CHAPTER 4 Positron Emission Tomography
Positron emission tomography (PET) provides information about molecular processes that cannot be obtained with conventional cross-sectional imaging techniques such as ultrasound, computed tomography (CT), and magnetic resonance imaging (MRI). Such information about cellular metabolism provides an additional method for detecting disease, accurately characterizing tissues, and determining tumor activity. When combined with anatomic imaging using a hybrid technique such as PET/CT, metabolic data can be combined with anatomic localization to create a powerful problem-solving tool.
PROBLEM-SOLVING APPLICATIONS OF PET AND PET/CT
In the literature, 18F-FDG PET has been shown to provide incremental clinical value over anatomical imaging in three main clinical scenarios: (1) lesion detection; (2) lesion characterization; and (3) directing cancer therapy. A summary of some current indications for PET imaging are listed in Box 4-1. We will now consider these applications in more detail.
BOX 4-1 Potential Problem-Solving Uses for PET in the Abdomen and Pelvis
Lesion Detection
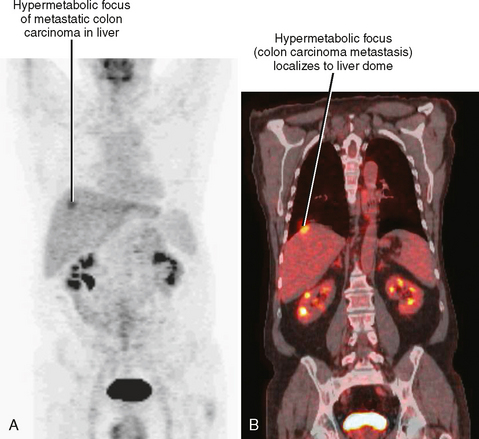
In patients with known malignant tumor, PET/CT may be beneficial in the detection of metastases, particularly those distant from the primary tumor. In a study of colon cancer patients by Cohade and colleagues, 30% more lesions were detected by PET/CT than by CT alone. In this same study, the accuracy of tumor staging increased from 78% to 89% with PET/CT. Similar results were reported in a review by Subhas and colleagues on the use of PET in patients with cervical and endometrial cancer. These authors showed greater than 95% sensitivity and 76% specificity in detecting disease recurrence. Schiepers and colleagues reported sensitivities of 82% to 99% and specificities of approximately 99% for initial staging and posttherapy evaluation of non-Hodgkin lymphoma. In addition to detecting distant metastases in patients with newly diagnosed malignant tumors, PET and PET/CT are useful for detecting metastases in patients with rising tumor markers despite negative anatomic imaging (Figs. 4-1 and 4-2). Unfortunately, very small (<6 mm) lesions such as peritoneal implants often are not evident on PET despite increased metabolism.
When considering the use of PET to detect malignant lesions in the abdomen and pelvis, the avidity of 18F-FDG for various malignancies should be considered. The most common abdominal and pelvic tumors known to be strongly positive on 18F-FDG PET in the majority of cases are listed in Box 4-2.
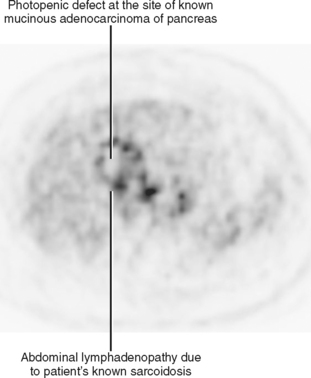
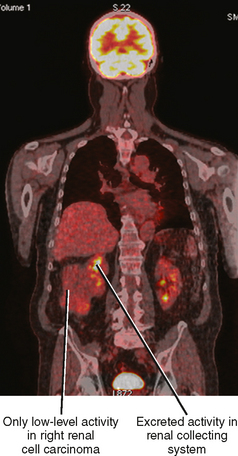
Abdominal malignancies commonly regarded as showing no or little hypermetabolic activity on 18F-FDG PET include mucinous adenocarcinoma, well-differentiated hepatocellular carcinoma, and well-differentiated prostate cancer (Fig. 4-3). Testicular cancer shows variable 18F-FDG uptake. While high-grade lymphomas usually are hypermetabolic, low-grade lymphoma may be difficult to detect with PET/CT. Up to half of all renal cell carcinomas are not 18F-FDG avid (Fig. 4-4). 18F-FDG PET for renal cell carcinoma presents additional challenges even when the tumor is hypermetabolic. Renal cell carcinoma may be isointense to surrounding renal parenchyma on PET images, and renal excretion of 18F-FDG can obscure primary renal lesions adjacent to the renal collecting system. Despite these limitations, PET may be occasionally useful for finding distant metastatic deposits from renal cell carcinoma. In particular, 18F-FDG PET seems to be very sensitive for early detection of lytic bone metastases when compared with plain film, CT or bone scan. For tumors with variable avidity for 18F-FDG, if PET/CT shows hypermetabolic activity in lesions with anatomic correlates, then the study may be a reliable indicator of extent of disease.
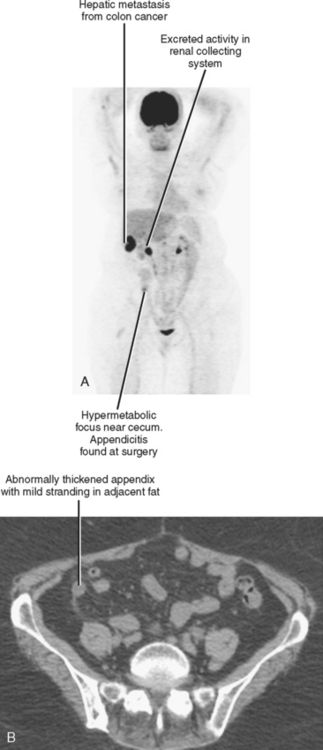
The utility of 18F-FDG PET is not limited to the detection of malignant neoplasms. The highly sensitive nature of PET imaging may be exploited for the evaluation of patients with fever of unknown origin, vasculitis, arthroplasty infections, and inflammatory disorders such as sarcoidosis (Fig. 4-5). Because PET and PET/CT are emerging technologies, not all potential applications are reimbursed by insurers. As with any imaging modality, incidental findings are common on PET and PET/CT scans (Figs. 4-6 and 4-7). Normal physiologic FDG uptake (e.g., bowel, brown fat) is also common and must be distinguished from pathologic FDG activity.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree