Fig. 1 a–c.
Three-dimensional evaluation of prosthesis components with reconstruction of the mechanical axis femoral and tibial resulting in a 3 degree varus (a). Easy measurement of femoral varus/valgus, femoral flexion/extension and femoral rotation (b). The tibial component slope and the tibial rotation are defined (c) (for color reproduction see p 313)
Image Fusion
The fusion is usually performed with the vendor’s software package and provides perfect matched images in most cases. In some cases, for example when technical defects of the SPECT/CT scanner occur with the CT component, it is possible to use an available dedicated CT system and fuse the images afterwards on the workstation. The modern voxel-based algorithms often produce good results; the quality of results in descending order is: hip, knee and shoulder. Because of the very complex anatomy, this method does not usually give reliable results for the foot and ankle.
Examination Recommendations
Patient support: position your patient in a comfortable pain-free position! Because of the long examination time up to 45 min, pain can cause distinct motion artefacts, which can compromise the whole examination. In some cases, it is necessary to apply painkillers intravenously. Pain and long examination times can be disadvantageous when using special devices to standardize patient position or simulate weight-bearing images.
Image Analysis: Look at Everything
First, analyze the scintigraphic images, including early phase images, and address the following points: the presence/ absence of hyperemia; tracer distribution and spot localization; prosthesis component — one/both sides; location of hot spots to the prosthesis; bone/cement interface; intensity on the whole body scan.
Second, obtain morphological information from CT scan and address the following points: bone density; presence/ absence of focal osteopenia; presence/absence of granulomas/osteolysis; component position; relation to mechanical axis; available conventional X-rays; type of prosthesis; cemented or uncemented; coating of the prosthesis, if known (e.g., hydroxyapatite). There is a strong relationship between biomechanical principles of the prosthesis model, mechanical fixation and possible uptake patterns; therefore, it is necessary talk to the orthopedic surgeon.
Combine All Your Information
Is there a special uptake pattern? Can it be explained by malpositioning or malrotation? Also, it is important to detect stress reactions, as these can lead to a misdiagnosis of loosening.
In summary, the complex situation in many patients requires a stringent interdisciplinary approach.
SPECT/CT in Different Regions
Shoulder
The number of patients who receive a shoulder arthroplasty is steadily increasing [11–14]. The spectrum of devices includes resurfacing techniques, and partial prosthesis up to complex inverse prosthesis types [12, 13]. Compared with other joints, the spherical component of the head causes strong beam hardening artefacts that make it difficult to analyze the images. The orthopedic point of view focuses on the following questions:
1.
Bone quality: is there osteolysis?
2.
Are there signs of aseptic loosening?
3.
Are there signs of aseptic loosening?
4.
Are there signs of acromial impingement as possible cause of pain, which can be easily seen as zone of hypermetabolism on the acromion?
5.
Bone stock glenoidal before revision surgery: is thereenough bone to fix the component?
6.
Are there signs of infection?
7.
If there is sign of infection, carry out additional antigranulocyte-SPECT-CT as a second examination.
The literature regarding the use of SPECT/CT in shoulder prostheses is limited to case reports [11].
Practical recommendations:
The affected arm/shoulder should lie in a neutral position, and the other arm should be elevated above the head. This “swimmer” position reduces artefacts caused by both shoulders. The head should be turned to one side to allow the camera to scan close to the body surface.
Hip
Hip arthroplasty is currently one of the major orthopedic arthroplasty procedures. Indications are: unexplained pain in the postoperative setting (15–20% of all patients), suspicion of loosening, suspicion of infection, and detection of other/additional causes of pain such as spine pathologies. Before analyzing the images the following questions should be answered:
1.
Are the components cemented or uncemented?
2.
In cases of uncemented components, what is the type of fixation: proximal or distal?
3.
What type of cup fixation has been used: press-fit or screws?
It is very important to differentiate between cemented and uncemented types of prosthesis. The uncemented shafts usually show a proximal or distal fixation zone where enostal thickening of the bone associated with focal higher uptake can appear. This is equivalent to a biomechanical stress reaction and physiological bone remodeling process, which should not be misinterpreted as aseptic loosening (Fig. 2). Usually — with the exception of the new hydroxyapatite-coated femoral shafts — a small boneless margin (smaller than 2 mm) around the shaft can be seen. Every focal widening or irregularity is suspicious of loosening. The cortical bone should be homogeneous. Distal periostal thickening distal is suspicious of micromotion of the shaft and can indicate loosening in cases of a proximal fixed prosthesis.
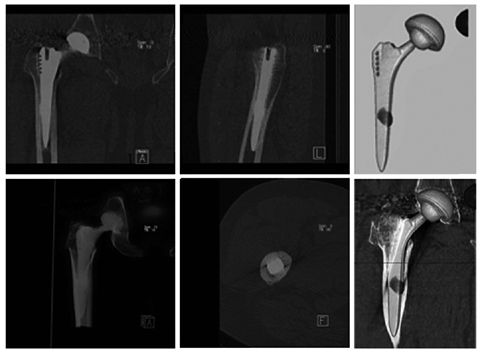
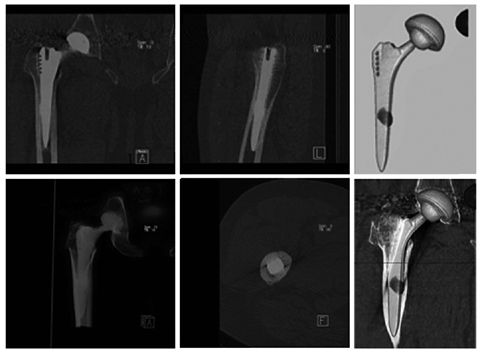
Fig. 2
A 54-year-old man with hip replacement on the right side 6/2008. Four years after surgery, pain is experienced under stress. SPECT-CT shows intact prosthesis components. Only slight uptake in the midshaft. Minimal varus of the shaft. Diagnosis: no loosening, slight uptake in the fixation zone and stress reaction caused by a minimal varus. The surgeon did not believe the diagnosis and the patient underwent revision. No loosening was found intraoperatively (for color reproduction see p 314)
In cases of a cemented shaft, the cement layer should not show any sign of breaking, which is a clear sign of loosening. Osteopenic areas, especially in the trochanter, can indicate either cement problems (a thin layer that cannot distribute the pressure adequately) or component malposition, such as varus with high pressure in the trochanter minor (higher focal uptake) and less pressure in the trochanter major (less uptake). In cases of an uncemented cup, uptake can usually be seen in the cranial parts of the acetabulum, where the main force vectors are located. Any other uptake localization should lead to careful evaluation of the acetabular bone to exclude osteolysis/ granulomas and pathological margins >2 mm. In cases of wide margins and large granulomas, the pathology is often seen in the CT scans only, and the scinti — graphy is negative. This pathology can be missed on planar images and SPECT alone. Some cups are fixed by winding in the bone. In these cases, small focused margins and only focal missing contact between the winding and the bone is normal and is related to the operative technique. These morphological patterns do not represent any loosening. Particularly in revision surgery, the cups are often fixed with additional screws. The analysis should consider material failure. The screws should not reach far into the pelvis as this can cause muscle problems (irritation or hematoma in the iliacus muscle) or pelvic nerve irritation. For cemented cups, the same criteria used for the shaft can be applied. Subsequently, the head should be assessed to detect signs of wearing, which is usually seen as asymmetric narrowing of the joint space. It is necessary to at least have a close look at the soft tissue (is there presence of a hematoma or pseudotumor?) and ectopic ossifications, which sometimes show an inflammatory component in the early phase or can cause mechanical problems limiting the range of motion.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







