Chapter 8 Pericardium
Pericardial effusion and tamponade
Congenital pericardial disorders
Pericardium
Introduction
The pericardium stabilizes the heart within the thorax and maintains cardiac efficiency. Pericardial disease is associated with a large range of symptoms from mild discomfort to haemodynamic collapse. Pericardial disease often presents a diagnostic conundrum, and its diagnosis is a good example of multimodality cardiovascular imaging. Echocardiography provides acute assessment of the pericardium, in particular the amount and impact of pericardial fluid. Cardiac CT and MR provide detailed investigation of the pericardial tissue and a wider field of view to look for related disease.
Anatomy
The pericardium consists of a fibrous pericardium which superiorly blends into the aorta and pulmonary arteries and inferiorly attaches to the diaphragm, sternum, and vertebrae. Within this is the serous pericardium, consisting of two membranes that move over each other lubricated by a small amount of pericardial fluid (10–50mL). There are two holes within the pericardium: one to accommodate the aorta and pulmonary artery, and the other to accommodate the pulmonary veins and vena cavae. Two pockets (or sinuses) are created by these holes: the transverse sinus between the aorta and the pulmonary artery, and the oblique sinus between the pulmonary veins.
Pathology
Abnormalities of the pericardium have significant haemodynamic consequences because they restrict normal cardiac function.
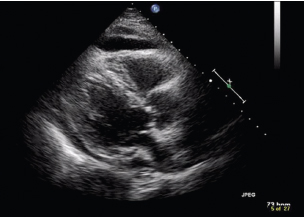
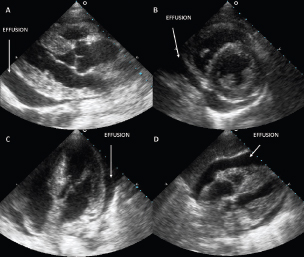
 The serous membranes provide a potential space for fluid accumulation (pericardial effusion) (Fig. 8.1), and increases in intrapericardial pressure related to this fluid can restrict cardiac function (cardiac tamponade).
The serous membranes provide a potential space for fluid accumulation (pericardial effusion) (Fig. 8.1), and increases in intrapericardial pressure related to this fluid can restrict cardiac function (cardiac tamponade).
 Changes in pericardial compliance due to fibrosis, such as that associated with chronic inflammation after infection or surgery, can also restrict cardiac function (constrictive pericarditis).
Changes in pericardial compliance due to fibrosis, such as that associated with chronic inflammation after infection or surgery, can also restrict cardiac function (constrictive pericarditis).
 Masses can be found within the pericardium—benign such as pericardial cysts and malignant such as pericardial mesothelioma. These can alter pericardial compliance as well as causing pericardial effusions or direct compression of the cardiac chambers.
Masses can be found within the pericardium—benign such as pericardial cysts and malignant such as pericardial mesothelioma. These can alter pericardial compliance as well as causing pericardial effusions or direct compression of the cardiac chambers.
 Congenital abnormalities of the pericardium include partial or complete agenesis of the pericardium which may have no functional significance or, if chambers are herniated, may lead to haemodynamic impairment.
Congenital abnormalities of the pericardium include partial or complete agenesis of the pericardium which may have no functional significance or, if chambers are herniated, may lead to haemodynamic impairment.
Fig. 8.1 Transthoracic echocardiography subcostal view of a global pericardial effusion. Fluid is evident anterior to the right ventricle and posterior to the left ventricle.
Chest X-ray
As chest X-ray is the standard first-line investigation in patients with chest pain or shortness of breath, this is the usual initial available modality.
Advantages of the chest X-ray
 Widely available.
Widely available.
 Wide field of view to pick up alternative or related pathology such as chest infection.
Wide field of view to pick up alternative or related pathology such as chest infection.
 Identification of calcification.
Identification of calcification.
Disadvantages of the chest X-ray
 Only provides outline of cardiovascular structures against the lung to identify change in shape. Therefore its main use is in identification of a pericardial effusion which may be confused with other causes for an increased cardiac silhouette.
Only provides outline of cardiovascular structures against the lung to identify change in shape. Therefore its main use is in identification of a pericardial effusion which may be confused with other causes for an increased cardiac silhouette.
What can the chest X-ray tell us?
Pericardial disease
 The pericardium itself is not normally visible, except when it becomes calcified. The presence of calcification provides an immediate likely diagnosis of constrictive pericarditis.
The pericardium itself is not normally visible, except when it becomes calcified. The presence of calcification provides an immediate likely diagnosis of constrictive pericarditis.
 Othe irregularities along its border (caused by masses or enlargement of cardiac chambers such as the left atrium in constrictive physiology) and shift of cardiac position within the chest (related to congenital absence of the pericardium).
Othe irregularities along its border (caused by masses or enlargement of cardiac chambers such as the left atrium in constrictive physiology) and shift of cardiac position within the chest (related to congenital absence of the pericardium).
Pericardial space
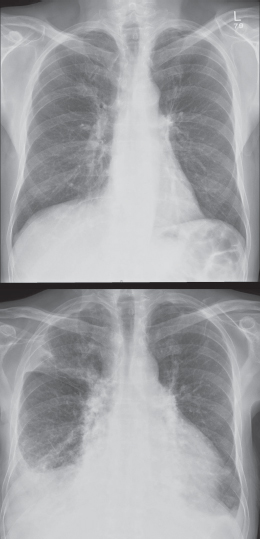
The key information is obtained from change in the shape of the cardiac silhouette related to a pericardial effusion (Fig. 8.2). Specific features are:
 increase in size
increase in size
 a globular heart.
a globular heart.
Fig. 8.2 Two chest X-rays in the same patient taken 6 months apart. The top image is normal but the lower image shows that the cardiac shadow has become globular in appearance, consistent with a pericardial effusion.
Echocardiography
Echocardiography is the initial imaging modality of choice for investigation of possible pericardial pathology.
Advantages of echocardiography
 Readily available within the hospital.
Readily available within the hospital.
 High spatial and temporal resolution to provide information on the quantity and position of fluid within the pericardial space combined with related changes in haemodynamics.
High spatial and temporal resolution to provide information on the quantity and position of fluid within the pericardial space combined with related changes in haemodynamics.
 Can also assess cardiac size, function, and mass.
Can also assess cardiac size, function, and mass.
 Transoesophageal imaging can also assess sinuses.
Transoesophageal imaging can also assess sinuses.
 Some tissue characterization (e.g. the presence of thrombus or fibrin in effusion or masses associated with the pericardium) can be identified. Useful in the emergency setting to assess acute haemodynamic compromise and assist with pericardial drainage.
Some tissue characterization (e.g. the presence of thrombus or fibrin in effusion or masses associated with the pericardium) can be identified. Useful in the emergency setting to assess acute haemodynamic compromise and assist with pericardial drainage.
 Doppler can assess both myocardial and blood velocities to investigate constrictive and restrictive physiology.
Doppler can assess both myocardial and blood velocities to investigate constrictive and restrictive physiology.
Disadvantages of echocardiography
 Field of view does not allow study of related pathology in the chest.
Field of view does not allow study of related pathology in the chest.
 Imaging may be limited by body habitus.
Imaging may be limited by body habitus.
 Limited ability to study tissue characteristics of any pericardial masses.
Limited ability to study tissue characteristics of any pericardial masses.
 Not able to accurately measure pericardial size.
Not able to accurately measure pericardial size.
What can echocardiography tell us?
Part of the pericardium and pericardial space is seen in all standard echocardiography views. Echocardiography is used to identify masses or calcification and accumulation of fluid within the pericardial space. It can be combined with Doppler assessment of valvular flow during respiration to assess cardiac compromise. At the same time a comprehensive assessment of cardiac and valvular function can be performed.
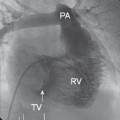
 The best views are the parasternal long- and short-axis, apical four-chamber, and subcostal views (Fig. 8.3).
The best views are the parasternal long- and short-axis, apical four-chamber, and subcostal views (Fig. 8.3).
 During transoeosphageal echocardiography additional views are available, including the four-chamber view (mid-oesophageal 0° view) to assess localized collections around the pulmonary veins and right heart.
During transoeosphageal echocardiography additional views are available, including the four-chamber view (mid-oesophageal 0° view) to assess localized collections around the pulmonary veins and right heart.
 Pericardial surfaces are seen as a thin, slightly brighter line around the heart, but the acoustic properties of the pericardium are similar to surrounding tissue and therefore are difficult to measure accurately. Gross changes in thickness or calcification (which are seen as echo-lucent areas with associated shadowing) may be apparent.
Pericardial surfaces are seen as a thin, slightly brighter line around the heart, but the acoustic properties of the pericardium are similar to surrounding tissue and therefore are difficult to measure accurately. Gross changes in thickness or calcification (which are seen as echo-lucent areas with associated shadowing) may be apparent.
 Pericardial space is seen as a thin black line around the heart, which is usually only a few millimetres thick.
Pericardial space is seen as a thin black line around the heart, which is usually only a few millimetres thick.
Fig. 8.3 Four standard echocardiography views with the pericardial effusion annotated.
Cardiac CT
Cardiac CT is a key modality for more detailed assessment of pericardial pathology that has been identified by echocardiography. Pericardial disease may also be identified during chest CT imaging for investigation of symptoms such as shortness of breath. As the modality has been available for longer than magnetic resonance imaging, it has traditionally been the modality of choice for detailed assessment of pericardial pathology. Multi-detector CT has enabled motion-free imaging of the pericardium to improve resolution, multiplanar re-formation, and options to assess associated changes in cardiac function.
Advantages of cardiac CT
 Ability to provide soft tissue contrast with tissue characterization based on attenuation.
Ability to provide soft tissue contrast with tissue characterization based on attenuation.
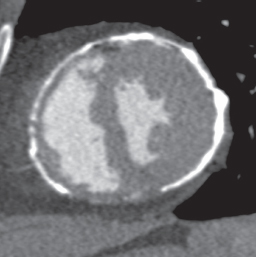
 Ientification of calcification, including microcalcifications (Fig. 8.4).
Ientification of calcification, including microcalcifications (Fig. 8.4).
 Wide field of view allowing identification of associated chest pathology.
Wide field of view allowing identification of associated chest pathology.
Disadvantages of cardiac CT
 Without gating, motion artefacts can make measurements difficult including complicating differentiation of thickened pericardium from fluid.
Without gating, motion artefacts can make measurements difficult including complicating differentiation of thickened pericardium from fluid.
 Requirement for ionizing radiation.
Requirement for ionizing radiation.
 Use of iodinated contrast agents.
Use of iodinated contrast agents.
What can cardiac CT tell us?
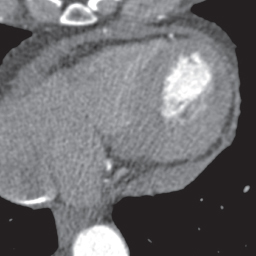
 Pericardial surfaces are seen as a thin grey line of soft tissue density. This is predominantly fibrous pericardium but also incorporates the serous membranes. The presence of pericardial and epicardial fat improves delineation of the pericardium because of the attenuation characteristics of fat. Therefore thickness is best assessed in front of the right ventricle and right atrium where there is an area of ventral mediastinal fat. Thickness is usually 1–2mm, with >4mm considered abnormal (Fig. 8.5). Calcifications suggest constrictive pathology.
Pericardial surfaces are seen as a thin grey line of soft tissue density. This is predominantly fibrous pericardium but also incorporates the serous membranes. The presence of pericardial and epicardial fat improves delineation of the pericardium because of the attenuation characteristics of fat. Therefore thickness is best assessed in front of the right ventricle and right atrium where there is an area of ventral mediastinal fat. Thickness is usually 1–2mm, with >4mm considered abnormal (Fig. 8.5). Calcifications suggest constrictive pathology.
 Pericardial fluid has the attenuation characteristics of water and is seen as a thin line between the pericardial surfaces and the heart. Attenuation characteristics may allow differentiation between transudates (attenuation similar to water) and exudates or haemorrhage (higher protein content with greater attenuation). Because the whole heart is seen, loculated or localized effusions can be imaged.
Pericardial fluid has the attenuation characteristics of water and is seen as a thin line between the pericardial surfaces and the heart. Attenuation characteristics may allow differentiation between transudates (attenuation similar to water) and exudates or haemorrhage (higher protein content with greater attenuation). Because the whole heart is seen, loculated or localized effusions can be imaged.
 Multi-detector CT allows visualization of cardiac function to identify chamber collapse or changes in cardiac chamber size.
Multi-detector CT allows visualization of cardiac function to identify chamber collapse or changes in cardiac chamber size.
 The wide field of view allows assessment of related pathology in the lungs and clearer characterization of the extent of masses associated with the pericardium. Therefore cardiac CT is particularly useful for more detailed assessment of pericardial pathology, in particular pericardial thickness, calcification, and size, and the extent and functional effects of pericardial masses.
The wide field of view allows assessment of related pathology in the lungs and clearer characterization of the extent of masses associated with the pericardium. Therefore cardiac CT is particularly useful for more detailed assessment of pericardial pathology, in particular pericardial thickness, calcification, and size, and the extent and functional effects of pericardial masses.
Fig. 8.4 Cardiac CT short axis view of the left ventricle. Pericardial calcification consistent with constrictive pericarditis is easily seen.
Cardiac magnetic resonance
Cardiac magnetic resonance (CMR) imaging is increasingly used as the modality of choice for more detailed assessment of pericardial pathology.
Advantages of CMR
 Unrestricted planes of view.
Unrestricted planes of view.
 Differentiation of tissue and fluid characteristics based on T1 and T2 characteristics.
Differentiation of tissue and fluid characteristics based on T1 and T2 characteristics.
 Functional cardiac imaging.
Functional cardiac imaging.
 Assessment of myocardium to investigate cardiomyopathic processes that may complicate differentiation of constrictive and restrictive physiology.
Assessment of myocardium to investigate cardiomyopathic processes that may complicate differentiation of constrictive and restrictive physiology.
 Wide field of view allowing study of related chest pathology or definition of extent of pericardial masses.
Wide field of view allowing study of related chest pathology or definition of extent of pericardial masses.
 Avoids ionizing radiation.
Avoids ionizing radiation.
Disadvantages of CMR
 Investigations are relatively time consuming.
Investigations are relatively time consuming.
What can CMR tell us?
 Pericardial surfaces are visible as a thin dark line on most CMR sequences (T1 and T2 weightings, steady state free precession (SSFP) imaging) surrounding the heart. It is dark on both T1
Pericardial surfaces are visible as a thin dark line on most CMR sequences (T1 and T2 weightings, steady state free precession (SSFP) imaging) surrounding the heart. It is dark on both T1
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree