Fig. 10.1
The curve of the temperature monitor during microwave ablation (MWA) for a metastatic hepatic tumor abutting the small intestine. The temperature of the marginal tissue of the tumor neighboring the gastrointestinal tract is monitored and controlled to fluctuate between 45 and 52 °C during the whole treatment procedure according to the abdominal operation history of the patient
10.4 Adjuvant Therapy with EA of Small Dose
For tumors protruding or in contact with the GIT, one to two 21G PTC needles could be placed into marginal tissue of the tumor proximal to the GIT under US guidance. A small dose (<20 ml for per session) of dehydrated, sterile, 99.5 % ethanol could be slowly injected into the marginal tissue of the tumor during the process of ablation treatment until the marginal tissue of the tumor proximal to the GIT is completely overlapped with hyperechogenicity.
10.5 Clinical Effect
Our latest data of MWA for 175 hepatic tumors abutting the GIT show that the complete ablation rate is 96.5 % (169/175) and local tumor progression is 10.1 % (17/169) (Figs. 10.2, 10.3, 10.4, and 10.5) which is similar with the results of our previous published paper [15, 16].









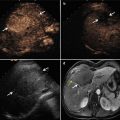
Fig. 10.2
A 44-year-old man with a history of chronic hepatitis B, cirrhosis, and splenectomy is found to have a hepatic lesion (6.0 × 5.4 × 5.4 cm) located in the right anterior lobe and abutting the small intestine. The lesion is diagnosed to be hepatocellular carcinoma (HCC) and treated with MWA and ethanol ablation (EA). (a) The hepatic lesion located in the right anterior lobe (arrow) is hypervascular and adjacent to the small intestine on contrast-enhanced computed tomography before treatment. (b) The hepatic lesion abutting the small intestine (arrow) is slight hyperechoic with obscure margin on B-mode ultrasound (US) before treatment. (c) Color and pulsed Doppler flow image before treatment shows arterial blood flow signals appearing within and around the lesion. (d) The lesion (arrow) highly enhances in the early arterial phase with irregular and multiple nodules fusion shape slightly protruded from liver capsule on contrast-enhanced US before treatment. (e) The lesion (arrow) is treated with MWA with two antennas and three insertions of antenna under powers of 60 W. One 21G thermocouple needle is inserted under US guidance into the edge of the lesion abutting the intestine to survey the temperature of the marginal tissue of the tumor and control MW emission. The temperature cutoff of ablation therapy is set at 50 °C. (f) Four days after MWA, contrast-enhanced US shows a no-enhancement area of 6.0 × 6.0 × 5.8 cm in the treatment region (arrow). (g) Magnetic resonance imaging (MRI) obtained 23 months after MWA finds a new lesion adjacent to ablation zone which shows high enhancement in arterial phase on contrast-enhanced T1-WI (arrow). (h) The new lesion adjacent ablation zone is central low enhancement in portal venous phase on contrast-enhanced T1-WI MRI (arrow). (i) Contrast-enhanced US performed 23 months after MWA shows two hypervascular lesions with size of 1.6 × 1.3 cm and 1.3 × 1.0 cm near the marginal site of the no enhanced ablation zone abutting the intestine in the arterial phase (arrow). The two lesions are treated with EA. (j) On MRI obtained 50 months after MWA, local tumor progression is not found (arrow)

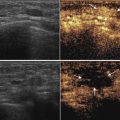
Fig. 10.3
An 88-year-old man without a history of chronic hepatitis is found with a hepatic lesion (3.5 × 2.8 × 2.6 cm) located in the right posterior lobe and abutting the small intestine. The lesion is diagnosed to be HCC with contrast-enhanced images and treated with MWA and EA. (a) The hepatic lesion located in the right posterior lobe is heterogeneously hypervascular and adjacent to the small intestine (arrow) on contrast-enhanced MRI before treatment. (b) The lesion is highly enhanced (arrow) on contrast-enhanced US before treatment. (c) The lesion is treated with MWA (arrow) with two antennas under powers of 50 W and EA (total dose 7.5 ml) with three 21G PTC needles. One 21G thermocouple needle is inserted under US guidance near the capsule of liver abutting the intestine. The temperature cutoff of ablation therapy is set at 50 °C. (d) Seven days after MWA, contrast-enhanced US shows a no-enhancement area of 3.7 ×3.2 ×2.7 cm in the treatment region without residual focus (arrow). (e) On MRI obtained 12 months after MWA and EA, the treated lesion abutting the intestine has no enhancement in arterial phase on contrast-enhanced T1-WI and local tumor progression is not found (arrow). (f) Contrast-enhanced US performed 12 months after MWA and EA; the treated lesion has totally no enhancement (arrow). (g) Local tumor progression is not found (arrow) on MRI obtained 18 months after MWA and EA


Fig. 10.4
A 55-year-old man with a history of chronic hepatitis B, cirrhosis, and transcatheter arterial chemoembolization for HCC is found with a hepatic lesion (5 cm) located in the left lateral lobe and adjacent to stomach. The lesion is diagnosed to be HCC combined with history and contrast-enhanced images and treated with MWA and EA. (a) The hepatic lesion located in the left lateral lobe (arrow) is hypointense and adjacent to stomach on T1-WI MRI before treatment. (b) The hepatic lesion is hyperintense (arrow) on T2-WI MRI before treatment. (c) The hepatic lesion is hyperintense (arrow) on DWI MRI before treatment. (d) The hepatic lesion is highly enhanced in the arterial phase (arrow) of contrast-enhanced MRI before treatment. (e) The hepatic lesion located in the left lateral lobe has no enhancement in the arterial phase (arrow) of contrast-enhanced MRI obtained 19 months after MWA and EA. (f) The ablated area is larger than and has completely covered the treated HCC lesion on the delayed phase (arrow) of MRI obtained 19 months after MWA and EA


Fig. 10.5
A 53-year-old man with a history of chronic hepatitis B, cirrhosis, and transcatheter arterial chemoembolization for HCC is found with a hepatic lesion (2.1 × 1.8 cm) located in the right anterior lobe and adjacent to intestine. The lesion is diagnosed to be HCC combined with history and contrast-enhanced images and treated with MWA and EA. (a) The hepatic lesion located in the right anterior lobe has high intensity and is adjacent to the intestine (arrow) on T2-WI MRI before treatment. (b) The hepatic lesion adjacent to intestine is highly enhanced (arrow) on contrast-enhanced T1-WI MRI before treatment. (c) On contrast-enhanced US before treatment, the hepatic lesion of the right anterior lobe adjacent to the intestine is hypervascular (arrow). (d) On T1-WI MRI obtained 17 months after MWA and EA treatment, the hepatic lesion of the right anterior lobe adjacent to the intestine (arrow) is heterogeneous. (e) On contrast-enhanced T1-WI MRI obtained 17 months after treatment, the hepatic lesion of the right anterior lobe adjacent to the intestine had no enhancement and local tumor progression is not found (arrow)
RFA for hepatic tumors abutting GIT is reported by several authors using different protective methods (Table 10.1). Artificial ascites is usually used as a protective method in percutaneous RFA through which the GIT was satisfactorily separated from 78 to 91.7 % lesions with 3.1–17.5 % local tumor progression rate and low rate of major complications [6–9]. Although the separating rate between the GIT and liver could not reach 100 %, artificial ascites is an easy and feasible method in majority of patients with hepatic tumor abutting the GIT. Temperature monitor during thermal ablation is another method to protect extrahepatic organs. The thermocouple needle should be inserted accurately into the site of tumor margin abutting the GIT and should be monitored continuously during ablation to timely discover the possible movement of thermocouple needle. Moreover, abdominal adhesion after abdominal operation may cause separation between the liver and GIT to be difficult; artificial ascites technique is suitable for patients without abdominal operation history. Different from it, Temperature monitor do not get restricted by abdominal operation history. The complete ablation rate of our result is similar with that of MWA and RFA for hepatic tumors reported in large clinical series [17, 18] and that of RFA combined with artificial ascites for hepatic tumors abutting the GIT [6–9]. Local tumor progression is similar with other reports of percutaneous thermal ablation for hepatic lesions adjacent to the GIT (Table 10.1) [6–13].
Table 10.1
Clinical studies reporting outcomes of thermal ablation for hepatic lesions abutting the gastrointestinal tract
Authors | Number of patients
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|
|---|