, Gila Perk2, Natesa G. Pandian3, Hans-Joachim Nesser4 and Itzhak Kronzon2
(1)
Department of Cardiology, Cardiocentro Ticino, Lugano, Switzerland
(2)
Non-Invasive Cardiology, Lenox Hill Hospital, New York, NY, USA
(3)
Tufts University School of Medicine, Boston, MA, USA
(4)
Department of Medicine Elisabethinen, Teaching Hospital, Linz, Austria
Abstract
Percutaneous mitral commissurotomy (PMC) was one of the first catheter-based therapies for structural heart disease and has now become the treatment of choice for selected patients with rheumatic mitral stenosis. Inoue’s single-balloon technique has become the most popular method for performing PMC in most institutions today. The traditional tools of invasive cardiologist (i.e. fluoroscopy and hemodynamic pressure measurement) are inadequate for this procedure, and transoesophageal echocardiography (TEE) has become an essential component. Real time three-dimensional transesophageal echocardiography (RT 3D TEE) has greatly expanded the visualization of mitral stenosis. It provides detailed morphology of leaflets and commissures, and permits accurate planimetry of the valve. It is likely that RT 3D TEE will be used as a primary modality for guiding PMBV in the future. In this chapter we will describe the RT 3D TEE morphology of mitral stenosis, and how RT 3D TEE may add useful information in each stage of the procedure.
Electronic supplementary material
The online version of this chapter (doi:10.1007/978-1-4471-4745-9_4) contains supplementary material, which is available to authorized users.
Percutaneous mitral commissurotomy (PMC) was one of the first catheter-based therapies for structural heart disease and has now become the treatment of choice for selected patients with rheumatic mitral stenosis. Inoue’s single-balloon technique has become the most popular method for performing PMC in most institutions today. The traditional tools of invasive cardiologist (i.e. fluoroscopy and hemodynamic pressure measurement) are inadequate for this procedure, and transoesophageal echocardiography (TEE) has become an essential component.
Two-dimensional transthoracic echocardiography (2D TTE) plays a major role in the selection of suitable patients for PMC. Traditionally, the morphologic assessment of the stenosis with regard to the feasibility and safety of PMC has used a mitral valve score. The Massachusetts General Hospital Score (Wilkins score) is one of the most popular and widely adopted. This score evaluates four criteria—leaflet mobility and thickening, calcifications, and chordal involvement—on a scale of 0–4. Mitral valve morphology is considered suitable for PMC if the total score is less than 8. Because PMC results in commissural splitting, a limitation of this scoring system is the lack of information on commissural calcifications. Today, inclusion criteria for PMC have been simplified, taking into consideration the absence of commissural calcification, absence of moderate to severe mitral regurgitation, pliability/mobility of the anterior mitral leaflet, and absence of thrombi in the left atrium or left atrial appendage.
Once the decision to perform PMC has been made, 2D TEE during the procedure is of great value. In patients with distorted anatomy due to an enlarged left atrium (which is almost always the case in patients with severe mitral stenosis), 2D TEE is used to guide the transseptal puncture and positioning of the balloon across the mitral valve. Moreover, it is used to assess for the presence of complications such as perforation or tamponade and for mitral regurgitation due to leaflet tear.
Three-dimensional transoesophageal echocardiography (3D TEE) has greatly expanded the visualization of mitral stenosis. It provides detailed morphology of leaflets and commissures and permits accurate planimetry of the valve. It is likely that 3D TEE will be used as a primary modality to guide PMC in the future. This chapter describes the 3D TEE morphology of mitral stenosis and discusses how 3D TEE may add useful information in each stage of the PMC procedure.
4.1 Three-Dimensional TEE in Mitral Stenosis
The most relevant advantages of 3D TEE over 2D TEE in studying the morphology of mitral stenosis include (1) enhanced evaluation of mitral commissural fusion, (2) better visualization of the extent of commissural calcifications, (3) better assessment of leaflet pliability, and (4) more accurate planimetry of valve area.
The ‘3D zoom mode’ (which acquires 3D images over one beat) is preferred over the wide-angle full-volume mode (which merges four to seven narrow pyramidal data sets and may suffer from artifacts due to arrhythmias). Because of the relatively small size of the annulus, the truncated pyramidal data set may be narrowed to allow high-quality images with an acceptable frame rate. Moreover, there are no limitations related to arrhythmias.
From the ‘surgical’ view, typical pathological details of the leaflets are evident. In less-disrupted valves, the posterior leaflet loses its indentations; the fusion of the indentations between the scallops is one of the earliest pathological abnormalities of rheumatic mitral valve stenosis. The anterior leaflet may be fibrosed and thickened at the free margin (Fig. 4.1a). In severe stenosis, the leaflets form a unique rigid diaphragm. The residual valve orifice is markedly reduced and assumes a fish-mouth shape (Fig. 4.1b and Video 4.1).
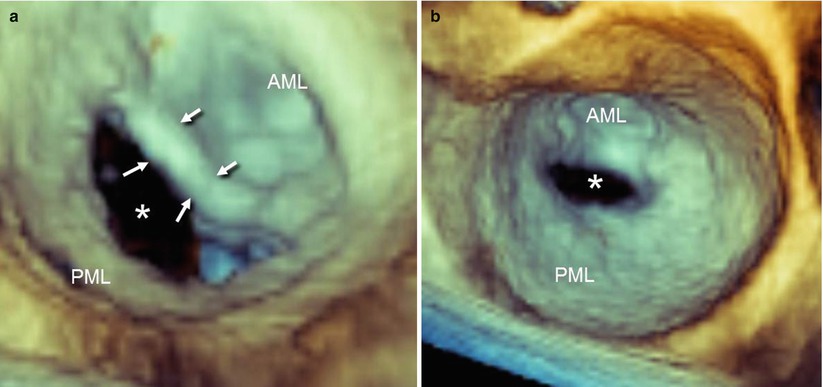
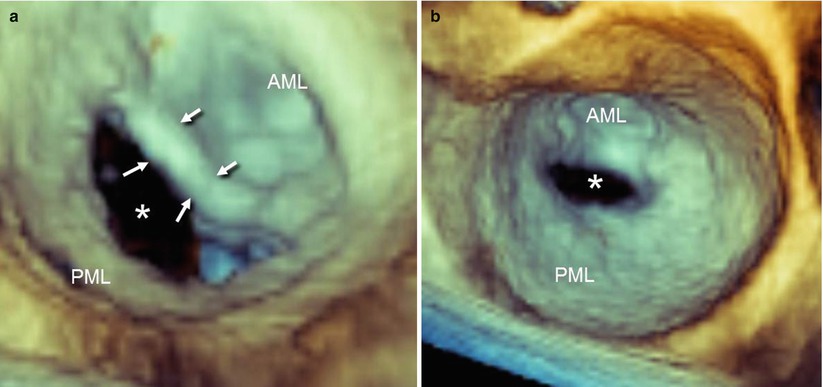
Fig. 4.1
Two cases of mitral stenosis, in which 3D TEE from the atrial perspective (surgical view) shows typical pathological details. (a) In the less-disrupted valve, the free margin of the anterior mitral leaflet (AML) is thickened (arrows), and the indentations of the posterior mitral leaflet (PML) are no longer visible. (b) In severe mitral stenosis, both leaflets form a unique diaphragm. The residual valve area (asterisk) is markedly reduced and appears longer in the horizontal than in the vertical dimension; as the leaflets taper smoothly at each commissure, the orifice assumes a fish-mouth shape
4.1.1 Commissural Fusion
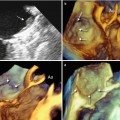
The extent of commissural fusion cannot be fully appreciated with the 2D TTE short-axis view. From an anatomic standpoint, the stenosed mitral valve has a funnel-shaped morphology. The commissural fusion extends from the annulus to the deepest and narrowest orifice. Because the fusion traverses multiple cross-sectional planes, a single plane would assess the commissural fusion only at that cross section. Thus, multiple adjacent parallel planes are needed to evaluate the whole extent of the fusion (which may be difficult with the 2D TTE short-axis view and the 2D TEE transgastric short-axis view). Conversely, 3D TEE allows visualization of the entire funnel-shaped configuration in a single volumetric database, and commissural fusion can be assessed from the most favourable perspectives. One of the preferred ways to evaluate commissural fusion is from the left ventricular perspective. From this perspective, both commissures can be evaluated and graded according to Carpentier’s classification: grade I is a partial fusion of the commissures; grade II is complete fusion of commissures with a visible delineation between the anterior and posterior leaflets; grade III is a complete fusion of one or both commissures with no visible delineation between the anterior and posterior leaflets (Fig. 4.2).
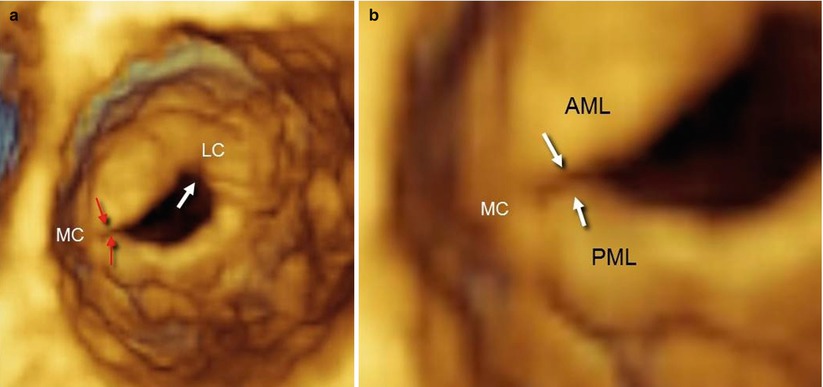
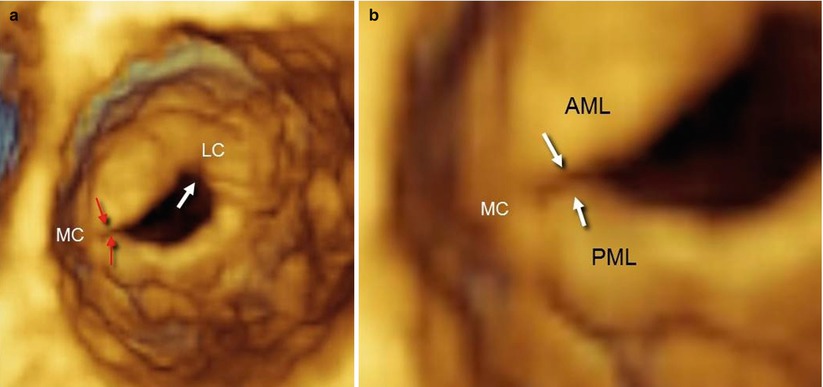
Fig. 4.2
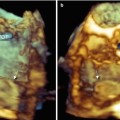
(a) From the ventricular perspective, 3D TEE shows the complete fusion of the medial commissure (MC) with a visible delineation between the anterior and the posterior leaflets (grade II in Carpentier’s classification; red arrows), and a complete fusion of lateral commissure (LC) with no visible delineation between leaflets (grade III, white arrow). (b) A magnified image of the medial commissure shows at least partial delineation of the anterior mitral leaflet (AML) and posterior mitral leaflet (PML). This pathological arrangement of commissures can also be described as asymmetric fusion
A slight right-to-left rotation from this perspective may better show the lateral commissure (Fig. 4.3a), and left-to-right rotation may better expose the medial commissure (Fig. 4.3b).
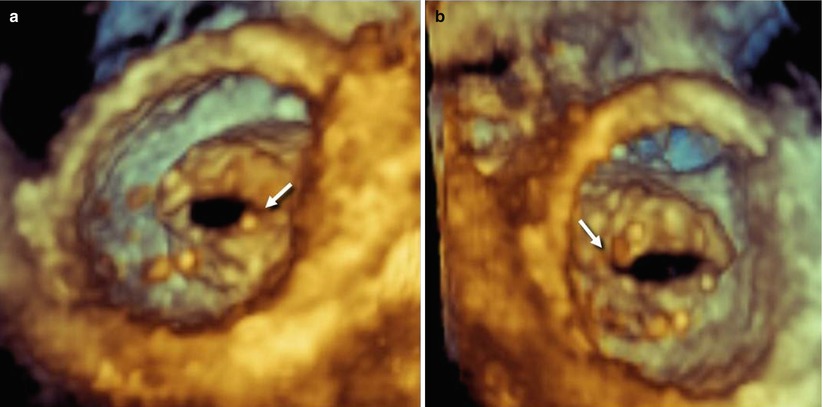
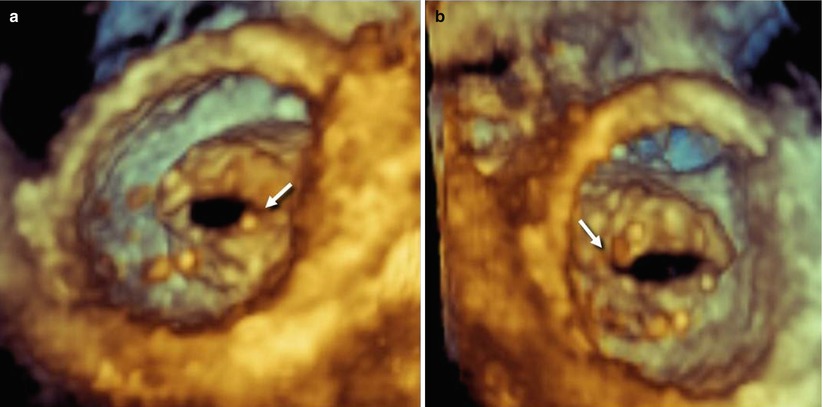
Fig. 4.3
(a) After slight right-to-left rotation from the ventricular perspective, 3D TEE permits better visualization of the lateral commissure (arrow). (b) Slight left-to-right rotation permits better visualization of the medial commissure (arrow). In this patient, both commissures can be classified as grade II, as there is a visible delineation between the anterior and the posterior leaflets. This pathological arrangement of commissures can also be described as symmetric fusion
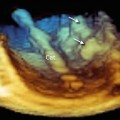
Because of the appreciation of the third dimension, commissures can also be visualized from a perspective similar to the 2D TEE long-axis view (Fig. 4.4




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree