Author
No. of patients/nodules
Tumor size (cm)
Treatment
Median operating times (mins)
Technical effectiveness (%)
Total/local recurrence (%)
Median survival time (mons)
Survival rate (%)
Complications (%)
Follow-up (months)
1-
3-
5-year
Yamamoto et al. [4]
7/7
N/A
Hepatic resection
890
N/A
85.7/N/A
39
N/A
N/A
57.1
42.9
118
Aoki et al. [6]
9/9
3.2
Hepatic resection
600
N/A
88.9/N/A
25.8
N/A
N/A
N/A
66.7
N/A
Hemming et al. [7]
16/16
N/A
Hepatic resection
N/A
N/A
N/A
N/A
88
50
N/A
36
22
Teratani et al. [28]
81/81
2.7
RFA
34
N/A
N/A/3.1
N/A
N/A
N/A
N/A
4.8
N/A
Lu et al. [29]
N/A/31
2.4
RFA
N/A
52
N/A/14.3
N/A
N/A
N/A
N/A
6.4
11.3
Ren et al. [32]
18/18
2.8
MWA
N/A
94.4
N/A/5.6
N/A
100
N/A
N/A
5.6
15
Huang Shijia [33]
139/163
2.5
MWA
10.4
96.3
N/A/13.5
N/A
94
72
64
14.4
24.5
Technical points are as follows: (1) Theoretical merits of MWA make it produce higher intratumoral temperatures, larger ablation zones, less ablation time, and less dependence on the electrical conductivities of tissue consistently. Also, the energy delivery is less controlled by the exponentially rising electrical impedance of tumor tissue. (2) According to our experience, long-duration ablation (about 1 min more than the ablation time of tumors in safe sites) may cause gradual ablation of the tumors adjacent to large vessels and compensate the defect from heat-sink effect in the large vessels. (3) After the first procedure, contrast-enhanced imaging (CEUS, computed tomography, or magnetic resonance imaging) should be performed in time in the following 3 days to examine whether any residual cancer still have not been eliminated. Consequently, a second session will be determined to achieve complete ablation. (4) With MWA emission, ethanol ablation should be performed at the same time for tumors adjacent to both large vessels and bile ducts. The purpose of the procedures is to wipe out the tumor tissue adjacent to the biliary duct and blood vessel and to avoid the overheating injury to those vital tissues by means of increasing thermal conduction and diffusivity [27]. (5) Real-time peritumoral temperature monitoring should be used as an indicator for complete MWA. (6) Rich experience in detailed treatment protocol, accurate image guiding, and proper placement of antennas contribute a lot for the success of the treatment (Figs. 7.1 and 7.2) [33].



Fig. 7.1
Contrast-enhanced magnetic resonance imaging (MRI) of a 48-year-old man shows a 4.1 × 3.4 cm nodule of hepatocellular carcinoma (HCC) adjacent to the inferior vena cava (black arrows in b and c) treated by microwave ablation (MWA). (a) Preablation image shows one neoplasm (white arrows) adjacent to the inferior vena cava (black arrow). (b) On the arterial phase image obtained in the 12th month after treatment, no enhancement is seen in the ablation zone (white arrows). (c) Transverse and (d) coronal images show that there remains no enhancement of the ablation zone (white arrows in c and black arrows in d) in the 36 months after treatment

Fig. 7.2




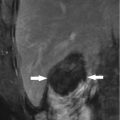
Contrast-enhanced images show a 3.3 × 2.3 cm HCC nodule adjacent to the right portal vein (white arrows in e and f) in the liver of a 63-year-old man treated with MWA. (a) Preoperative contrast-enhanced ultrasound (CEUS) and (b) transverse and (c) coronal preoperative MRI show that there is one HCC nodule (white arrows) with hyperenhancement during the arterial phase of CEUS, with high signal during the arterial phase of MRI and with low signal during the portal phase of MRI. The lesion is in front of the right portal vein (black arrow). (d) After one session, the nodule (white arrows) which is close to the blood vessel (black arrow) was completely ablated. (e) On the arterial phase image obtained in 12 months after treatment, no enhancement is seen in the ablation zone (black arrows). And (f) the arterial phase image shows that there remains no enhancement of the ablation zone (black arrows) in 24 months after treatment
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree