Fig. 28.1
Metabolic pathway of 5-ALA
Fig. 28.2
Fluorescence spectrum of PpIX excited with 405 nm
Figure 28.3 shows fluorescence images of various colorectal cancer cell lines (HT-29, CACO-2, DLD-1, and HCT-15) and isolated normal LN cells [19]. Primary-culture normal LN cells were negative for 5-ALA-derived PpIX fluorescence at 1 and 3 h; in contrast, all colorectal cancer cell lines tested were positive after the start of incubation. Speckled PpIX-fluorescence signal was detected in the cytoplasm of the colorectal cancer cells.
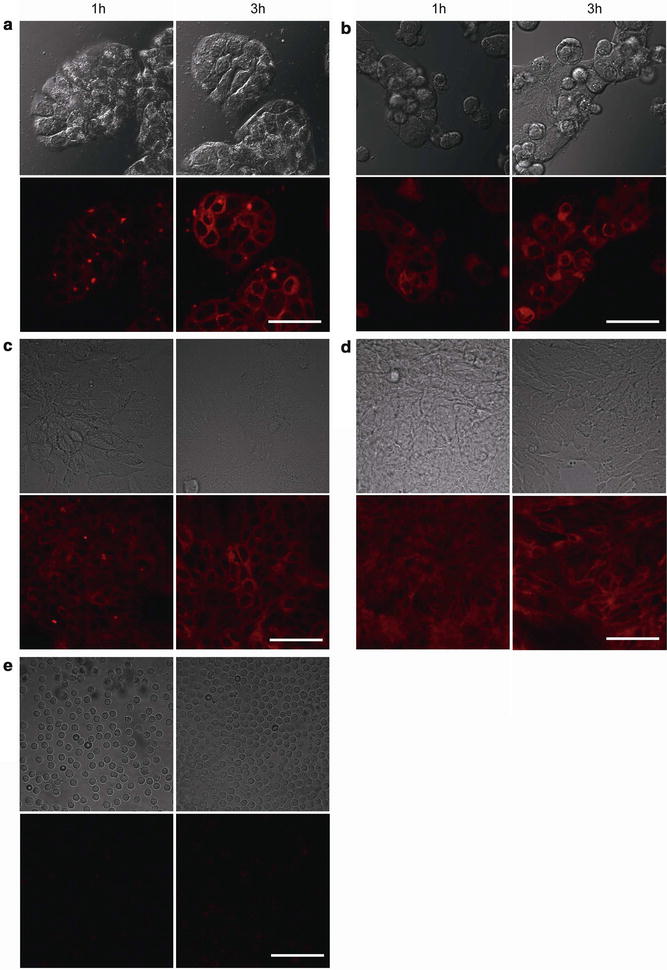
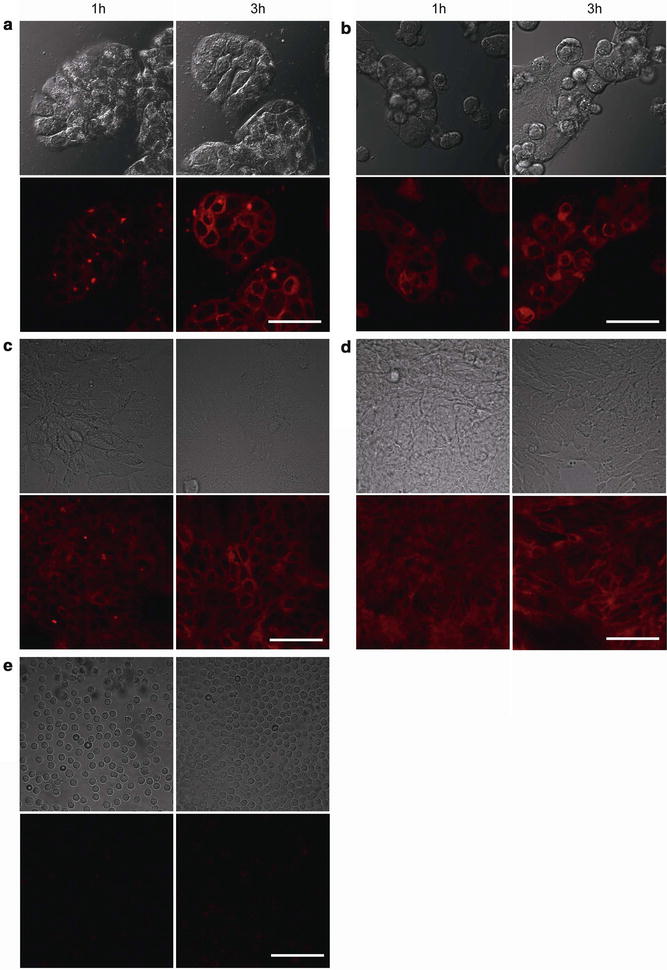
Fig. 28.3
Fluorescence detection of cancer cells by using 5-ALA administration. (a) HT-29, (b) CACO-2, (c) DLD-1, and (d) HCT-15 colorectal cancer cells and (e) isolated normal LN cells (e) were incubated with 15 mM 5-ALA for 30 min. With permission from Murayama Y, Harada Y, Imaizumi K, Dai P, Nakano K, Okamoto K, et al. Precise detection of lymph node metastases in mouse rectal cancer by using 5-aminolevulinic acid. Int J Cancer 2009;15;125(10):2256–63. © 2009 John Wiley and Sons [19]
Since the exogenous administration of the 5-ALA has few side effects in patients without metabolic disease of heme synthesis, such as porphyria, 5-ALA has been widely applied clinically for the detection of primary malignant tumors such as brain tumor, urinary bladder tumor, and gastrointestinal tumor [20–25]. Recently, several studies revealed that exogenous 5-ALA also accumulates in metastatic cancer cells at LNs to an extent sufficient to allow fluorescence detection of PpIX [19, 26–30]. Regarding its application to gastrointestinal cancer, the feasibility of PpIX-based fluorescence detection of LN metastasis was initially investigated by using a mouse model bearing rectal cancer [19], and the first clinical application to patients with gastrointestinal cancer was conducted in gastric cancer patients [27].
Fluorescence Detection of LN Metastasis Using 5-ALA in Xenograft Mouse Model of Gastrointestinal Cancer
The feasibility of fluorescence-based diagnosis of LN metastasis using 5-ALA has been preliminarily evaluated by using a xenograft mouse model of gastrointestinal cancer [19]. Figure 28.4 shows images from a feasibility study of the fluorescence diagnosis of LN metastasis carried out with an orthotopic mouse model of human rectal cancer [19]. This model develops LN metastases, around the abdominal aorta, from the aortic bifurcation to the renal arteries, 5 weeks after the inoculation of the rectal tumor [31].
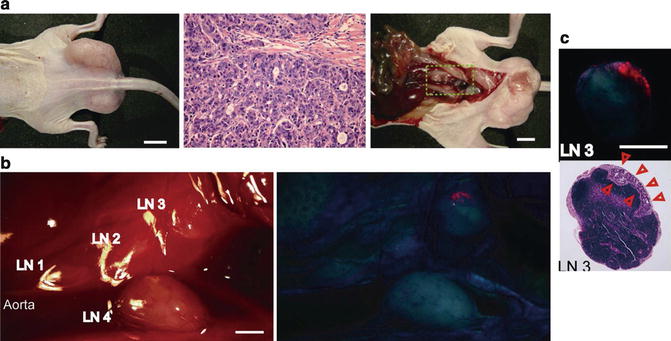
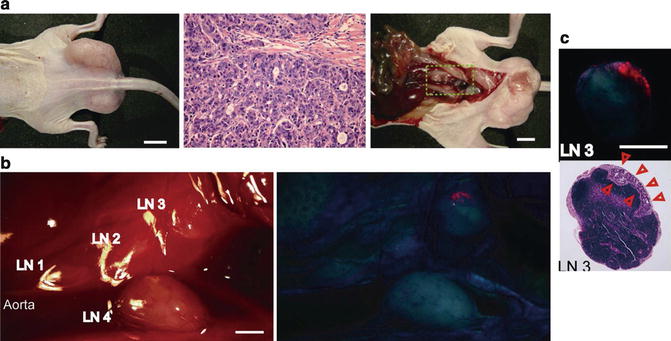
Fig. 28.4
Feasibility study of the fluorescence diagnosis of LN metastasis conducted with an orthotopic mouse model of human rectal cancer. (a) White-light image of a BALB/c nude mouse after the injection of human rectal cancer (HT-29) (left), image of HE-stained specimen of primary tumor (center), and white-light image of abdominal cavity of the nude mouse (right). (b) PpIX-fluorescence diagnosis of LN metastasis. White-light image of LNs (left) and fluorescence image of PpIX (right). (c) Fluorescence image and image of HE-stained specimen of excised LN3. With permission from Murayama Y, Harada Y, Imaizumi K, Dai P, Nakano K, Okamoto K, et al. Precise detection of lymph node metastases in mouse rectal cancer by using 5-aminolevulinic acid. Int J Cancer 2009;15;125(10):2256–63. © 2009 John Wiley and Sons [19]
After injection of 5-ALA via the tail vein, 5-ALA-derived PpIX fluorescence could be detected, as shown in Fig. 28.4b. The PpIX-fluorescence-positive region coincided with metastatic lesions. In contrast, PpIX-fluorescence-negative LNs contained no metastatic lesion. In this model, sufficient PpIX fluorescence was observed from 6 to 9 h after the 5-ALA injection. In general, the presence of metastasis in LNs is often identified based on the shape and hardness of the LNs, i.e., the metastatic LNs are generally enlarged and hardened due to infiltration and proliferation of metastatic cancer cells in the LNs. In Fig. 28.4b, c, although the metastatic lesions were present on the LNs but remained unrecognized on the white-light imaging, they could be clearly and accurately identified by the PpIX-fluorescence diagnostic method.
The PpIX-fluorescence diagnostic method provides high sensitivity and accuracy for the diagnosis of LN metastasis in this model. Figure 28.5 shows scatterplots of the fluorescence intensity ratios of metastatic and nonmetastatic LNs of the orthotopic mouse model of human rectal cancer at 6 and 9 h after 5-ALA injection. The mean intensity ratios were 3.67 ± 1.38 in the metastatic LNs and 0.99 ± 0.15 in the nonmetastatic LNs. The PpIX-fluorescence diagnostic method identified all metastatic and nonmetastatic LNs when the cutoff of the intensity ratio was set at 1.7.
Fig. 28.5
Scatterplots of the fluorescence intensity ratio between excised metastatic and nonmetastatic LNs of mice with rectal cancer 6 and 9 h after administration of 5-ALA. The decision line (1.7) yields sensitivity of 100 % and specificity of 100 % for differentiating metastatic from nonmetastatic LNs. Filled circles and open rectangles denote metastatic LNs and nonmetastatic LNs, respectively. With permission from Murayama Y, Harada Y, Imaizumi K, Dai P, Nakano K, Okamoto K, et al. Precise detection of lymph node metastases in mouse rectal cancer by using 5-aminolevulinic acid. Int J Cancer 2009;15;125(10):2256–63. © 2009 John Wiley and Sons [19]
In histological analysis of surgical specimens, simplified examination of HE-stained sections is generally performed, i.e., a few slides obtained from each LN with spacing of a few millimeter are analyzed for rapid diagnosis. Although precise HE staining analysis of whole LNs with narrow spacing of serial sections (<100 μm) provides definitive diagnosis of LN metastasis, the simplified HE staining analysis sometimes yields false-negative result due to the finite number of sections of metastatic LNs [32–34]. The PpIX-fluorescence detection method requires no thin sectioning of LNs and no time-consuming preparation for diagnosis and thus has the potential to allow detection of LN metastasis including small metastatic lesions that might otherwise lead to diagnostic error in the analysis with the simplified HE staining analysis.
Procedure of Fluorescence Detection of LN Metastasis Using 5-ALA in Human Gastrointestinal Cancer Patients
Appropriate Patients
Since 5-ALA is naturally generated in the human body, it is considered to be relatively safe even after exogenous administration. Indeed, 5-ALA is commercially distributed worldwide as a medicinal drug for photodynamic diagnosis of bladder cancer and malignant glioma and for photodynamic therapy of actinic keratosis and condyloma acuminatum.
Since 5-ALA is metabolized to heme, its use in patients with metabolic diseases of heme synthesis such as acute or chronic porphyria is inappropriate. Hypersensitivity to 5-ALA or porphyrins is also a major contraindication. The liver and kidneys are two of the main accumulation sites for the excretion of 5-ALA; 5-ALA should be used with caution in patients with renal or hepatic insufficiency.
Administration of 5-ALA
For the detection of LN metastasis in gastrointestinal cancer patients, oral administration of 5-ALA is generally performed [26, 27, 35]. In general, 5-ALA hydrochloride dissolved in water with 50 % glucose is applied orally at a concentration ranging from 15 to 20 mg per kg of body weight. Although the concentration of 5-ALA for oral administration is based on comparison with the detection of primary tumors such as glioma, the optimal administration concentration of 5-ALA for the detection of LN metastasis of various cancers is now under investigation. After the administration of 5-ALA, patients should be protected from strong light such as direct sunlight for 24–48 h to avoid photosensitivity reaction.
Various groups reported that the half-life of 5-ALA in the human body is approximately 45 min, and the maximum concentration of PpIX in blood is reportedly approximately 6–9 h after oral administration of 5-ALA [36–38]. Therefore, in general surgery for gastrointestinal cancer, in which LNs are excised in about 3–5 h after general anesthesia, 5-ALA should be administered to the patients 2–4 h prior to induction of general anesthesia.
Side Effects of 5-ALA Administration
The side effects of the administration of 5-ALA have been investigated in patients in several studies [35, 38, 39]. Although substance-specific side effects, such as hypotension, nausea, photosensitivity reaction, and photodermatosis, are reported, these effects are uncommon reactions (less than 1 % incidence). Other side effects such as anemia, thrombocytopenia, leukocytosis, and impairment of liver function have also developed after surgery; however, these seem to be related to procedure involved in the surgery.
Sample Preparation
Tissues including LNs at several sites at which metastatic lymph nodes are suspected to be present are carefully removed during gastrointestinal surgery. The LNs are isolated from the resected tissues and are analyzed immediately, avoiding unnecessary light exposure. For precise analysis of PpIX fluorescence from the LNs, if necessary, the LNs are cut into a few parts with a fine blade due to the limited penetration depth of excitation light. Fluorescence imaging of the cut surface and diagnostic evaluation of LN metastasis are performed. After the PpIX-fluorescence diagnostic evaluation, the LNs are subjected to a postoperative histopathological diagnosis for precise evaluation of disease.
Fluorescence Detection of LN Metastasis Using 5-ALA for Human Gastrointestinal Cancer Patients
Fluorescence Detection of LN Metastasis for Gastric Cancer Patients
In this section, we introduce some applications of fluorescence diagnosis of LN metastasis using 5-ALA in human gastrointestinal cancer patients. Firstly, the detection of LN metastasis of gastric cancer is presented.
Figure 28.6 shows representative images of metastatic and nonmetastatic LNs from gastric cancer patients [27]. 5-ALA hydrochloride at 15 mg per kg of body weight was dissolved in 20 ml of 50 % glucose solution and administered orally to the patients 2 h prior to induction of general anesthesia. Isolated lymph nodes were cut in half longitudinally one by one with a fine blade. Fluorescence images of the cut surface were obtained by using a stereomicroscope that comprised a 405-nm band-pass filter for excitation and a color CCD camera equipped with a 430-nm long-pass filter for emission. In practice, the peak wavelength of PpIX fluorescence is about 635 nm, and the fluorescence from PpIX must be filtered with its peak wavelength to obtain the optimum contrast of the PpIX image. Since the PpIX fluorescence observed in the red channel of the color CCD camera is relatively strong compared to the background autofluorescence, the color CCD camera is widely used for the observation of PpIX fluorescence owing to its convenience for use. Furthermore, blue and green fluorescence predominantly represents the distribution of flavins, collagens, and fats, and the analysis of RGB channels of the color CCD camera provides us data for not only the distribution of PpIX but also the distribution of parenchyma and stroma of LNs.
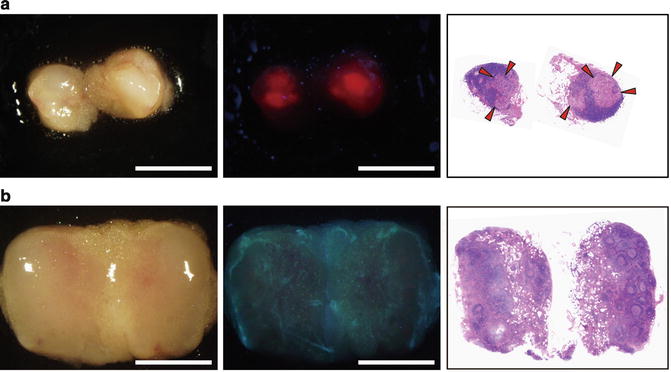
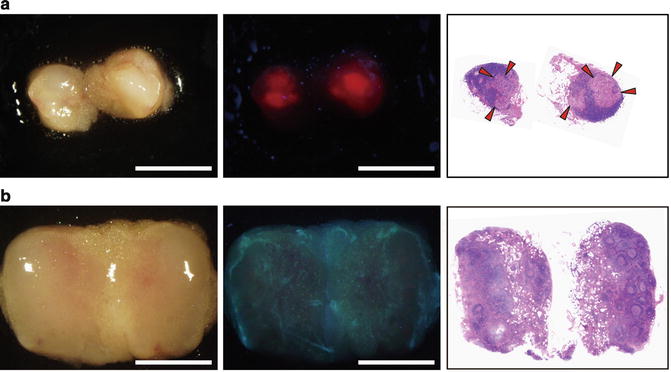
Fig. 28.6
Representative images of (a) metastatic and (b) nonmetastatic LNs from gastric cancer patients. (left) White-light and (center) fluorescence images obtained with a color CCD camera and (right) image of HE-stained specimens from each lymph node are shown. Arrowheads indicate metastatic lesions. Scale bar = 3 mm. With permission from Harada K, Harada Y, Beika M, Koizumi N, Inoue K, Murayama Y, et al. Detection of lymph node metastases in human colorectal cancer by using 5-aminolevulinic acid-induced protoporphyrin IX fluorescence with spectral unmixing. Int J Molecular Sci 2013;14(11):23140–52.© Springer [26]
In the metastatic LNs, strong red fluorescence was observed, and the distribution coincided with malignant lesions that were confirmed by HE stain image. In contrast, red fluorescence was weak in nonmetastatic LNs. Results for quantitative analysis of fluorescence intensity of LNs observed on the R channel of the color CCD camera are shown in Fig. 28.7. The fluorescence intensities of the metastatic and nonmetastatic LNs without follicular accumulation are significantly different.
Fig. 28.7
Quantitative analysis of fluorescence intensity of metastatic and nonmetastatic LNs observed in the R channel of the color CCD camera. The fluorescence intensity of the R channel is normalized with total fluorescence of RGB channels to eliminate individual variation of autofluorescence. The normalized fluorescence intensity of the R channel between metastatic lymph nodes and nonmetastatic lymph nodes without follicular accumulation showed significant difference (p < 0.0001). With permission from Harada K, Harada Y, Beika M, Koizumi N, Inoue K, Murayama Y, et al. Detection of lymph node metastases in human colorectal cancer by using 5-aminolevulinic acid-induced protoporphyrin IX fluorescence with spectral unmixing. Int J Molecular Sci 2013;14(11):23140–52.© Springer [26]
Diagnostic accuracy of the PpIX-fluorescence diagnosis was evaluated with 144 LNs. The PpIX-fluorescence diagnosis was compared with histopathological diagnosis as the gold standard for the detection of LN metastasis. Totals of 17 out of 24 metastatic LNs and 106 out of 120 nonmetastatic LNs were detected by the PpIX-fluorescence diagnostic method with agreement with the histopathological diagnosis. The overall diagnostic accuracy of gross fluorescence inspection was 85.4 % (123/144).
For the PpIX-fluorescence diagnosis, there were false-positive results for 14 nonmetastatic LNs that were deemed to be metastatic and false-negative results for 7 metastatic LNs that were deemed to be nonmetastatic. False-positive results were mainly due to the accumulation of PpIX in normal lymphoid follicles [40, 41]. The normal lymphoid follicles exhibit specific accumulation patterns of PpIX, and the diagnostic specificity and accuracy are, respectively, improved from 88.3 to 96.7 % and from 85.4 to 92.4 % after special consideration of the fluorescence patterns of the malignant lesions and the normal lymphoid follicles. In false-negative results, it is considered that extraneous fluorescence from nonmetastatic regions such as that from collagen, flavins, and fats obscures the PpIX fluorescence from metastatic LNs; in particular, some of the metastatic LNs of patients with scirrhous carcinoma could not be detected owing to strong autofluorescence emitted from increased amount of fibrous tissues. To eliminate the autofluorescence from nonmetastatic regions, detailed analysis of fluorescence spectra of PpIX and nonmetastatic regions is required. One technique of spectral analysis to eliminate autofluorescence of nonmetastatic regions is presented in the next subsection. Individual variation of absorption capacity of 5-ALA may also be in part responsible for false-negative results. Because 5-ALA is mainly absorbed at the upper gastrointestinal tract, patients with diseased stomach may take in 5-ALA of insufficient dose.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree