Placenta and Umbilical Cord
INTRODUCTION
The placenta is a highly specialized organ that supports growth and development of the fetus and serves as the interface between the maternal and fetal circulations. The placenta functions as the pregnancy organ that delivers nutrients, exchanges respiratory gas, and eliminates toxic waste. The placenta is also an important endocrine organ producing hormones to support and sustain pregnancy and plays a critical role in prevention of pregnancy rejection. Impairment in placental development and/or function has a profound impact on pregnancy outcome. Accumulating data suggest that the placenta plays a critical role in the future health of the fetus such as the risk for adult-onset cardiovascular disease among other diseases.1, 2, 3, 4 This chapter presents the embryologic development and normal sonographic appearance of the placenta and umbilical cord and discusses common placental and cord abnormalities that can be detected in the first trimester of pregnancy.
EMBRYOLOGY
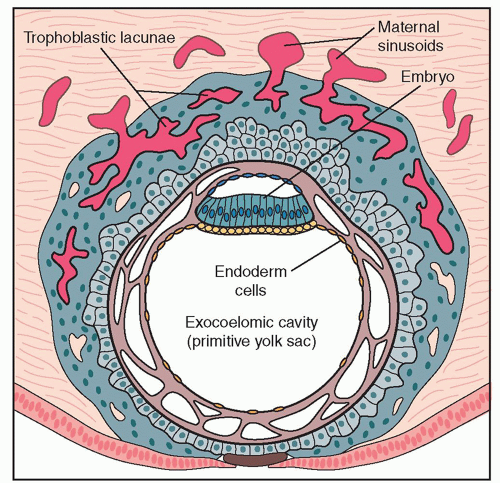
The blastocyst reaches the endometrial cavity at 4 to 5 days postfertilization. The outer surface of the blastocyst differentiates into trophoblastic cells and produces an overlying syncytial layer that adheres to the endometrium. Implantation of the blastocyst then commences as the syncytiotrophoblast cells penetrate the decidualized endometrium. Endometrial gland secretions provide nourishment to the embryo at this early stage. Spaces are then developed within the syncytiotrophoblast and form anastomosis with maternal vascular sinusoids, thus establishing the first (lacunar) uteroplacental circulation (Fig. 15.1). The placental circulation then develops with finger-like projections into the maternal blood spaces. These projections extend from the chorion and form the primary villi with an inner layer of cytotrophoblast and an outer layer of syncytiotrophoblast. The primary villi become secondary villi with the invasion of the extraembryonic mesoderm and finally become tertiary villi as embryonic blood vessels develop within them. In the early stages of placental development, cytotrophoblasts invade the endothelium and smooth muscle of endometrial spiral arteries, releasing them from maternal influences. The fully formed human placenta is termed hemochorial because the maternal blood is separated from the fetal blood only by elements of the chorion. Growth in size and thickness of the placenta continues rapidly in the first trimester and into the second trimester of pregnancy. The term placenta has a fetal portion, the chorion frondosum, and a maternal portion, the decidua basalis, and covers 15% to 30% of the decidua of the endometrial cavity.5 The placenta at term is about 20 cm in diameter, has a volume of 400 to
600 mL, and weighs approximately one-sixth as much as the fetus.5,6
600 mL, and weighs approximately one-sixth as much as the fetus.5,6
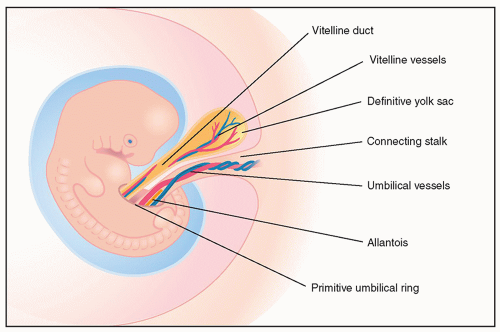
In early embryogenesis, two stalks are seen: the yolk sac, ventrally located and containing the vitelline duct and vessels, and the connecting stalk, caudally located and containing the allantois and the umbilical vessels (Fig. 15.2). With cephalocaudal flexion of the embryo, the connecting stalk fuses with the yolk sac stalk to form the umbilical cord. The umbilical cord in its early development is inserted in the lower ventral portions of the embryo, is short and thick, and contains the allantois, the vitelline duct and vessels, and the umbilical vessels. The amnion covers the umbilical cord and becomes continuous with the outer epithelial layer of the embryo. The umbilical cord elongates and thins out with the development of the anterior abdominal wall. The umbilical cord initially attaches centrally to the developing
placenta. As the placenta grows, it tends to expand preferentially in regions with sufficient myometrial perfusion and atrophy in areas with suboptimal blood supply. As a result, the cord insertion may become somewhat eccentric. This process is known as trophotropism. The umbilical cord consists of two umbilical arteries and one vein, which are surrounded by mucoid connective tissue—Wharton jelly. The cord at term is usually 1 to 2 cm in diameter and 30 to 90 cm in length.
placenta. As the placenta grows, it tends to expand preferentially in regions with sufficient myometrial perfusion and atrophy in areas with suboptimal blood supply. As a result, the cord insertion may become somewhat eccentric. This process is known as trophotropism. The umbilical cord consists of two umbilical arteries and one vein, which are surrounded by mucoid connective tissue—Wharton jelly. The cord at term is usually 1 to 2 cm in diameter and 30 to 90 cm in length.
NORMAL SONOGRAPHIC ANATOMY
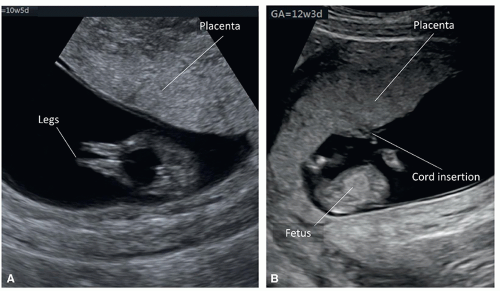
The placenta is first recognized sonographically as a thickened echogenic region on the endometrium by about 9 to 10 weeks of gestation (Figs. 15.3 and 15.4A). By 12 to 13 weeks of gestation, the placenta is easily seen on ultrasound and appears slightly echogenic with uniformed homogeneous echotexture (Figs. 15.4B and 15.5).
During the first trimester ultrasound examination (see Chapter 5), the location of the placenta in the uterus should be reported. Identifying the location of the placenta on the first trimester ultrasound is not as easy as in the second trimester given the presence of uterine flexion and extension. Indeed, inaccuracies can be introduced especially when the placenta appears to be in the lower uterine segment. In order to improve accuracy of placental localization on the first trimester ultrasound, we recommend identifying the cervix and the anterior and posterior uterine walls before describing the placental location (Figs. 15.6 and 15.7).
The placental size, thickness, location within the endometrial cavity, and echogenicity can also be evaluated by ultrasound in the late first trimester of pregnancy.7 The normal thickness of the placenta is correlated to gestational age of the embryo/fetus and is approximately 1 mm per week of gestation.8 With advanced three-dimensional (3D) ultrasound techniques, placental volume can now be measured in the first trimester
(Fig. 15.8), and along with placental biometry has been shown to correlate with pregnancy complications.9,10 Indeed, we believe that first trimester measurement of placental length, width, and volume is more accurate than later on in pregnancy given that the whole placenta is seen in one ultrasound image in early gestation. The assessment of biometric dimensions of the placenta is infrequently performed on prenatal sonography today, unless in rare pathologic conditions or for research purposes. Abnormal placental findings on first trimester ultrasound, such as masses, multiple cystic spaces, or large subchorionic fluid collection, should be noted and followed up.
(Fig. 15.8), and along with placental biometry has been shown to correlate with pregnancy complications.9,10 Indeed, we believe that first trimester measurement of placental length, width, and volume is more accurate than later on in pregnancy given that the whole placenta is seen in one ultrasound image in early gestation. The assessment of biometric dimensions of the placenta is infrequently performed on prenatal sonography today, unless in rare pathologic conditions or for research purposes. Abnormal placental findings on first trimester ultrasound, such as masses, multiple cystic spaces, or large subchorionic fluid collection, should be noted and followed up.
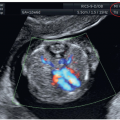
Maternal blood flow is established within the placenta by 12 weeks of gestation.11 Blood flow in the maternal and fetal placental vasculature can be demonstrated in the first trimester on color and pulsed Doppler ultrasound (Fig. 15.9).
Quantitative assessment of placental vascularization may be useful for predicting pregnancy complications and adverse events.12, 13, 14
Quantitative assessment of placental vascularization may be useful for predicting pregnancy complications and adverse events.12, 13, 14
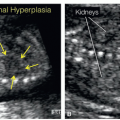
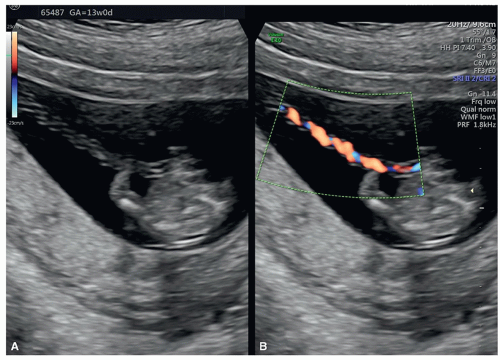 Figure 15.11: Two-dimensional ultrasound in gray scale (A) and color Doppler (B) of the umbilical cord in a pregnancy at 13 weeks of gestation. Note in A and B that the umbilical cord is elongated and thinned from its appearance between 7 and 10 weeks of gestation (Fig. 15.10). The umbilical cord at 13 weeks of gestation has the same appearance as that in the second trimester of pregnancy. |
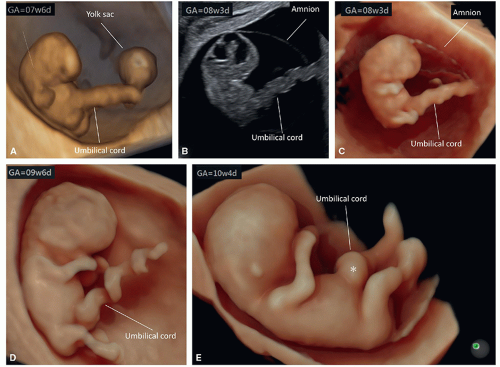
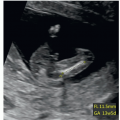
The umbilical cord can be recognized by ultrasound as early as the seventh week of gestation and appears as a straight thick structure connecting the embryo to the developing placenta (Fig. 15.10). In the first trimester, the length of the umbilical cord is approximately the same as the crown-rump length.15 The umbilical cord elongates and thins with advancing gestation, and by the 13th week, the cord has the same sonographic appearance as in the second trimester of pregnancy (Fig. 15.11). Umbilical arteries can be seen in the first trimester as branches of the internal iliac arteries, running alongside the fetal bladder in a cross-section view of the fetal pelvis using color or power Doppler (Fig. 15.12A), and the number of umbilical arteries can thus be reliably determined.16 Midline sagittal plane of the fetus demonstrates the insertion of the umbilical cord into the abdomen, and this plane is also important in the evaluation of the integrity of the abdominal wall in the first trimester (Fig. 15.12B) (see Chapters 5 and 12). 3D ultrasound in surface mode can also clearly demonstrate the umbilical cord (Fig. 15.13).
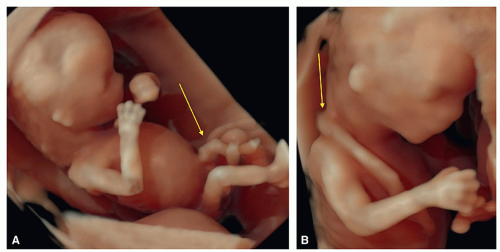 Figure 15.13: Three-dimensional ultrasound in surface mode in two fetuses at 12 (A) and 13 (B) weeks of gestation demonstrating external fetal anatomy along with the umbilical cord (arrow). |
PLACENTAL ABNORMALITIES
Intrauterine Hematoma
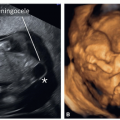
Intrauterine hematoma is a common finding on routine ultrasound in the first trimester, especially among pregnant women presenting with vaginal bleeding. Intrauterine hematoma usually appears as a crescent-shaped, sonolucent fluid collection behind the fetal membranes or the placenta, but may vary significantly in shape and size. The position of the hematoma relative to the placental site can be described as subchorionic or retroplacental. The subchorionic hematoma is located between the chorion and the uterine wall (Fig. 15.14), whereas the retroplacental hematoma is located behind the placenta (Fig. 15.15). The reported incidence of first trimester hematomas diagnosed by ultrasound varies widely, from as low as 0.5% to as high as 22%, depending on the patient population studied and the ultrasound evaluation.17,18 In low-risk general obstetric population, intrauterine hematomas occur in 3.1% of cases in the first trimester.19 Although approximately 70% of subchorionic hematomas resolve spontaneously by the end of the second trimester without clinical sequelae, some may persist until the end of pregnancy and be associated with increased risk of pregnancy complications.17
 Figure 15.15: Two-dimensional ultrasound with color Doppler in a pregnancy at 10 weeks of gestation demonstrating a retroplacental hematoma (asterisk and arrows) located behind the placenta. |
The clinical significance of an intrauterine hematoma noted on the first trimester ultrasound is currently controversial.20, 21, 22, 23, 24 Systematic review and meta-analysis performed by Tuuli et al.25 demonstrated that presence of a first trimester intrauterine hematoma is associated with adverse pregnancy outcome, including an increased risk for spontaneous abortion, stillbirth, placental abruption, preterm premature rupture of membranes, and preterm delivery. There is no consistency in study results, however, and the association of an intrauterine hematoma with pregnancy complications such as preeclampsia and fetal growth restriction has not been confirmed.25 Retroplacental position of the hematoma (Fig. 15.15) appears to carry a higher risk for poor pregnancy outcome.19 An intrauterine hematoma can be classified based upon its relative size. In a study on this subject, the size of the hematoma was graded according to the percentage of chorionic sac circumference elevated by the hematoma, with small indicating less than one-third of the chorionic sac circumference, moderate indicating one-third to one-half of the chorionic sac circumference, and large indicating two-thirds or greater of chorionic sac circumference.22 Large intrauterine hematomas (Fig. 15.16) were found to be associated with an almost threefold increase in risk of spontaneous abortion.22 There is currently sufficient evidence in the literature to suggest that the presence of a first trimester large intrauterine hematoma may increase the pregnancy risk, and follow-up ultrasound examinations in the second and possibly third trimester of pregnancy is thus warranted.
Although a subchorionic hematoma is relatively easy to identify in the first trimester, the diagnosis of a subplacental hematoma is challenging especially in the absence of clinical symptoms. The presence of a transient uterine contraction (see
Fig. 5.1) or thickened uterine wall can mimic the diagnosis of subplacental bleed. The application of color Doppler can help differentiate a subplacental bleed from a uterine contraction or thickening.
Fig. 5.1) or thickened uterine wall can mimic the diagnosis of subplacental bleed. The application of color Doppler can help differentiate a subplacental bleed from a uterine contraction or thickening.
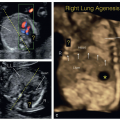
Placenta Previa
The term placenta previa describes a placenta that covers the internal cervical os. In normal pregnancy, the placenta implants in the upper uterine segment. In the case of placenta previa, the placenta is partially or totally implanted in the lower uterine segment and placental tissue covers the internal cervical os (Figs. 15.17 and 15.18). In the second trimester of pregnancy, if the placenta is attached in the lower uterine segment and placental tissue does not cover the internal os, but is within 2 cm from the internal os, the placenta is called low lying.
 Figure 15.18: Two-dimensional transvaginal ultrasound in a pregnancy at 13 weeks of gestation demonstrating a placenta previa. Note that the placenta is covering the internal cervical os. |
The incidence of placenta previa varies greatly with gestational age. Placenta previa is more commonly seen in early gestation and presents in approximately 4.5% to 6.2% of pregnancies between 12 and 16 weeks of gestation.26,27 The proportion of patients with the placenta extending to or covering the internal cervical os significantly decreases with advancing gestation from 5.5% at 12+0 to 12+6 weeks, to 2.4% at 15+0 to 15+6 weeks of gestation and to 0.16% at term.26 Several studies have shown that if the placenta extends at least 15 mm over the internal cervical os at 12 to 16 weeks of gestation, a placenta previa is present at term with a sensitivity of 80% and a positive predictive value of 5.1%.26, 27, 28 The mechanism resulting in the resolution of a first trimester placenta previa with advancing gestation is poorly understood, but may be related to a preferential growth of the placenta toward a better vascularized upper endometrium (trophotropism). According to current guidelines for performance of first trimester fetal ultrasound, it is not recommended to report the presence of placenta previa or low-lying placenta between 11+0 and 13+6 weeks of gestation because the position of the placenta in relation to the cervix at this stage of pregnancy is of less clinical importance as a result of the “migration” phenomenon.7
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree