Although imaging plays a critical role and has become an integral part in preprocedure evaluation of osteoporotic patients at risk of compression fracture, many treated patients undergo follow-up imaging, for reasons ranging from potential procedure-related complications to development of new symptoms after initial improvement after successful vertebral augmentation (VA). Although imaging is frequently obtained for evaluation of these patients, there is a general lack of knowledge about imaging characteristics of treated vertebrae. This article reviews various indications for post-VA imaging, the appearance of augmented spine on imaging, and the important complications associated with the VA procedure.
Key points
- •
The goal of the vertebral augmentation (VA) procedure is to relieve pain by providing structural stability of the fractured vertebra through the safe injection of a stabilizing material.
- •
Complications from VA procedures are rare and generally result from unrecognized leakage of acrylic bone cement. Meticulous needle-placement technique and fluoroscopic monitoring during careful cement injection contribute to the safe performance of these procedures.
- •
Any worsening of the clinical symptoms during or after the VA procedure should warrant an urgent computed tomography (CT) scan to assess for potential cement leak.
- •
A new neurologic deficit should lead to an emergent CT scan and spine surgical consult.
- •
It is important to be aware of the expected imaging changes in previously augmented vertebrae.
- •
Magnetic resonance imaging should be strongly considered in the evaluation of patients presenting with unexplained new or residual symptoms after an initial successful VA procedure.
- •
Persistent edema and interval height loss after a successful VA procedure should not be interpreted as sufficient evidence of ongoing abnormality at the treated vertebral level.
- •
To make an accurate diagnosis, it is of vital importance to apply the knowledge of expected imaging changes in treated vertebrae, and correlate post-VA imaging findings with new clinical symptoms and the physical examination.
Introduction
The osteoporotic population at risk of compression fracture is sizable, with more than 700,000 new fractures every year in the United States alone. Although imaging plays a critical role and has become an integral part in preprocedure evaluation of these patients, a substantial number of treated patients undergo follow-up imaging. Reasons for obtaining follow-up imaging range from potential procedure-related complications to development of new symptoms after initial improvement from a successful vertebral augmentation (VA). Although imaging is frequently obtained for evaluation of these patients, there is a general lack of knowledge about imaging characteristics of treated vertebrae. This article reviews various indications for post-VA imaging, the appearance of augmented spine on imaging; especially magnetic resonance (MR) imaging, and the important complications associated with the VA procedure.
Introduction
The osteoporotic population at risk of compression fracture is sizable, with more than 700,000 new fractures every year in the United States alone. Although imaging plays a critical role and has become an integral part in preprocedure evaluation of these patients, a substantial number of treated patients undergo follow-up imaging. Reasons for obtaining follow-up imaging range from potential procedure-related complications to development of new symptoms after initial improvement from a successful vertebral augmentation (VA). Although imaging is frequently obtained for evaluation of these patients, there is a general lack of knowledge about imaging characteristics of treated vertebrae. This article reviews various indications for post-VA imaging, the appearance of augmented spine on imaging; especially magnetic resonance (MR) imaging, and the important complications associated with the VA procedure.
Vertebral augmentation
VA is a percutaneous, imaged-guided procedure primarily used for treating back pain associated with vertebral compression fractures that are not effectively treated by conservative or medical therapy. This procedure was first introduced as a technique for the treatment of a symptomatic cervical vertebral hemangioma in 1987. Since then, it has become a valuable and frequently used therapeutic option in the management of back pain caused by osteoporotic and pathologic vertebral compression fractures.
The fundamental aim of the VA procedure is to improve pain, stability, and compressive strength of the vertebral body through the safe injection of a stabilizing material. This goal can be achieved by both vertebroplasty and kyphoplasty. Vertebroplasty involves the injection of acrylic bone cement inside the fractured vertebra using a needle under image guidance, generally x-ray or computed tomography (CT) fluoroscopy. Kyphoplasty, in comparison with vertebroplasty, involves the additional step of creating a cavity inside the diseased vertebral body by temporarily inflating a balloon tamp followed by injection of the bone cement into the cavity.
The usefulness of cross-sectional imaging in preprocedure evaluation of a VA procedure, including MR imaging and CT, is well established. MR imaging provides information on anatomic vertebral collapse and marrow edema that is essential for identifying the location and extent of the disease ( Fig. 1 ). It also provides useful information about any canal or neural compromise. CT is helpful in identifying the potential route of cement extravasations by demonstrating any open fracture lines and osseous destruction, especially in pathologic fractures.
By contrast, the indications and role of imaging in the post-VA setting is not as well described, but is becoming increasingly important.
Reasons for post-VA imaging
Reasons for obtaining post-VA imaging can be broadly categorized as shown in Box 1 .
- 1.
Baseline imaging obtained at the completion of an uneventful procedure
- 2.
Imaging obtained for further evaluation of suspected complications resulting from the augmentation procedure
- 3.
Imaging obtained for evaluation of new or recurrent symptoms after initial improvement
Post-VA Baseline Imaging
Single or biplane x-ray fluoroscopy has been the most widely used modality to perform VA procedures. Radiographic images in 2 orthogonal planes should be obtained at the end of each augmentation procedure for documentation and evaluation of cement distribution; this is generally sufficient for an uneventful treatment of an osteoporotic vertebral compression fracture. Routine postprocedure CT imaging should be considered after treatment of pathologic vertebral fractures. There is increasing use of CT fluoroscopy to perform VA procedures in both osteoporotic and pathologic compression fractures. In such cases, CT images are obtained at the completion of the procedure. This CT scan provides useful baseline information about the distribution of acrylic bone cement and also demonstrates any unsuspected complications including cement leakage, changes in tumor position, procedure-related hematoma, and fracture.
Post-VA Imaging for Suspected Complications
Fortunately, the complication rate with VA procedures is low and ranges from 1.3% for osteoporosis, to 2.5% for hemangiomas, and 10% for neoplastic disease. The commonly encountered complications during VA are further discussed here.
Cement leakage
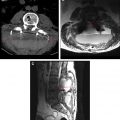
Cement leakage accounts for most symptomatic complications that can occur in association with VA. The primary cause is the leakage of acrylic bone cement beyond the confines of the vertebral body into the epidural and/or paravertebral venous plexus ( Fig. 2 ) or into adjacent spaces via existing fracture lines and cortical destruction. Cement leaks may be seen in up to 15% of routine cases. The overwhelming majority of these leaks is generally small and of no clinical significance.
Any acute worsening of the patient’s clinical symptoms during or immediately after the procedure should warrant a CT scan to assess the size and location of potential cement extravasation. A new neurologic deficit should lead to an immediate CT scan and possible spine surgical consultation. The most common consequence of a symptomatic cement leakage occurs locally, producing radiculopathy from nerve-root irritation or myelopathy from cord compression. Nerve-root irritation may be transient, and is treatable with nonsteroidal anti-inflammatory medications or local steroid injections ( Fig. 3 ). Persistent pain may require surgical removal of the extravasated cement. Cord compression may result in paresis or paralysis, and requires immediate surgical intervention. In one series of 40 patients with osteolytic metastases or myeloma, venous and cortical cement leaks were identified in 29 of 40 patients using postprocedure CT scans. Most of these cement leaks were asymptomatic, but 2 of 8 foraminal cement leaks produced nerve-root compression that required decompressive surgery. In another subsequent series, only 3 of 13 patients with radicular pain required surgical treatments while another 10 responded well to local anesthetic infiltration or medical therapy. Only 1 of 258 treated patients experienced spinal cord compression that required surgery.
Another common location for cement leakage is intravasation into venous structures. Migration of small amounts of acrylic bone cement to the pulmonary veins is generally without clinical significance, but symptomatic pulmonary embolus ( Fig. 4 ) and death have been reported. In otherwise healthy individuals, the lungs can tolerate small acrylic cement emboli without symptoms. However, a large cement bolus can cause pulmonary infarct, and multiple emboli may lead to pulmonary compromise or even death. An operator can take 2 important steps to diagnose this complication. First, it is necessary to monitor the patient’s vital signs and oxygen saturation before, during, and after the VA procedure. Any sudden and unexplained alteration of the patient’s respiratory rate, heart rate, or oxygen saturation should raise the possibility of a potential acute pulmonary embolic event. Second, careful periprocedural fluoroscopic monitoring will help the operator to detect cement extravasation and, therefore, stop the cement injection. Chest radiographs and/or CT of the thorax may be required to confirm the presence of cement emboli.

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree