Fractures are common in children, although accurate diagnosis is confounded by mimics of fractures some of which are unique to the pediatric population. Such fracture mimics include developmental variations of the growth plates, normal anatomic structures that simulate fracture lines, and/or metabolic disorders that alter the pattern of ossification. Although subtle clues on plain radiographs may help to discriminate between a true fracture or injury and a fracture mimic, MR imaging may be helpful to eliminate uncertainty or expedite diagnosis.
Key points
- •
Pediatric fractures are subtle and may mimic other conditions.
- •
Growth plates in children are a common source of confusion regarding presence or absence of fracture.
- •
Patterns of injury in children are different from those in adults.
- •
MR imaging features of trauma include bone marrow and soft tissue edema, and subtle fracture lines, and help clarify equivocal plain radiographic findings.
Introduction
Osseous injuries are common in children and constitute 10% to 15% of all childhood injuries. The risk of developing a fracture by age 16 years is 42% for boys and 27% for girls. Fractures are more common in children than in adults following minimal trauma, related to a proportionate increase in the amount of cartilage and collagen within the pediatric skeleton contributing to a reduced strength of the immature skeleton compared with adults. Growth spurts represent an additional point of risk for the pediatric skeleton as bone strength and development lags behind muscle mass. Patterns of injury in pediatric patients can subtle, and it is these subtle injuries that may elude even the most experienced reader. Radiologists and clinicians presented with skeletal radiographs in pediatric patients must be well equipped to differentiate fracture from the numerous mimics of fracture that exist in this population. Fracture mimics include developmental variations of the growth plates and secondary ossification centers, normal osseous landmarks that simulate fracture lines, and metabolic disorders that affect the pattern and rate of ossification. There are various imaging clues that allow for distinguishing fractures from mimics on plain radiographs, although MR imaging may be useful when there is uncertainty or when expedited diagnosis is required ( Table 1 ).
| Injury | Mimic |
|---|---|
| Salter 2 fracture | Developmental physeal variants |
|
|
| Salter 3 fracture | Cleft epiphyses |
| Avulsion fracture | Accessory ossification centers |
| Greenstick fracture | Nutrient foramina |
| Stress fracture | Osteoid osteoma |
| Vertebral compression fracture |
|
Physeal injuries and mimics
The most common source of pitfalls in diagnosing skeletal trauma in pediatric patients is the growth centers. Physeal injuries represent approximately 20% of pediatric fractures. A baseline understanding of the normal appearance of the physis is critical to differentiating fractures from normal growth centers. Although the cartilaginous physis of long bones is flat at birth, over time it develops irregularities in response to increased biomechanical forces. These undulations serve to increase the shear strength of the physis. The physis represents a source of weakness within the skeleton, which accounts for why fractures so often involve this structure. The Salter-Harris classification is the most commonly used classification system for physeal injures. The original five Salter-Harris fracture types are the most widely used when describing physeal fractures. Salter-Harris fractures are distinguished from each other based on the pattern of involvement of the metaphysis, epiphysis, or both. In certain locations normal variants may mimic a physeal fracture. Variants are divided into three categories: (1) those that represent chronic chondro-osseous disruption, (2) those that predispose to traumatic and/or degenerative change, and (3) those that predispose to premature degenerative change.
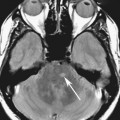
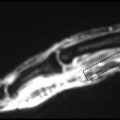
The Salter 2 fracture is the most common Salter-Harris fracture, constituting approximately 75% of Salter-Harris fractures. In a Salter 2 fracture the plane of the fracture propagates transversely through the physeal cartilage before exiting into the metaphysis. The most common sites include the distal radius, phalanges, and distal tibia. The pattern of injury may be difficult to characterize on plain radiographs alone, and MR imaging is useful ( Fig. 1 ). Small metaphyseal or epiphyseal fractures may be missed on plain radiographs, whereas they are plainly visible at MR imaging or computed tomography (CT). Physeal variants may mimic a Salter 2 fracture, such as within the distal fibula ( Fig. 2 ) or proximal radius ( Fig. 3 ). In some patients there is a vertical extension of physeal cartilage extending into the fibular metaphysis at the lateral margin of the physis. Diagnosis may be confounded by recent history of trauma. The normal fibular physis is wider laterally than it is medially, often with irregular ossification patterns at the lateral margin of the distal fibular physis, which may raise concern for a physeal fracture. MR imaging may be helpful to detect more detailed information about the pattern of injury, such as subtle fracture lines, bone marrow edema, or fluid signal within the physis.



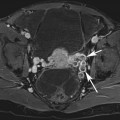
In a Salter 1 fracture, the fracture propagates through the physis without metaphyseal or epiphyseal extension. If there is no periosteal disruption, the bone remains appropriately aligned and the only manifestation of the acute fracture is widening or irregularity of the physis ( Fig. 4 ). This may be difficult to appreciate given expected physeal irregularity. Abnormal widening of the physis is also present in the context of chronic physeal stress changes. In this background, repetitive, forceful loading activities leading to overuse of an extremity can cause shear injury and microtrauma to the cartilaginous physis. This differs from a Salter 1 fracture, because there is no fracture line but rather disorganized enchondral ossification leading to hypertrophic cartilage extending into the metaphysis. Although a Salter 1 fracture usually involves the entire physis, chronic stress change is focal or diffuse. A classic location includes the proximal humeral physis in overhead throwing athletes, termed Little Leaguer’s shoulder. On radiographs this is manifest as a widened proximal humeral physis, which appears asymmetrically irregular when compared with the contralateral side, with associated periphyseal sclerosis ( Fig. 5 ). Similar physeal stress changes may occur in the distal radius in patients who engage in sports that involve weightbearing with the upper extremities, such as gymnasts ( Fig. 6 ), or in the distal femurs or proximal tibiae of children who participate in aggressive physical activity using their lower extremities, such as soccer or running ( Fig. 7 ). The physis is wide and irregular and there is periphyseal sclerosis reflecting the healing response. MR imaging is helpful at revealing the presence of marrow edema and fluid within the physis that is present in the setting of trauma. In the hip, slipped capital femoral epiphysis is a condition that is considered a Salter 1 equivalent injury that ultimately results in displacement of the femoral heal, usually in a posteromedial orientation. The diagnosis is most often made with plain radiographs, although when the degree of epiphyseal displacement is subtle or when displacement has not yet occurred the abnormalities are best appreciated at MR imaging ( Fig. 8 ).





Certain metabolic conditions that cause disruption of the normal pattern of enchondral ossification at the physis may mimic traumatic or stress-induced injuries, including rickets. Rickets is a group of conditions related to deficiency of (or resistance to) vitamin D or its derivative. This manifests as disordered enchondral ossification with disruption of the normal configuration of the physis. Radiographs demonstrate abnormal widening of the physis associated with decreased density in the zone of provisional calcification (ZPC). MR images demonstrate widening of the physes with increased physeal T2-weighted signal, with absent ZPC ( Fig. 9 ). Key imaging features that enable differentiating rickets from trauma are the absent ZPC, and lack of metaphyseal marrow edema (or mild edema). The classic radiographic changes may take longer to manifest, and include irregular, cupped, and/or frayed metaphyses. Although these features are easily detected on plain radiographs, they may not be present in the early stages of the disease process. The physes of patients with rickets are at least 50% wider than the physes of normal, age-matched control subjects. In the early stages of rickets, the imaging features mimic stress-related changes. In the appropriate clinical context it should not be necessary to perform MR imaging to distinguish between these two conditions given the subtle radiographic clues that help make the distinction (ie, absent ZPC in rickets) in addition to differing clinical presentations. Stress changes tend to occur in older children known to be involved in activities that would predispose to these types of injuries. Patients with rickets have laboratory abnormalities that coincide with the imaging manifestations of the disease. MR imaging may be useful in confounding cases. Increasingly, active patients with a history of rickets are developing risk factors for stress-related physeal changes. Plain radiographic imaging may not be well-suited to determine the underlying cause for the physeal change, and treatment choice depends on whether the ZPC is present (in the setting of stress changes) or absent (in the setting or rickets) ( Fig. 10 ).


Patients with other diffuse metabolic conditions may also demonstrate skeletal findings that may mimic physeal microtrauma. Shwachman-Diamond syndrome (SDS) is an autosomal-recessive condition described in patients with pancreatic insufficiency, bone marrow dysfunction, and metaphyseal chondrodysplasia. Skeletal findings are symmetric metaphyseal changes in the hips and knees, such as periphyseal irregularity with mixed lytic and sclerotic areas ( Fig. 11 ). In the femoral neck the physis becomes wedge-shaped over time and grows into a cone-shaped defect in the metaphysis. The skeletal manifestations of the disorder are not present in all patients, and the imaging of patients with SDS focuses mainly on the abdominal manifestations of the disease, which includes pancreatic lipomatosis. MR imaging is believed to be helpful in the diagnosis of SDS and differentiation from other conditions with exocrine pancreatic insufficiency, such as cystic fibrosis, and the hips may be included in the field of view when evaluating the abdomen. The metaphyseal dysosostosis that affects patients with SDS may mimic an advanced form of physeal stress injury.


Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree