Pharynx and Esophagus
Sara Moshiri
William E. Brant
Imaging Methods
The upper gastrointestinal (UGI) series, also called a barium meal, is a barium examination of the alimentary tract from the pharynx to the ligament of Treitz. A barium swallow or esophagram is a study more dedicated to evaluation of swallowing disorders and suspected lesions of the pharynx and the esophagus. Barium sulfate preparations are ingested orally, and filming is performed during fluoroscopy. The fluoroscopic examination is commonly videotaped or digitally stored to allow for more detailed review of swallowing dynamics and motility. Double-contrast techniques using mucosal coating with barium combined with luminal distension are preferred for mucosal detail. Distension of the pharynx is provided by having the patient phonate. Distension of the esophagus is attained by having the patient ingest gas-producing crystals. Full-column, or single-contrast, technique uses barium suspension alone to fill and distend the esophagus. Mucosal relief views are collapsed views of the barium-coated esophagus.
Cross-sectional imaging techniques are used to stage malignancies of the pharynx and esophagus and to clarify findings seen with other imaging methods (1). CT complements barium studies and endoscopy of the esophagus by demonstrating the esophageal wall and adjacent structures to determine extent of disease (2). CT is poor at evaluating the mucosa and generally cannot differentiate inflammatory and neoplastic conditions. MR is preferred over CT for evaluation of the nasopharynx and is an alternative to CT for demonstrating the extent of esophageal disease. The clear depiction of blood vessels by MR is useful in confirming the presence of varices and in evaluating mediastinal vascular anatomy. Endoscopic sonography is useful for demonstration of tumor penetration of the esophageal wall.
This chapter reviews the pharynx as studied as part of a barium examination and for assessment of swallowing disorders. Cross-sectional imaging of the neck and pharynx is reviewed in Chapter 9.
Anatomy
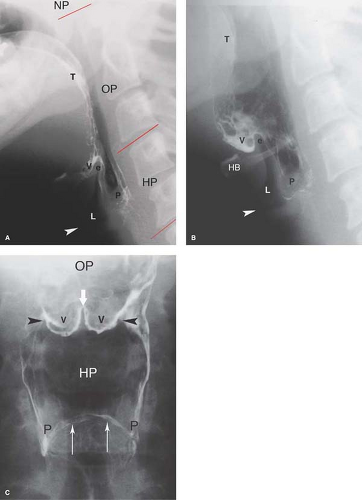
The pharynx extends from the nasal cavity to the larynx and is arbitrarily divided into three compartments (Fig. 28.1). The nasopharynx extends from the skull base to the soft palate. Its function is entirely respiratory, and the nasopharynx is not considered further in this chapter. The oropharynx is posterior to the oral cavity and extends from the soft palate to the hyoid bone. The hypopharynx (laryngopharynx) extends from the hyoid bone to the cricopharyngeus muscle. The base of the tongue forms the anterior boundary of the oropharynx. The outline of the surface of the tongue is nodular because of the presence of lymphoid tissue forming the lingual tonsils and the circumvallate papillae, which contain taste buds. The lingual tonsils may hypertrophy and mimic a neoplasm. The epiglottis and aryepiglottic folds separate the larynx from the oropharynx and the hypopharynx. The valleculae are two symmetrical pouches formed in the recess between the base of the tongue and the epiglottis. They are divided medially by the median glossoepiglottic fold and bounded laterally by the lateral glossoepiglottic folds. The piriform sinuses are deep, symmetrical, lateral recesses formed by the protrusion of the larynx into the hypopharynx.
The esophagus extends from the cricopharyngeus muscle at the level of C5–6 to the gastroesophageal junction (GEJ). The esophagus is a muscular tube formed by an outer longitudinal muscle layer and an inner circular muscle layer lined by stratified squamous epithelium. The esophagus lacks a serosal layer, which allows the rapid spread of tumor into adjacent tissues. The proximal one-third of the esophagus is predominantly striated muscle, whereas the distal two-thirds, below the level of the aortic arch, is predominantly smooth muscle. Normal extrinsic impressions on the esophagus are made by the aortic arch, the left mainstem bronchus, and the left atrium. The normal esophageal mucosa is smooth and featureless when fully distended on air–contrast barium studies (3). With partial collapse, multiple longitudinal folds, 1 to 2 mm in thickness, become evident. Multiple regular, transverse folds, 1-mm thick, result from contraction of the longitudinal fibers in the muscularis mucosa. This pattern is called feline esophagus because it is typical of a normal esophagus in cats. In humans, it may be an early sign of dysmotility or esophagitis (see Fig. 28.21).
On cross-sectional imaging, the esophagus appears as an oval of soft tissue density usually surrounded by fat. In most cases (>60%), the esophagus is collapsed and contains no air (2). Normal air or contrast within the lumen of the esophagus is located centrally within its lumen. Eccentric contrast or air should be considered abnormal. Distension of the upper
esophagus more than 10 mm or the lower esophagus more than 20 mm is abnormal (2). Air–fluid levels in the esophagus are always abnormal. The lower esophageal sphincter (LES) is normally closed. The wall of the distended esophagus should not exceed 3 mm in thickness.
esophagus more than 10 mm or the lower esophagus more than 20 mm is abnormal (2). Air–fluid levels in the esophagus are always abnormal. The lower esophageal sphincter (LES) is normally closed. The wall of the distended esophagus should not exceed 3 mm in thickness.
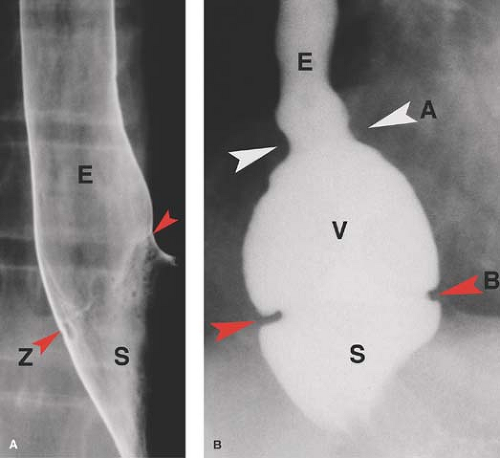
Anatomy of the esophagogastric region is complex (4) (Fig. 28.2). The length of the esophagus is tubular, and its termination is saccular. The saccular termination is called the esophageal vestibule. The tubulovestibular junction is formed by a symmetrical muscular ring called the A ring. The B ring is an
asymmetrical mucosal ring or notch that occurs at the junction of esophageal squamous epithelium with gastric columnar epithelium. This squamocolumnar junction is also marked by the Z line, a thin ragged line of demarcation seen on double-contrast views of the lower esophagus. The B ring and the Z line are considered to be radiographic markers of the GEJ. The LES is a physiologic rather than an anatomic structure. It is a 2- to 4-cm-long high-pressure zone located in the esophageal vestibule. It is defined manometrically but is without a distinct anatomic correlate. At rest, the LES is tightly closed with a pressure higher than gastric pressure to prevent reflux of gastric contents into the esophagus. Malfunction of the LES results in gastroesophageal reflux disease (GERD). The act of swallowing generates peristalsis in the esophagus, which results in relaxation of the LES allowing passage of swallowed liquids and solids into the stomach (4).
asymmetrical mucosal ring or notch that occurs at the junction of esophageal squamous epithelium with gastric columnar epithelium. This squamocolumnar junction is also marked by the Z line, a thin ragged line of demarcation seen on double-contrast views of the lower esophagus. The B ring and the Z line are considered to be radiographic markers of the GEJ. The LES is a physiologic rather than an anatomic structure. It is a 2- to 4-cm-long high-pressure zone located in the esophageal vestibule. It is defined manometrically but is without a distinct anatomic correlate. At rest, the LES is tightly closed with a pressure higher than gastric pressure to prevent reflux of gastric contents into the esophagus. Malfunction of the LES results in gastroesophageal reflux disease (GERD). The act of swallowing generates peristalsis in the esophagus, which results in relaxation of the LES allowing passage of swallowed liquids and solids into the stomach (4).
The esophageal hiatus is an angled opening in the diaphragm, formed by the edges of the diaphragmatic crura. On CT and MR, the crura appear as often prominent, teardrop-shaped structures of muscle density. With normal breathing, the proximal vestibule and A ring lie in the thorax. The midvestibule is in the esophageal hiatus, and the distal vestibule and B ring are in the abdomen. With swallowing, the vestibule opens and moves upward, and the B ring may be seen 1 cm above the diaphragm.
Normal Swallowing and Motility
The normal process of swallowing can be divided into oral, pharyngeal, and esophageal phases. The oral stage involves the voluntary transport of a bolus from the oral cavity into the pharynx. The soft palate elevates and the tongue depresses to accommodate the bolus and channel it into the oropharynx. The oropharynx and the hypopharynx receive the bolus and conduct it to the esophagus. Breathing is halted while the larynx elevates, the laryngeal vestibule closes, and the epiglottis and aryepiglottic folds close over the opening into the larynx and deflect the bolus through the lateral piriform recesses.
The functional upper esophageal sphincter (UES), formed by the cricopharyngeus and other pharyngeal muscles, opens to receive the bolus. Peristalsis conveys ingested material through the tubular esophagus to the stomach. Primary peristalsis is composed of a rapid wave of inhibition that opens the sphincters, followed by a slow wave of contraction that moves the bolus. Normal peristalsis will clear the esophagus completely with each swallow. Radiographically, primary peristalsis appears as a stripping wave that traverses the entire esophagus from top to bottom. Secondary peristalsis is initiated by distension of the esophageal lumen. The peristaltic wave starts in the midesophagus and spreads simultaneously up and down the esophagus to clear reflux or any part of a bolus left behind. Secondary waves have the same radiographic appearance as primary waves except that they start at the point of the retained barium bolus. Tertiary waves are nonproductive contractions associated with motility disorders. Irregular contractions follow one another at close intervals from the top to the bottom of the esophagus. These nonperistaltic contractions cause a corkscrew or beaded appearance of the esophageal barium column. The functional LES at the level of the esophageal vestibule relaxes and opens in response to swallowing, primary peristalsis, and proximal esophageal dilation.
Oral and pharyngeal swallowing are evaluated fluoroscopically with the patient in an upright position simulating normal eating. The lateral projection is most useful. Studies are videotaped or digitally stored for subsequent detailed study. Esophageal motility is evaluated by observing fluoroscopically
at least five separate swallows of barium with the patient in a prone oblique position. The patient must be instructed to swallow only once, as continuous swallowing distends the esophagus and makes the evaluation of primary peristalsis impossible.
at least five separate swallows of barium with the patient in a prone oblique position. The patient must be instructed to swallow only once, as continuous swallowing distends the esophagus and makes the evaluation of primary peristalsis impossible.
Motility Disorders
Difficulty with swallowing has an increasingly high prevalence with age. Symptoms of abnormal oral or pharyngeal swallowing include difficulty initiating swallowing, globus sensation (lump in throat), cervical dysphagia, nasal regurgitation, hoarseness, coughing, or choking. Symptoms suggesting esophageal dysfunction include heartburn, dysphagia, “indigestion,” and chest pain. Dysphagia is defined as the awareness of swallowing difficulty during the passage of solids or liquids from mouth to stomach. Patients complain of food “sticking in the throat” and of painful swallowing (odynophagia). These symptoms may be caused by anatomic abnormalities, tumors, or motility disorders. The patient’s subjective assessment of the location of the abnormality is not reliable. Detailed dynamic barium studies of the entire oropharyngeal–esophageal pathway with videofluoroscopy are needed for complete evaluation. Motility disorders that may cause dysphagia or aspiration are reviewed in this section. Radiographic findings of functional abnormalities of the pharynx and the esophagus increase in prevalence with age, may not correlate with specific symptoms, and must be interpreted with caution.
Signs of Pharyngeal Dysfunction. Pharyngeal stasis, indicative of impaired pharyngeal transport, is seen as increased residual volume of swallowed material filling the valleculae and piriform sinuses (5). Laryngeal penetration is defined as entry of barium into the laryngeal vestibule without passage below the vocal cords. Aspiration implies barium passage below the vocal cords (Fig. 28.3). Any of these findings may precipitate a cough. Laryngeal penetration and tracheobronchial aspiration are associated with increased risk of developing pneumonia especially in hospitalized patients. Nasal regurgitation occurs when the soft palate does not make a good seal against the posterior pharyngeal wall. Causes include neurologic impairment, muscular dystrophies, and structural defects in the palate. The major causes of pharyngeal dysfunction are listed in Table 28.1.
Table 28.1 Causes of Pharyngeal Swallowing Dysfunction | |||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Cricopharyngeal achalasia is attributable to failure of complete relaxation of the UES, commonly resulting in dysphagia and aspiration. Barium swallow demonstrates a shelf-like impression (cricopharyngeal bar) on the barium column at the pharyngoesophageal junction at the level of C5–6. The pharynx is distended, and barium may overflow into the larynx and trachea. Because some normal individuals have a prominent cricopharyngeal impression, controversy exists as to how prominent the impression must be to be considered significant. Narrowing of the lumen greater than 50% is generally accepted as a definite cause of dysphagia. Cricopharyngeal dysfunction is commonly associated with neuromuscular disorders of the pharynx.
Achalasia of the esophagus is a disease of unknown etiology characterized by (1) absence of peristalsis in the body of the esophagus, (2) marked increase in resting pressure of the LES, and (3) failure of the LES to relax with swallowing
(4). The abnormal peristalsis and LES spasm result in a failure of the esophagus to empty. Pathologically, cases show a deficiency of ganglion cells in the myenteric plexus (Auerbach plexus) throughout the esophagus. The clinical presentation is insidious, usually at age 30 to 50 years, with dysphagia, regurgitation, foul breath, and aspiration. Radiographic signs include (1) uniform dilatation of the esophagus, usually with an air–fluid level present; (2) absence of peristalsis, with tertiary waves common in the early stages of the disease; (3) tapered “beak” deformity at the LES because of failure of relaxation (Fig. 28.4); (4) findings of esophagitis including ulceration; and (5) increased incidence of epiphrenic diverticula and esophageal carcinoma. Treatment of achalasia is balloon dilation or Heller myotomy. Diseases that may mimic esophageal achalasia include the following.
(4). The abnormal peristalsis and LES spasm result in a failure of the esophagus to empty. Pathologically, cases show a deficiency of ganglion cells in the myenteric plexus (Auerbach plexus) throughout the esophagus. The clinical presentation is insidious, usually at age 30 to 50 years, with dysphagia, regurgitation, foul breath, and aspiration. Radiographic signs include (1) uniform dilatation of the esophagus, usually with an air–fluid level present; (2) absence of peristalsis, with tertiary waves common in the early stages of the disease; (3) tapered “beak” deformity at the LES because of failure of relaxation (Fig. 28.4); (4) findings of esophagitis including ulceration; and (5) increased incidence of epiphrenic diverticula and esophageal carcinoma. Treatment of achalasia is balloon dilation or Heller myotomy. Diseases that may mimic esophageal achalasia include the following.
Chagas disease is caused by the destruction of ganglion cells of the esophagus due to a neurotoxin released by the protozoa, Trypanosoma cruzi, endemic to South America, especially eastern Brazil. The radiographic appearance of the esophagus is identical to achalasia. Associated abnormalities include cardiomyopathy, megaduodenum, megaureter, and megacolon.
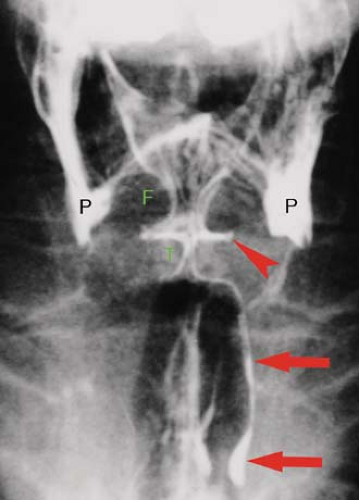
Carcinoma of the GEJ may mimic achalasia but tends to involve a longer (>3.5 cm) segment of the distal esophagus, is rigid, and tends to show more irregular tapering of the distal esophagus and mass effect (Fig. 28.5). When findings of achalasia are present on barium studies, it is important to evaluate the gastric cardia and fundus to rule out an underlying malignant tumor at the GEJ as the cause of these findings. The cardia and fundus is however not adequately evaluated radiographically in all patients because of delayed emptying of barium from the esophagus. Therefore, it is important to be aware of the limitations of barium studies in evaluating the cardia and fundus in patients with suspected achalasia (6).
Peptic strictures are usually associated with normal primary peristalsis. A hiatal hernia is usually present.
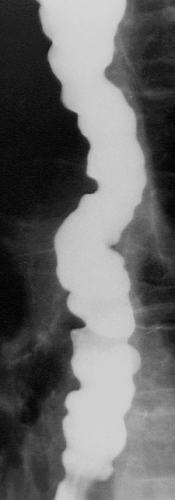
Diffuse esophageal spasm is a syndrome of unknown cause characterized by multiple tertiary esophageal contractions (Fig. 28.6), thickened esophageal wall, and intermittent dysphagia and chest pain. Primary peristalsis is usually present, but the contractions are infrequent. Most patients are middle-aged. The LES is frequently dysfunctional and the condition commonly improves with injection of Clostridium botulinum toxin at the GEJ or with endoscopic balloon dilatation of the LES. Diffuse esophageal spasm is characterized on barium studies by intermittently absent or weakened primary esophageal peristalsis with simultaneous, nonperistaltic contractions that compartmentalize the esophagus, producing a classic corkscrew appearance. CT reveals circumferential thickening (5 to 15 mm) of the wall of the distal 5 cm of the esophagus in 20% of patients (7).
Neuromuscular disorders are a common cause of abnormalities of the oral, pharyngeal, or esophageal phases of swallowing. The most common cause of neurologic dysfunction is cerebrovascular disease and stroke. Additional causes include Parkinsonism, Alzheimer disease, multiple sclerosis, neoplasms of the CNS, and posttraumatic CNS injury. Diseases of striated muscle, such as muscular dystrophy, myasthenia gravis, and dermatomyositis, predominantly affect the pharynx and proximal third (striated muscle portion) of the esophagus.
Scleroderma is a systemic disease of unknown cause characterized by progressive atrophy of smooth muscle and progressive fibrosis of affected tissues. Women are most commonly affected, usually aged 20 to 40 years at the onset of disease. The esophagus is affected in 75% to 80% of patients. Radiographic findings (Fig. 28.7) include (1) weak to absent peristalsis in the distal two-thirds (smooth muscle portion) of the esophagus; (2) delayed esophageal emptying; (3) a stiff dilated esophagus that does not collapse with emptying; and (4) wide gaping LES with free gastroesophageal reflux. Despite free reflux, tight strictures of the distal esophagus are uncommon.
Postoperative states, including surgery for malignancy of the tongue, larynx, and pharynx, commonly impair swallowing function as well as alter the morphology. Surgical resection is aimed at providing at least a 1-cm margin free of tumor and often results in removing large blocks of tissue and functionally altering the structures that remain.
Esophagitis frequently results in abnormal esophageal motility and visualization of tertiary esophageal contractions.
Gastroesophageal reflux disease (GERD) is a major health problem in the United States. GERD occurs as a result of incompetence of the LES. The resting pressure of the LES is abnormally decreased and fails to increase with raised intra-abdominal pressure. As a result, increases in intra-abdominal pressure exceed LES pressure, and gastric contents are allowed to reflux into the esophagus. GERD is classified as a spectrum of conditions: nonerosive reflux disease, erosive esophagitis, and Barrett esophagus. Symptoms of GERD include substernal burning pain (“heartburn”), postural regurgitation (in supine position), and development of reflux esophagitis, dysphagia, and odynophagia. Complications of GERD include reflux esophagitis, stricture, and development of Barrett esophagus. The radiographic diagnosis of GERD may be difficult because 20% of normal individuals show spontaneous reflux on UGI examination, and patients with pathologic GERD may not demonstrate reflux without provocative tests. Findings associated with GERD on barium esophagrams include (1) hiatal hernia, associated with presence of reflux esophagitis; (2) shortening of the esophagus, a finding of importance to treating GERD surgically; (3) impaired esophageal motility; (4) gastroesophageal reflux, often demonstrated by provocative maneuvers such as Valsalva, leg raising, and cough; and (5) prolonged clearance time of refluxed gastric contents. Low volume reflux that clears rapidly is not considered a significant finding (8). Monitoring of esophageal pH for 24 hours in an ambulatory patient is the most sensitive means of diagnosing abnormal GERD. GERD is managed medically with agents that inhibit gastric acid production or surgically with fundoplication.
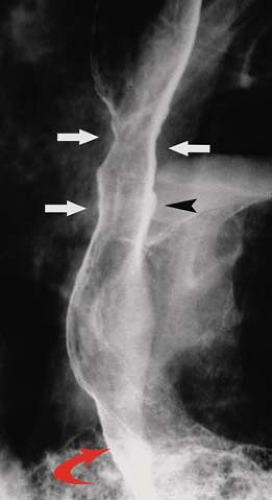 Figure 28.7. Scleroderma. Double-contrast esophagram in a patient with scleroderma demonstrates a stiff esophagus with peristalsis. The gastroesophageal junction (curved arrow) is gaping and free gastroesophageal reflux was observed. Reflux esophagitis has resulted in mild stricturing (white arrows) of the esophagus and focal ulcers (black arrowhead).
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|