Post-surgical scar
Recurrent hernia
Mass effect
No
Yes
Dural traction
Yes
No
Impression on dural sack
Posterolateral
Anterolateral
Relationship with the disk
Contiguity
Continuity
CE
Yes
No
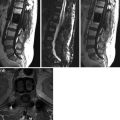
Usually, diskal hernia causes mass effect with impression on the anterolateral dural sack without dural traction and with a clear continuity with the disk. There is no early CE for pathological lack of vascularization; sometimes early peripheral contrast enhancement with delayed (10 min) central diffusion due to the presence of granulation tissue can be found; in later phase (1 month) CE can occur for a diffusion mechanism. Conversely, in surgical scar, in early stage, there is no mass effect, but there is dural traction and contiguity with the disk. Exuberant scar tissue surrounds generally the dural sac (especially along the surgical edges) with possible compression mechanism. Contrast enhancement is early, intense, and diffused thanks to neo-angiogenesis; then trends to significantly disappear at least after 1 year [2, 15, 16]. Therefore, CE-MR images acquired within 7–10 min are important for differential diagnosis.
Complications
Complications are radiculitis, discitis, spondylitis, spondylodiscitis, arachnoidal inflammation, CSF fistula, hematoma, seroma, meningoceles, and pseudo-meningoceles.
Radiculitis
Radiculitis is present in about 20 % of treated patients for lumbar hernia with recurrent or persistent low back pain. It is characterized by pathological CE of the roots, secondary to temporary damage of their barrier caused by surgery or chronic trauma of slipped disk before surgery [17, 18]. This finding should be considered pathological if documented after 6 months, as before, although present and asymptomatic, is not pathological because, it is a part of the regular post-surgery evolution.
Diskitis-Spondylitis-Spondylodiscitis
Infectious complications are appreciable at short time after surgery, characterized by the appearance after a short healthy period of persistent and progressive low back pain associated with inflammatory markers increase. In contrast to diskitis and spondylitis, rare and characterized by signal alteration (T1 hypointensity, T2 hyperintensity) and CE, respectively, of the intervertebral disk and vertebral body, spondylodiscitis is the most common infectious complication (5 %), especially after removal of hernia and disk “curettage” [19].
For accurate and early diagnosis it is important to evaluate symptoms, phlogosis index (fever, elevated ESR, elevated CRP), and MRI. Magnetic resonance shows signal alteration of the disk and subchondral bone (T1 hypointensity, T2 hyperintensity). There is CE with possible and pathological involvement of paravertebral surrounding soft tissues and spine canal with impression on root and dural sack. Risk factors can be related to the nature of the spinal pathology and the surgical procedure such as extensive soft tissue dissection, longer operating time, soft tissue devitalization, kind of surgical instrumentation, and systemic health conditions.
To prevent postoperative infections it is necessary prophylactic antibiotics, meticulous adherence to aseptic technique, and frequent release of retractors to avoid myonecrosis. Use of antibiotics against Gram-positive is frequent (staphylococcus aureus, staphylococcus epidermitis, and beta-hemolytic streptococcus). Sometimes, more aggressive surgical treatment may be required to help the eradication of the infection, providing an adequate wound closure and maintaining spine column mechanical stability.
Abscess
Abscess, alone or in association with diskitis or osteitis, is characterized by a collection that extends from the disk to the epidural space. It is characterized by T2 hyperintensity with irregular peripheral rim CE. This complication, although rare, may occur 2–4 weeks after surgery and may become a possible cause of new neurological deficits requiring urgent decompression.
Arachnoidal Inflammation and CSF Fistula
Arachnoid phlogosis is not common (6–16 % of surgery), especially in opening or fissuring of the dural sack. The three MR patterns in adhesive arachnoiditis are scattered groups of matted or clampe nerve roots, an empty teca sack caused by adhesion of the nerve roots to its walls and an intrathecal soft tissue mass with a broad dural base, representing a large group of matted roots that may obstruct the cerebrospinal fluid pathways [20]. Moreover, there is low CE of cauda roots. CSF fistulae can appear in case of bacterial or fungal meningitis at a distance of months or even years after surgery.
Epidural Hematoma
Epidural hematoma may be associated with an excessive or uncontrolled intraoperative bleeding. A neurological deterioration may occur for compression mechanism, thus requiring decompression [21]. In this case, it is essential for MR evaluation in urgency. It is a liquid collection, with smooth margins, with MRI signal variable in relation to the various stages of hemoglobin degradation.
Seroma
Seromas are sterile cyst paraspinal collections, usually a result of untreated hematoma and then with CSF-like MR signal.
Meningoceles and Pseudomeningoceles
Meningoceles are CSF collections communicating with the subarachnoid space caused by arachnoid herniation through the surgical dural breach. Conversely, pseudomeningoceles is an extra-meningeal collection, with non-homogeneous signal in relation to the presence of proteins or blood with fistula communicating with the subarachnoid space. Both types of CSF collections may extend outside or inside the vertebral canal.
5.1.2 Surgery in Cervical Hernia
Post-surgery imaging of cervical hernia is related to the type of therapeutic procedure. In arthrodesis, bone graft used presents a variable MR signal in relation to intrinsic characteristics of itself and to the variability of the vascularization following surgery. In established arthrodesis interbody space is no longer evident and vertebral bodies have a continuous and homogeneous structure, hardly distinguishable from the adjacent, with low MR signal in all sequences. In anterior microdiskectomy, bone graft has a rectangular shape and varying MR signal. Recently, in microdiskectomy vertebral prostheses of various materials are used (carbon, methacrylate) whose signal appears low in all sequences.
5.2 Vertebroplasty
In postvertebroplasty, imaging shows distribution of synthetic cement (PMMA) in the treated body in which can occur changes in density (X-rays or CT) or signal intensity (MRI) [22–24]. In preoperative is present edema pattern of subchondral spongiosa (hyperintensity in fat suppression STIR); 1 week later there is usually STIR hypointensity in the cement with hyperintense edematous surrounding area also in relation to macrophage reaction; 1 month later hypointensity of cement persists with surrounding thin remaining hyperintensity caused by fibroelastic reaction.
Pattern of cement distribution is variable: rounded, like map, point or oval, homogeneous, or inhomogeneous. Body morphology may appear like vertebra plana, vertebra with depression of the inferior or superior border, biconcave lens. Usually after percutaneous procedure, there is no significant morphological change of vertebral body caused by diffusive and no expansive cement behavior.
< div class='tao-gold-member'>
Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree