PETROUS APEX MALIGNANT TUMORS
KEY POINTS
- Magnetic resonance imaging and computed tomography can very often suggest the proper diagnosis of a malignant tumor of the petrous apex, although differentiation of skull base osteomyelitis from malignancy can prove challenging.
- Primary malignancies of the petrous apex are very uncommon.
- The majority of malignant disease involving the petrous apex is due to secondary spread of cancer.
- Imaging is essential in initial diagnosis and treatment planning and sometimes following surveillance strategies depending on the origin and extent of disease and the approach to treatment.
INTRODUCTION
Etiology
Malignant tumors arising primarily from the petrous apex aside from a chondrosarcoma (Chapter 125) are extremely rare. Secondary involvement is relatively common and most typically from nasopharyngeal carcinoma. Other secondary petrous apex malignancy is usually part of more generalized skull base malignant tumor involvement due to metastatic disease or lymphoma, leukemia, and plasma cell dyscrasias. Isolated petrous apex metastatic disease as an expression of systemic malignancy, however, is very uncommon. Chondrosarcoma, the most common of these relatively uncommon cancers that arise in the petrous apex, is discussed in general in Chapter 39 and more specifically as related to the benign and malignant lesions that affect the petrous apex in Chapter 125. Mesenchymal- and osseous-origin lesions such as Ewing sarcoma, rhabdomyosarcoma, and meningeal sarcoma are rarely limited to the petrous apex and are histologically difficult to anticipate precisely prior to tissue sampling. The rare tumor most likely to be properly anticipated histologically is the endolymphatic sac carcinoma known to occur both sporadically and in combination with von Hippel-Lindau syndrome (Fig. 126.1); it has a fairly characteristic imaging morphology and anatomic site of origin.
Petrous apex malignancies must be differentiated from a relatively short list of mucosal, congenital, vascular, and benign tumors that affect this part of the posterolateral portion of the central skull base. The most common of the benign tumors are meningiomas and nerve sheath tumors discussed in Chapter 124. Chordomas (Chapters 34 and 125) and paragangliomas (Chapter 33) are discussed separately. Other benign tumors are rare and include mesenchymal- and osseous-origin lesions such as fibromyxomas and osteochondromas and even pituitary tumors discussed in Chapters 32 and 35 through 40.
Prevalence and Epidemiology
These are mainly sporadic tumors usually with no known predisposing conditions except when there are known systemic malignancies that might lead to secondary involvement. As another example, there is the well-documented association of endolymphatic sac carcinoma with Von Hippel-Lindau syndrome. Metastatic disease to the temporal bone is most frequently located at the petrous apex and is most commonly seen in adenocarcinomas.1
Clinical Presentation
Facial, periorbital, and periocular pain or other mainly trigeminal nerve–related dysfunction occurs when the mass involves the mesial aspect of the petrous apex at its interface with entrance of the trigeminal nerve to its cistern. Dural involvement can produce localized headaches that may cause otalgia and/or headaches that are retro-orbital or referred to the skull vertex similar to the pattern of sphenoid sinus referred pain patterns.
A mass situated more laterally that involves the internal auditory canal or at the geniculate ganglion region may result in facial paralysis. Hearing loss may be conductive due to eustachian tube obstruction. Sensorineural hearing loss, vertigo, and/or tinnitus may be due to cochleovestibular nerve or direct inner ear involvement. Cranial nerve deficits tend to be grouped as VII through XII and II through VI depending on the site of origin and extent of the mass, although the deficits are typically of only one or two nerves at the time of presentation—most commonly, cranial nerves V and VI. Carotid artery occlusion can lead to signs and symptoms of ischemia.
PATHOPHYSIOLOGY
Anatomy
The anatomy of interest is that of the petrous apex (Figs. 104.15–104.17) described in detail in Chapter 104 (Fig. 104.48). It is also useful to understand the relationship of cranial nerves V and VI to the petroclival fissure region and the petrous segment of the carotid canal (Fig. 112.2). Collateral knowledge about the entire temporal bone and related cranial nerves is also a general requisite for interpreting studies of patients with petrous apex masses.
Pathology and Patterns of Disease
The appearance, patterns of growth, and pathophysiology of tumor growth in general is discussed in Chapter 21; those of metastatic disease are discussed more specifically in Chapter 42.
The masses may occasionally arise primarily and exclusively in the petrous apex due to hematogenous spread by the slow blood flow through the petrous apex marrow. More characteristically, the petrous apex will be secondarily involved from spread from the adjacent sphenoid wing or base of the sphenoid bone, with the tumors often spreading across the petroclival fissure. The disease process of origin may be one arising in the marrow space (Fig. 126.2) or one spreading from the nasopharynx along the attachments of the pharyngeal muscles to the undersurface of the temporal bone (Chapter 188). Secondary involvement of the petrous bone may also result from leptomeningeal extension of intra- or extracranial neoplasms.2
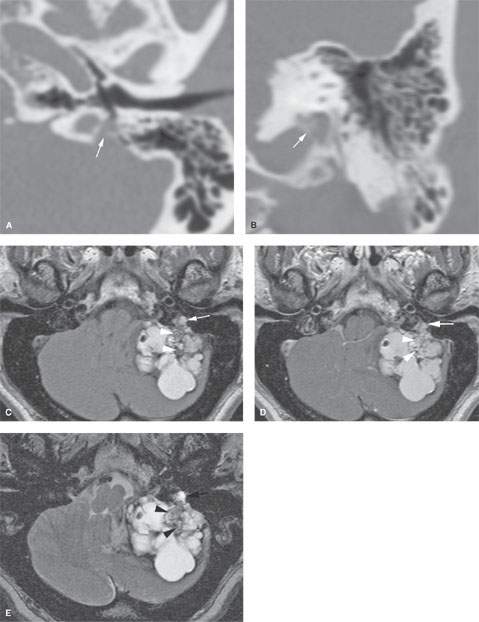
FIGURE 126.1. A patient with endolymphatic sac carcinoma. A, B: Computed tomography shows focal bone erosion where the tumor is pedicled (arrows) to the petrous apex at the endolymphatic sac–duct junction. C–E: There is a multicystic mass occupying the cerebellopontine angle. In (D), the non–contrast-enhanced T1-weighted (T1W) image shows the multiple cysts filled with highly proteinaceous fluid, so the contents are bright. In (D), the T2-weighted images show the multiple cysts filled with highly proteinaceous fluid; the contents are bright here as well. In (E), enhancement in this T1-weighted image with contrast is most obvious in the lower signal component (arrowheads in all images) that is pedicled to the region of the endolymphatic sac and canal.
Malignancies may invade or compress cranial nerves V, VI, VII, and VIII when they are more superior in origin and cranial nerves IX and XII when somewhat more inferior in origin or extent. The tumors may encase or invade major vessels including the dural sinuses, carotid artery, and jugular vein. Involvement of these transiting structures is typically associated with frank erosion of the internal auditory canal, carotid canal, and jugular fossa. The bony labyrinth may eventually be involved.
Pathologically Altered Function
There may be no deficits early in the pathogenesis of these chronically progressive tumors. At some point, the bony eustachian tube may be compressed with resulting eustachian tube dysfunction or otitis with effusions. Eventually, the tumors will cause cranial neuropathies and inner ear dysfunction.
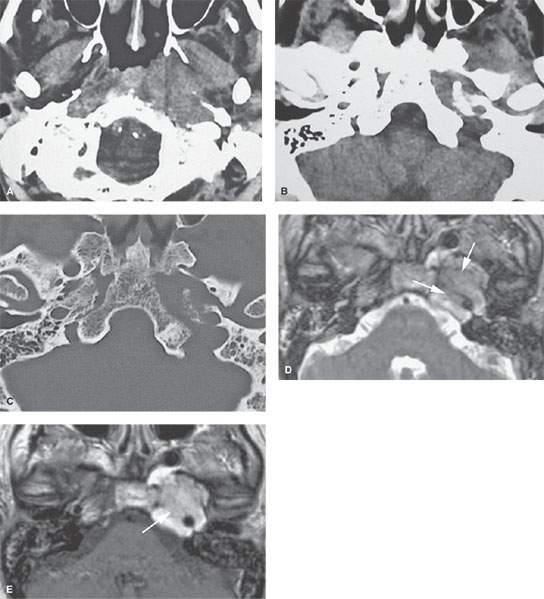
FIGURE 126.2. Two patients with plasmacytomas involving the petrous apex. A–C: Patient 1. Extramedullary plasmacytomas or the carotid petrous canal with invasion of the skull base and petrous apex. Computed tomography in soft tissue (A, B) and bone window (C) shows a submucosal nasopharyngeal and parapharyngeal mass on the left that erodes the petrous apex. D, E: Magnetic resonance of Patient 2 with plasmacytoma of the petrous apex. In (D), the T2-weighted image shows a mass (arrows) with signal intensity about equivalent to brain, suggesting high cellularity. In (E), the contrast-enhanced T1-weighted images shows diffuse and somewhat inhomogeneous enhancement.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








