ulnar separation. The fracture pattern that bears Galeazzi’s name was in fact described by Cooper in 1842, nearly a century before Galeazzi’s series of 18 cases was published (1934). It has been described it as the fracture of necessity, since it requires surgical treatment. They comprise up to about 7 % of all adult forearm fractures. The mechanism of injury is axial load from falling on an outstretched and hyperpronated forearm [1].


Case 3-03. Galeazzi fracture-dislocation. PA and lateral views of the forearm. There is a fracture of the mid to distal third of the radius and widening of the distal radioulnar joint and the distal ulna is very distal to the radius, consistent, with a Galeazzi fracture pattern.



Case 3-04. Galeazzi fracture-dislocation. PA views of the wrist and forearm and lateral view of the forearm. Fracture of the distal radius with volar and radial angulation and widening of the distal radio-ulnar joint is consistent with Galeazzi fracture pattern.

Case 3-05. Plastic bowing deformity. Oblique view of the forearm. Plastic bowing of the ulna and complete fracture of the mid radius is seen. Bending of the bone with low force is reversible and constitutes elastic deformity. More intense force gives rise to fractures. Forces that exceed those in reversible bending, but fall short of that required to produce a fracture can cause bowing deformity in children, due to the increased pliability of their bones. In older children, where much further growth is not anticipated, the deformity will not correct itself and reduction is necessary. Bowing deformity may only be manifest in one of the two standard projections and therefore can be overlooked.

Case 3-06. Greenstick fractures. PA view of a child’s forearm. There is an incomplete fracture with cortical break on the tension side and plastic deformity on the compression side in the mid to distal radius and ulna with ulnar angulation, consistent with greenstick fractures. Greenstick and bowing fractures are unique to children, due to the greater pliability of their bones. When only a single forearm bone is involved, the proximal and distal radioulnar joints are more prone to injury. Isolated ulnar greenstick fracture may represent a Monteggia fracture equivalent where there has been spontaneous radial head reduction.


Case 3-07. Nightstick fracture. PA and lateral views of the distal forearm. There is an isolated transverse fracture of the distal ulnar shaft, or nightstick fracture. The mechanism of injury is a direct blow from a stick or club, usually with the forearm raised in a protective attempt. Nightstick fractures are less often seen in the mid and proximal ulna and they are transverse or slightly oblique. Comminution, angulation exceeding 10 degrees, or displacement exceeding 50% are criteria for treatment by open reduction and internal fixation.



Case 3-08. Both bones forearm fractures. PA, lateral, and oblique views of the distal forearm. Fractures of the ulnar and radial shaft are seen with both bones fractured. The majority of forearm fractures involve both bones. Most of these (60%) occur in the middle third, excluding the end fifths of the bones. In children 75% of this fracture pattern is seen in the distal shaft [6-7] and in 85% the radial fracture is more distal than the ulnar fracture [8]. Separation of the forearm bones and proper alignment is important to preserve supination and pronation. The proximal radial fragment is being pulled into supination in this case, indicating that the fracture occurred proximal to the pronator teres insertion. The radial tuberosity lies medially, as seen here, with proximal supination [9].


Case 3-09. Both bones forearm fractures. PA and lateral views of the forearm. Both radius and ulna are fractured, producing butterfly fragments. The mechanism of injury is bending with the compression side failing due to shear stress before the fracture from tension force is completed, resulting in comminuted fracture on the compression side. Fractures of the forearm with butterfly fragments are more difficult to treat and may contribute to a poorer result. [10] In addition, fractures of the forearm that occur at the same level in general have a higher incidence of synostosis. Delayed and non-union are seen more often with premature mobilization prior to rigid fixation and with excessive periosteal stripping either at surgery from open reduction and internal fixation or at the time of injury such as a compound injury with contamination. Operative fixation is the usual treatment for both bone forearm fractures, unless completely non-displaced, and is performed in 48 hours with periosteal stripping only to the degree necessary to achieve good reduction and insert plate.


Case 3-10. Segmental bone bones forearm fractures. PA and lateral views of the forearm. Multilevel transverse fractures of both bones is consistent with segmental fractures. These fractures are fixed with 2 plates at 90 degrees or one long plate, with the goal of restoring normal alignment.


Case 3-11. Gunshot wound. AP and lateral views of the forearm. There are metal bullet fragments adjacent to a comminuted fracture of the mid shaft of the ulna consistent with a gunshot wound. The defect from these injuries may require bone grafting and more extensive surgery.


Case 3-12. Gunshot wound. PA and lateral views of the forearm. Very comminuted fracture of the mid-shaft of the radius is seen from a gunshot wound.



Case 3-13. Forearm amputation. PA and lateral views of the forearm and PA view of amputated hand and wrist. There are transverse fractures of the distal forearm with complete amputation at this level.


Case 3-14. Monteggia fracture-dislocation. PA and lateral views of the forearm. There is a fracture of the proximal third of the ulna and volar radial head dislocation. This fracture pattern was described in 1814 by Monteggia. Eventually, fractures of the ulnar shaft with any radial head dislocation became known by this name [11]. About 90% of the ulnar fractures are proximal, with 10 % mid and 1% distal in location [12]. A classification system is derived based on the dislocation pattern associated with the ulnar fracture. Type I is the most common and was the pattern described by Monteggia, as seen in this case. It involves an ulnar fracture with anterior angulation and radial head dislocation and constitutes 65% of these injuries [13] Type II demonstrates posterior or posterolateral dislocation and posterior fracture angulation and is next most common at 18%. Type III shows lateral or anterolateral dislocation with fracture just beyond the coronoid process and is seen in children. Type IV is anterior dislocation and proximal radial fracture in addition to ulnar shaft fracture. In addition to ulnar fracture and radial head dislocation, common to all of these variants is disruption of the proximal radioulnar joint and ligaments.



Case 3-15. Monteggia fracture-dislocation. Lateral, AP, and oblique views of the elbow. Anterior angulation of a proximal ulnar shaft fracture and anterior radial head dislocation is the sine qua non for type I Monteggia fracture.




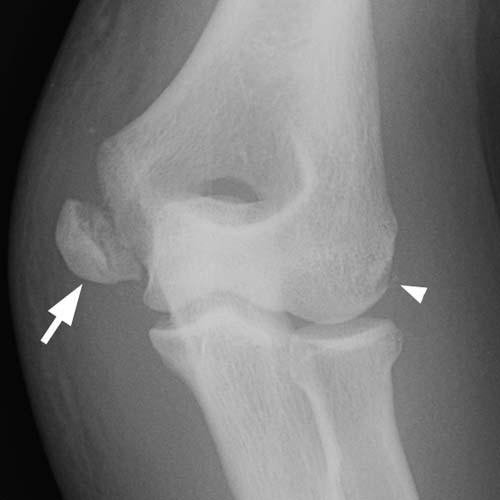
Case 3-16. Monteggia fracture-dislocation. AP, lateral, and oblique views of the elbow. Posterolateral dislocation of the radial head (arrow) is seen with posteriorly angulated ulnar fracture (arrowhead). This is a Monteggia type II fracture pattern.


Case 3-17. Open Monteggia fracture-dislocation. PA and lateral views of the forearm. There is fracture of the ulnar shaft, apex anterior, and open anterior dislocation of the radial head. This is an open Monteggia type I fracture pattern.



Case 3-18. Monteggia fracture-dislocation. AP, oblique, and lateral, views of the elbow. There is fracture of the ulna with apex lateral angulation (arrowhead) and lateral radial head dislocation (arrow), or type III Monteggia. In Monteggia injuries, the orientation of the ulnar angulation predicts the direction of radial head dislocation.



Case 3-19. Monteggia fracture-dislocation. Oblique and lateral views of the elbow. There is a fracture of the ulna with apex anterior and anterior radial head dislocation, and fracture of the radial neck, consistent with type IV Monteggia.




Case 3-20. Monteggia fracture-dislocation. AP and lateral views of the elbow. There is an apex posterior proximal ulna fracture (arrowhead) with posterior fracture-dislocation of the radial head (arrow). This is a variant of a Monteggia type III.


Case 3-21. Monteggia fracture-dislocation. AP, and lateral views of the forearm. There are fractures of the radius and ulna and anterior radial head dislocation, consistent with type 4 Monteggia. Only 1-5% of Monteggia injuries are of this type [11-13].



Case 3-22. Essex-Lopresti fracture. PA view of the forearm and wrist and AP view of the elbow. There is proximal radial fracture dislocation associated with distal radioulnar disruption. Proximal radial fracture with distal radioulnar dislocation, with or without proximal radial head dislocation is an Essex-Lopresti injury [14]. Incidentally noted is a scaphoid fracture. Distal radial and carpal fractures can be seen with proximal radial fractures [15]. The mechanism of injury is longitudinal compression with forces transmitted down the interosseous membrane, which is also injured. This injury is unstable and needs to be corrected at both ends for a proper outcome.




Case 3-23. Radial neck fracture. Lateral, capitellum and AP views of the elbow. The capitellum view is a lateral view with 45 degrees cephalad angulation, and is specifically for evaluating the capitellum and radial head. Radial head and neck are the most frequent adult injuries to the elbow and constitute 50% of these injuries [16]. The lateral view demonstrates a posterior fat pad sign. The posterior fat pad is normally invisible, however displacement of the fat pad posteriorly from joint effusion makes it perceptible. The anterior fat pad is anteriorly displaced (spinnaker sail sign). There is a step-off at the radial neck on the lateral view suggestive of impaction fracture. The supinator fascial plane is convex and displaced anteriorly on the lateral view. Obliteration or displacement of the supinator fascial plane is a constant finding in radial head or neck fractures [17]. These injuries are the most frequent adult elbow injury. Oblique views may be required to detect the fracture.


Case 3-24. Radial head subluxation (nursemaids’ elbow). Lateral and AP views of a child’s elbow. The radius and capitellum should be collinear on all projections. In this case the position of the radial head, which is not yet ossified, can be estimated by the radial neck. The line falls posterior to the capitellum, therefore there is posterior subluxation of the radial head. This is known as nursemaids’ elbow. The mechanism is from pulling a toddler’s hand by an adult. Before 5 years of age, the annular ligament is not taught and can lead to radial head subluxation out of the ligament when the forearm is pulled in pronation [18]. Supination may return the radial head to its proper location, and therefore the initial subluxation may be undetected on radiographs when interval supination has occurred.




Case 3-25. Radial head fracture. AP, lateral, radial head, and capitellum views of the elbow. A minimally displaced radial head fracture is seen on the capitellar view (arrow). The capitellar view is suited specifically for evaluation of the capitellum and proximal radius. The supinator fascial plane is indistinct, which is a reliable sign of proximal radial injury. Anterior and posterior fat pads are visible (arrowheads). The absence of a fat pat sign in an adult does not preclude radial head fracture. Step-off of 2 mm or more can predispose to osteoarthritis and may serve as an indication for surgery.


Case 3-26. Posterior elbow dislocation. AP and lateral views of the elbow. There is a posterior elbow dislocation. Most elbow dislocations are posterior or posterolateral (80-90%). The radius and ulna typically dislocate in the same direction.


Case 3-27. Posterior elbow dislocation. AP and lateral views of the elbow. There is a posterior dislocation with impaction fracture of the volar radial head. Most elbow dislocations occur in conjunction with fractures. Most commonly, this involves the medial epicondyle and second most commonly the radial head, as depicted here.



Case 3-28. Elbow fracture-dislocation. Lateral, AP, and capitellum views of the elbow. There is an oblique fracture through the olecranon with volar dislocation of the radius and distal ulnar fragment from the distal humerus. Soft tissue swelling of the olecranon bursa is seen. This is an anterior fracture-dislocation of the elbow. It bears resemblance to the Monteggia fracture pattern however the ulnar fracture involves the olecranon and the proximal radioulnar joint is intact. Fractures involving the anterior trochlear notch are highly associated with anterior dislocation.




Case 3-29. Elbow fracture-dislocation. AP, oblique, and lateral views of the elbow. Fracture of the proximal ulna and severely comminuted displaced fractures of the proximal radius and posterior dislocation of the ulna.

Case 3-30. Olecranon fracture. Lateral view of the elbow. There is a minimally displaced olecranon fracture. Simple oblique fracture of the olecranon are generated by valgus forces on an extended elbow. Olecranon bursal swelling is present. Inability to extend the elbow occurs with olecranon fractures and may preclude the ability to obtain an AP radiograph. Most olecranon fractures are transverse and occur at the trochlear notch [19]. Olecranon fractures are the second most common injury in the adult after proximal radial fractures and are responsible for 20% of elbow injuries.



Case 3-31. Capitellar fracture. Lateral, AP, and oblique views of the elbow. There is a joint effusion and displaced capitellar fracture. Shearing forces from radial head or lateral trochlear groove may produce this fracture pattern.




Case 3-32. Capitellar fracture in a 45-year-old woman in a bicycle accident. Lateral, capitellum, and AP views of the elbow. There is a large joint effusion and a displaced capitellar fracture. The fragment typically lies above the radial head as seen here. Rotation of the fragment may occur. Lateral projections are essential as the frontal view will not show this fracture well.

Sagittal CT image. The capitellar fragment includes the articular surface. The fragment is displaced, rotated 90 degrees, and anteriorly dislocated, relative to the radial head. Less commonly, the capitellar fragment may be displaced laterally or posteriorly [20]. Most capitellar fractures have complex involvement of the articular surfaces of both the capitellum itself as well as the trochlea [21].



Case 3-33. Supracondylar fracture. Oblique and lateral views of a child’s elbow. There is a joint effusion, manifested by posterior fat pad sign and elevation of the anterior fat pad. Posterior fat pad is highly associated with fracture (70-90% ) in children and adolescents [22-23]. The anterior humeral line normally intersects the middle 1/3 of the capitellum. In this case the anterior humeral line intersects the anterior 1/3 of the capitellum, which is diagnostic for a supracondylar fracture. These are the most common fractures seen in children (60%). Fracture traverses the condyles and into the olecranon fossa and coronoid fossa. The mechanism is fall on outstretched hand. A potential complication is radial artery injury with Volkmann’s contracture of the forearm and hand.

Case 3-34. Lateral condylar fracture. Oblique view of a child’s elbow. There is a fracture at the lateral condyle. After supracondylar fractures, lateral condylar fractures rank highest and make up 15 to 20% of childhood elbow injuries. The fracture fragment includes the lateral metaphysis, capitellum, and lateral trochlea. Fall on an outstretched hand with forearm supination and elbow varus angulation is the mechanism. Pull from the extensor attachment at this site contributes to the fracture and can cause distal and posterior displacement of the fragment. The oblique view is best suited for detecting this fracture.


Case 3-35. Medial epicondyle fracture. PA and lateral view of a child’s elbow. The medial epicondyle is rotated and displaced. Common flexor-pronator tendons and medial ulnar collateral ligament originate here. Technically it is an apophysis, since it does not participate in increasing bone length. Valgus force with traction from the flexor-pronator tendon gives rise to avulsion injury, with inferior displacement, as seen here. This is also known as little leaguer’s elbow, due to its frequency in pitchers. A potential complication is entrapment of the ossification center in the joint. There may be no evidence of joint effusion, as the medial epicondyle can be entirely extra-articular [24]. Ulnar nerve which runs posterior to the medial epicondyle, may also be injured.

Case 3-36. Medial epicondyle fracture. PA and oblique views of a 13-year-old girl’s elbow. Elbow fracture dislocation sustained while performing gymnastics. Note that at this age in a female, all of the physes and apophyses are closed. The elbow dislocation has been previously reduced. There is a displaced avulsion fracture of the medial epicondyle (arrow), with proximal retraction and marked overlying soft tissue swelling. There is also an avulsion fracture at the proximal attachment of the ulnar collateral ligament (arrowhead).


Case 3-37. Distal humeral fracture. AP, lateral, and oblique views of the elbow. There is a T-shaped distal humeral fracture. The mechanism of injury is falling on a flexed elbow. The articular part of the fracture typically lies between the trochlear groove and capitellotrochlear sulcus. This fracture then extends into horizontal (T) or oblique (Y) components into the condyles which are displaced by their respective muscle attachments. Distal humeral fractures have been divided into groups [25]. Type A are extra-articular. Type B are intra-articular unicondylar. Type C are bicondylar intra-articular fractures. Type A are further divided into A1 which are medial epicondylar, and Type 2 which are supracondylar, and type 3 which are comminuted supracondylar. B1 is a lateral condylar fracture and B2 is a medial condylar fracture. C1 is a Y- or T shaped fracture. C2 also has a comminuted fracture of the distal humeral shaft. C3 is comminuted intercondylar of the distal shaft and articular surface. 95 % are intra-articular and therefore type B or C. The fracture pattern seen here is C1, which is the most common, and found in 50% of cases [26].



Case 3-38. Transcondylar fracture. AP, oblique, and lateral view of the elbow. There is a fracture that extends transversely across the distal humerus at the level of the condyles. The fracture does not extend distally to separate the condyles from each other. These are the adult counterpart of supracondylar fractures in children. The condyles and olecranon fossa are disrupted. These are uncommon. Non-displaced fractures are treated with immobilization and displaced fractures are treated with ORIF [27].



Case 3-39. Humeral shaft fracture. AP, lateral, and oblique views of the elbow. There is a comminuted distal humeral fracture with a butterfly fragment. Angulation by itself produces a transverse fracture pattern in the humerus, while angulation in conjunction with torsion produces a butterfly fragment as seen here.
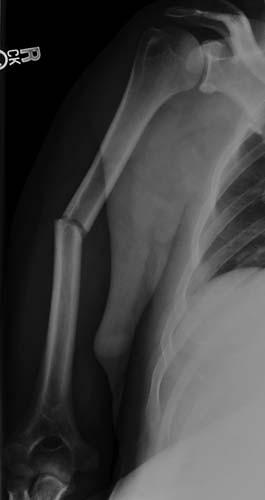

Case 3-40. Humeral shaft fracture. AP and lateral view of the humerus. There is a transverse mid-humeral shaft fracture with apex posterior and lateral. Most humeral fractures are transverse and most occur in the mid-shaft as seen here. Mechanism of injury include direct blow, fall, motor vehicle crash, and torsional stress from athletic activities. Up to 17% may also sustain radial nerve injuries which may manifest as wrist drop [28]. Proximal to the deltoid insertion results in medial displacement of the proximal fragment by the pectoralis muscles, and distal to the deltoid tuberosity leads to abduction of the proximal fragment, as seen here. Humeral shaft fractures are usually treated with a hanging cast. The high degree of mobility of the shoulder, which is a ball and socket joint, rotational and angular deformities of the humerus are not indications for surgery. A hinge joint such as at the knee and ankle does not afford varus or valgus or rotational deformities and tibial fractures with such deformities necessitate surgical correction.

Case 3-41. Humeral shaft fracture. AP radiograph of the humerus. There is a spiral fracture of the humeral shaft with minimal displacement. Spiral fractures are caused by loading under torsion (twisting). The fracture line follows the entire circumference of the bone in a spiral with a vertical component connecting the two ends. Spiral fractures may be left-handed or right-handed, depending on the direction of the spiral.



Case 3-42. Open distal humeral fracture dislocation with extrusion. AP, lateral, and oblique views of the humerus. There is an open humeral fracture with a segment of the bone extruded beyond the soft tissues onto the surface of the body. This is a high energy injury and requires surgical treatment. Nerve palsies are more common [29]. Wound treatment includes debridement, irrigation and prophylactic IV antibiotic therapy. Distal humeral defects can be treated with bone graft such as from the fibula [30].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree