10 Peripheral Nerve Imaging
Siegfried Peer and Werner Judmaier
Peripheral nerves are small structures, with a complex course along the extremities. They are often covered by thick layers of muscle and fatty tissue, which obscures them from direct access thus making them difficult to image. In addition, the most common pathologies–such as compression neuropathy at the carpal tunnel, for example–are clinically clearly defined and readily diagnosed entities. There is increasing demand for imaging and especially sonography of peripheral nerves. One of the reasons for this is that clinically similar neurologic findings may be caused by completely different pathologies structurally. For example, carpal tunnel syndrome, which may be idiopathic in nature, may also be caused by a space-occupying lesion in the carpal tunnel, such as ganglia, accessory muscle tissue, or vascular malformations, which may impinge on the median nerve. Various causes of carpal tunnel syndrome may cause quite similar neurologic symptoms and electrophysiologic studies may not reveal the underlying pathology. Imaging provides structural information of a nerve and its surroundings; this is important not only for diagnosis, but also for treatment planning. This is especially true for traumatic nerve lesions, where the definition of the exact site and extent of nerve involvement is crucial for the planning of surgical interventions; this directly affects the patient’s postoperative outcome. Another important reason for the revival of nerve imaging lies in the substantial improvement of imaging technology, especially in sonography and magnetic resonance imaging (MRI). This improvement–particularly in resolution–enables imaging of very small structures such that even tiny nerves in the finger may be visualized with sonography. This improved technology opens the field for the detailed study of intraneural structure, neural vasculature, and probably function.
 Clinical Indications
Clinical Indications
Common indications for peripheral nerve imaging may be categorized into three main areas: compression neuropathies, traumatic lesions, and tumors. These are the areas where sufficient expert knowledge based on clinical research in larger patient populations exists. There are attempts to image other nerve pathologies such as inflammatory conditions or systemic peripheral neuropathies, but despite some interesting reports in the literature, reliable data on the value of sonography for imaging of those conditions is currently lacking. Probably the most frequently imaged peripheral nerve pathology is compression neuropathy. The incidence of carpal tunnel syndrome, for example, is as high as 4% in the general population. The value of sonography for the diagnosis of compression neuropathy varies depending on the site of compression and the examination technique used. With high-resolution equipment, sonography can diagnose an idiopathic compression syndrome with high confidence and definitely define an extrinsic lesion with direct compromise of a nerve, such as compression by tumors, ganglia, accessory muscle, or functional impairment by dislocation of a nerve during movement. Another commonly imaged peripheral nerve pathology is trauma; the results of these imaging studies may substantially alter a patient’s therapeutic regime. For brachial plexus trauma and peripheral nerve injury in the extremities, ultrasound defines the location, extent, and severity of the lesion (i.e., if a lesion is complete or incomplete). Peripheral nerve tumors may be investigated with ultrasound based on the clinical suspicion of a lesion (i.e., a lesion with a positive Tinel sign or neurologic symptoms), but more often such a lesion is incidentally found during examination of an otherwise unclear soft tissue mass. A musculoskeletal sonographer should therefore be aware of the sonographic appearances of peripheral nerve tumors to have them included in the differential diagnosis.
 Technical Guidelines
Technical Guidelines
Equipment
Sonographic imaging relies on contrast and resolution. High-frequency transducers of up to 17 MHz result in an axial resolution of ~250 microns. High-frequency broadband linear arrays therefore are the state of the art for musculoskeletal and nerve imaging. High resolution, however, is not without problems; generally, improved resolution comes with a reduction in penetration. The choice of transducer for imaging of a specific nerve is therefore influenced by its location (Table 10.1).
Requirements for ultrasound scanner hard- and software warrant a short comment: while until recently only big and bulky top-notch ultrasound scanners had sufficient hardware power and software to enable imaging of tiny structures, this has recently changed. High-quality portable ultrasound systems, equipped with tissue harmonic imaging, image compounding, and various other artifact-reduction software similar to what we are used to apply on high-end scanners are becoming increasingly available. Combined with efficient high-frequency transducers, these small systems result in very high image quality, allow for bedside examination of peripheral nerves, and are now a valuable adjunct to the diagnostic toolbox of neurologists, orthopedists, and specialists in electrophysiology alike.
Table 10.1 Choice of Transducer Depending on Type of Nerve Examined and Clinical Question
| Transducer | Nerve | Clinical question |
|---|---|---|
| 3–9 MHz or similar | Sciatic nerve (proximal) | Trauma |
| 5–12 MHz or similar | Sciatic nerve (distal), brachial plexus, femoral nerve, radial/ulnar/median nerve | Trauma, tumor, compression neuropathy (cross sectional measurements), postoperative lesions (scar tissue compression), sonography guided interventions |
| 5–17 MHz or similar | Radial/ulnar/median/peroneal/tibial/ nerve | Compression neuropathy (structural analysis of nerve), trauma, neuritis, small tumors |
General Examination Technique
The general examination technique for sonography of peripheral nerves is similar to what we recommend for other musculoskeletal structures: findings are documented in two perpendicular planes and so on, but it differs especially in how a nerve and neural pathology are identified. It is desirable to scan a nerve in a short axis plane along its complete course along an extremity to search for suspected pathology. Sometimes (especially in traumatic lesions), it is more reliable to first identify the nerve at an area with distinct anatomic landmarks, where it may be easily found and then followed proximally or distally to the site of possible impairment. When scars or hematoma obscure direct access to a nerve at the level of impairment, the latter approach is more feasible.
The general appearance of a peripheral nerve on sonography is fairly uniform: on long axis sonograms the nerve is a longitudinal tubular structure with continuous hypoechoic elements (the axon bundles) interspersed and bordered by hyperechoic connective tissue (epi- and perineurium) (Fig. 10.1A). On short axis sonograms, a nerve shows a dotted appearance, like a cross-section of an electric cable, with quite regularly sized individual fascicular elements (Fig. 10.1B). The number of discernible fascicles and the amount of connective tissue may vary depending on the size of a nerve and its location in the body. Nerves that run along bony surfaces–especially in a curved fashion–or in osteofibrous tunnels, may undergo some normal amount of stretching and pressure and therefore show tighter packed fascicles with less echogenic elements. Nerves are mobile structures and are easily displaced during joint motion or even with light pressure of the transducer. The functional assessment of nerve motion may be an important sonographic technique to investigate impaction of a nerve under some tight ligament or in a postoperative scar.
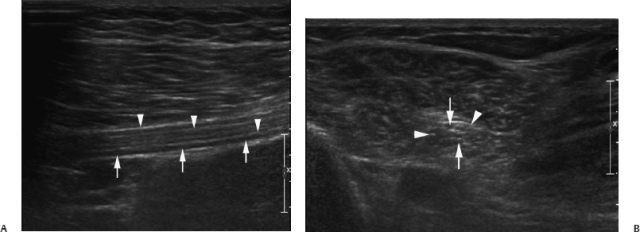
Fig. 10.1 (A) Long and (B) short axis sonogram of sciatic nerve in a volunteer. Continuous hypoechoic fascicular elements (arrows) interspersed and bordered by echoic epineurial tissue are seen (arrowheads).
 Normal Anatomy
Normal Anatomy
Peripheral nerves are small structures covered and surrounded by various elements of soft tissue (such as fat or muscle). This aspect, together with their peculiar anatomic course, combines to make nerves sometimes difficult to identify with sonography. In the following sections, we will focus on the topographic anatomy of the nerves that are more commonly imaged in routine clinical practice, providing details of their anatomic/sonographic and magnetic resonance imaging (MRI) correlation. Sonographic examination of other less commonly imaged nerves, their detailed anatomy, and description may be found elsewhere (see Suggested Readings); it is beyond the scope of this book, which is directed more toward the general sonographer.
The Cervical/Brachial Plexus
The cervical/brachial plexus is easiest identified in a transverse plane perpendicular and just slightly cranial to the clavicle. In this region, the plexus elements are seen surrounding the subclavian artery (Fig. 10.2A,B). If you slide your transducer upward along the plexus, you will easily reach the interscalene gap, where the plexus trunks are lined up one behind the other (Fig. 10.2C,D). From here it is easy to follow the individual root to its corresponding neural foramen (Fig. 10.2E,F).
For identification of an individual nerve root, the exact level of the neural foramen has to be determined, which can be achieved by two methods: either identify the transverse process of the sixth cervical vertebra searching for the entry of the vertebral artery into its foramen, or search for the transverse process with only a large posterior but no anterior tubercle, which is a distinct feature of the seventh cervical vertebra (Fig. 10.3).
The nerve root C5 to C7 is always accessible to sonography; however, the root C8 and TH1 may be obscured from direct access in patients with thick, short necks. The outlet of the neural foramen is best analyzed with oblique scanning in a coronal plane. This scan for example is best suited for the identification of an avulsed nerve root with pseudomeningocele (Fig. 10.4). The infraclavicular portion of the plexus may be assessed from an axillary approach with the patient’s arm abductedor elevated above the head. In slender individuals we may be able to assess the whole course of the plexus behind the clavicle with supra- and infraclavicular views, but often a short segment lying directly posterior to the clavicle is obscured from direct access.
The Cubital Tunnel
The cubital tunnel is an osteofibrous canal at the medial epicondyle of the humerus. It houses the ulnar nerve in its course to the forearm and is covered by a fibrous band called the cubital tunnel retinaculum also known as the Osborne fascia. The distal extension of this band connects the two heads of the flexor carpi ulnaris muscle and is called the arcuate ligament. Although you may identify the ulnar nerve on short axis views directly behind the tip of the medial epicondyle (Fig. 10.5) (the patient is best positioned with the lower arm in forced supination and slight elbow flexion with outward rotation of the upper arm), it is sometimes more feasible to identify it in the upper arm where it runs adjacent to the posterior margin of the biceps muscle. Hereafter, the nerve is continuously scanned distal until it exits the cubital tunnel. Normal diameters and cross-section areas of the nerve are documented in short axis views at the entry, in the middle (tip of the epicondyle), and exit of the tunnel and at any site of a sudden change in caliber. Normal values for cross-section areas range from 4 to 10 mm2. Note that the ulnar nerve is slightly enlarged in the middle section of the tunnel with a more hypoechoic appearance and less identifiable epineurial tissue in normal subjects. This is most probably due to its close contact with the bony bottom of the tunnel and some normal amount of constant stretching during elbow flexion/extension. Longitudinal scans should always be added, as they allow for easier identification of an abrupt change in nerve caliber (Fig. 10.6). Functional scanning with flexion/extension of the elbow is important to diagnose a snapping ulnaris/ snapping triceps syndrome, which is a rare, but important cause for ulnar neuropathy at the elbow.
The Carpal Tunnel
The median nerve inside the carpal tunnel is probably the most easily assessed peripheral nerve. Attempts to diagnose carpal tunnel syndrome with sonography date back to the early 1990s. The carpal tunnel holds the flexor tendons and the median nerve and is covered by the flexor retinaculum, sometimes also called the transverse carpal ligament. The retinaculum is readily identified on sonograms and MRIs alike as a small band-like structure traversing from its attachment at the pisiform bone to the scaphoid (Fig. 10.7).
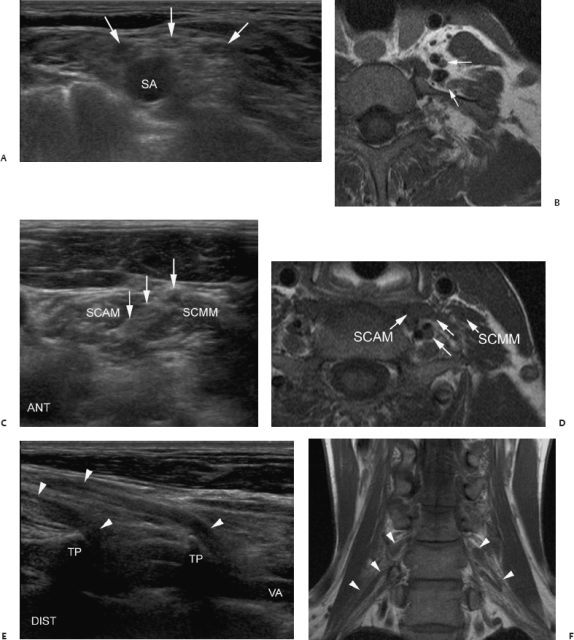
Fig. 10.2 (A–D) Sonography of normal brachial plexus with magnetic resonance imaging correlations. (A,B) Short axis, supraclavicular region: plexus fascicles surrounding subclavian artery (SA) (arrows). (C,D) Short axis, interscalene region: plexus trunks lined up inside interscalene gap (arrows). SCAM, scalenus anterior muscle; SCMM, scalenus medius muscle. (E,F) Long axis, root level: plexus roots (arrowheads). TP, transverse processes; VA, vertebral artery.
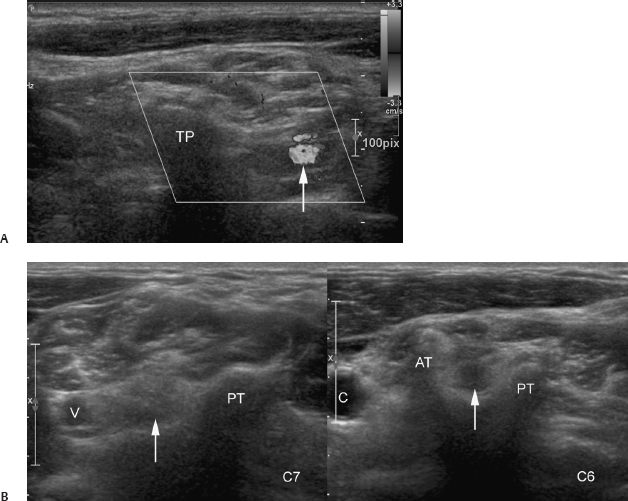
Fig. 10.3 Localization of nerve root in plexus sonography. (A) Oblique sonogram through transverse process (TP) of 6th cervical vertebra. The vertebral artery can be seen (arrow). (B) Short axis sonograms through transverse process of 7th and 6 th cervical vertebra. Note normal posterior tubercle (PT) in both vertebrae, absence of anterior tubercle (AT) in C7 and prominent anterior (AT) tubercle in C6. V, vertebral artery; C, carotid artery; arrows, C6/C7 nerve root.
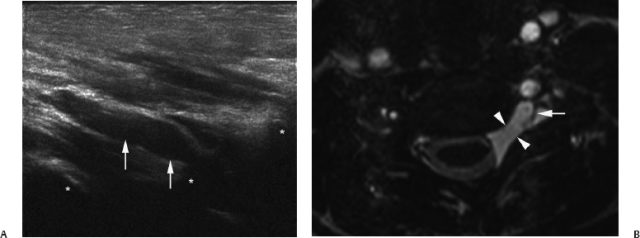
Fig. 10.4 (A) Long axis sonogram through paravertebral cervical plexus in a patient with root avulsion. Empty extraforaminal root sleeve (arrows) is demonstrated and the transverse processes can be seen (*). (B) Correlative axial T2-weighted magnetic resonance image confirms fluid-filled pseudomeningocele (arrowheads) and avulsed root fragment (arrow).
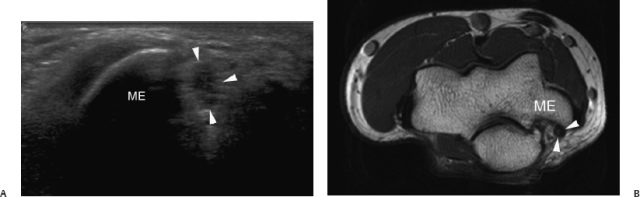
Fig. 10.5 Sonography of cubital tunnel (A) with magnetic resonance imaging correlation (B). Identification of ulnar nerve (arrowheads) behind the tip of the medial epicondyle (ME).
The median nerve normally runs through the carpal tunnel in a single stem, but may show a high bifurcation shortly proximal to its entrance into the carpal tunnel or at the forearm level. In ~25% of the latter cases it may be accompanied by an either perfused or obliterated persistent median artery (Fig. 10.8). The artery runs in between the two nerve bundles; it may either have a common envelope of outer connective tissue together with the two nerve stems, or the two nerve stems may be completely separated from each other and the interpositioned artery. A persistent median artery may also be found with a normal division of the median nerve, in which case it lies eccentric to the nerve.
The normal median nerve has a distinct echoic outer epineurium and consists of several individual fascicular bundles separated by inner epineurial tissue, which results in a honeycomb appearance on cross section. On long axis views we encounter the typical longitudinal tubular structure of a peripheral nerve. Note that the normal nerve slightly tapers toward the exit of the carpal tunnel (Fig. 10.9)–this must not be interpreted as a sign of carpal tunnel disease.
Data in the literature on normal values for median nerve diameters and cross-section areas vary, but in general the median nerve proximal to the flexor retinaculum has a crosssection of around 7 to 9 mm2. As there is a large interindividual variation in median nerve sizes, a forearm to wrist ratio has been introduced to reference median nerve size to a patient’s general body habitus and a ratio greater than 1.4 is considered abnormal.
The Popliteal Fossa
The popliteal fossa is an important region for the examination of the peripheral nervous system: it contains the division of the sciatic nerve into its main branches of the tibial and fibular nerves. It is the ideal site to localize the sciatic nerve and follow it back along its proximal course to the gluteal fold. Identification of the nerve at the posterior thigh level is often difficult, as the nerve is covered by the bulk of subcutaneous fat and muscles. The fossa is also ideal for identification of the common fibular nerve, which may then be followed along the tendon of the biceps femoris muscle on its course toward the fibular neck (Fig. 10.10) where it enters the peroneal tunnel. The common tibial nerve may be identified in the popliteal fossa as well (where it lies in-between the medial and lateral gastrocnemius muscle and directly adjacent to the deep popliteal vein) and followed along its distal course; however, it is easier to localize at its distal portion above the ankle. Although the sciatic nerve division is normally located in the popliteal fossa, a high division at a variable length above knee level may be encountered.
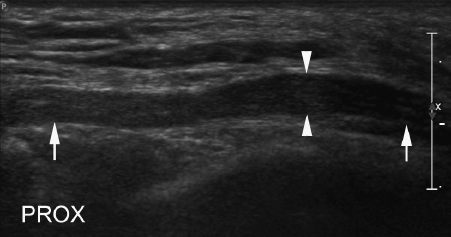
Fig. 10.6 Long axis view of ulnar nerve (arrows) in a patient with cubital tunnel syndrome. Note swelling with change of nerve diameter inside cubital tunnel (arrowheads).
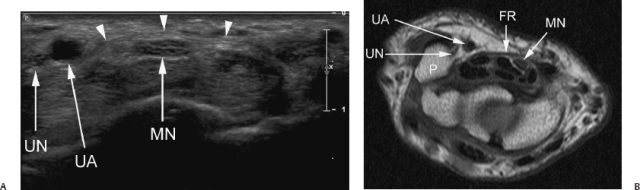
Fig. 10.7 (A) Short axis sonogram through carpal tunnel in healthy volunteer. The flexor retinaculum can be seen (arrowheads). (B) T1-weighted magnetic resonance image. MN, median nerve; UA, ulnar artery; UN, ulnar nerve; FR, flexor retinaculum (arrowheadsin A); P, pisiform bone.
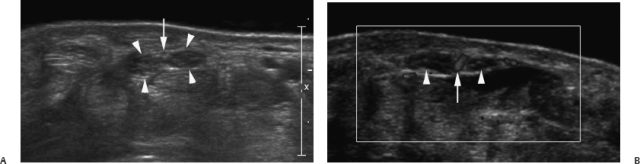
Fig. 10.8 (A) Short axis sonogram through median nerve with high division and obliterated median artery (arrow). Note that the nerve and artery share a common outer epineurial sheath (arrowheads). (B) Perfusion of median artery (arrow) is seen in another patient with high division of median nerve (arrowheads).
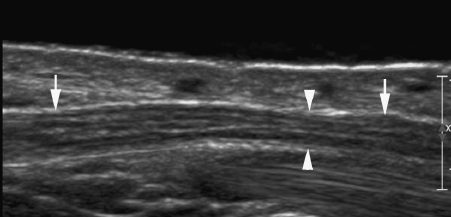
Fig. 10.9 Long axis view of normal median nerve (arrows) in a healthy volunteer. Note slight caliber reduction of median nerve inside carpal tunnel (arrowheads).
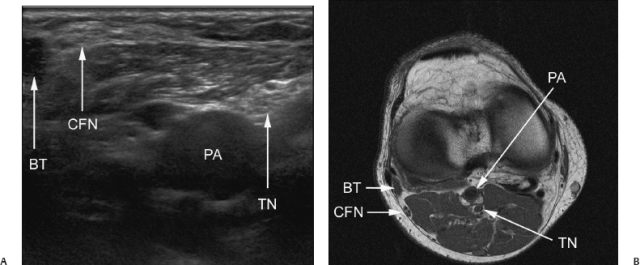
Fig. 10.10 (A) Transverse sonogram of popliteal fossa. (B) Correlative T1-weighted magnetic resonance image. PA, popliteal artery; BT, femoral biceps muscle tendon; TN, tibial nerve; CFN, common fibular nerve.
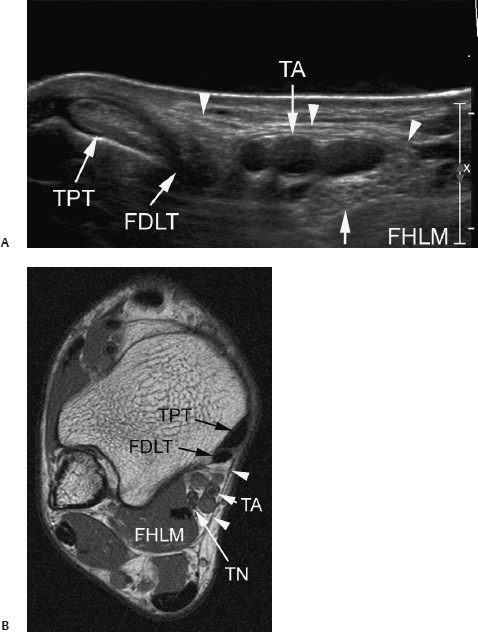
Fig. 10.11 (A) Transverse sonogram of tarsal tunnel and (B)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree





