POSTERIOR VISUAL PATHWAYS: CHIASM TO VISUAL CORTEX
KEY POINTS
- Magnetic resonance imaging/magnetic resonance angiography is the primary tool for looking for a structural cause for a cranial neuropathy that is likely involving the visual pathways.
- Magnetic resonance imaging and magnetic resonance angiography will confidently exclude structural pathology causing compression of these pathways in properly screened populations, assuming high-quality focused protocols are used.
- Computed tomography/computed tomographic angiography may substitute for magnetic resonance imaging/magnetic resonance angiography, but it is a second-line study except in selected circumstances.
- Diagnostic imaging, even performed optimally, may fail to find a reason for these deficits in most patients and never entirely excludes meningeal pathology.
INTRODUCTION
Clinical Presentation
The visual pathways from the optic chiasm and tracts entry into the brain to the visual cortex are primarily in the realm of the neuroimaging that involves pathology that is often outside the scope of a complete consideration in this resource. This chapter is meant to heighten awareness that those imaging the visual pathways must take into account any disease that interferes with vision along this entire functional pathway and design protocols and interpretive search patterns that account for the entire pathway.
Conditions affecting these pathways will present with diminished visual acuity and/or visual field deficits. Findings associated with diminished visual acuity and field defects that involve the oculomotor (IIIrd), trochlear (IVth), and abducens (VIth) nerves and produce ocular dysmotility, pupillary dysfunction, and/or ptosis will usually localize the problem at or more anteriorly than the chiasm and paracavernous region except for isolated sixth nerve problems that move the search to the clivus and posterior fossa. Some diseases will involve both the anterior and posterior pathways such as the tumors and hamartomas of neurofibromatosis type 1 and vascular malformations.
APPLIED ANATOMY
The various segments of the optic nerve, like the other cranial nerves, are best considered segmentally according to the particular territory through which it travels. The posterior segment includes the cisternal portion of the optic nerve, the optic chiasm, and the optic tract. After leaving the optic canal, the cisternal portion of the optic nerve passes superior and medial to the supraclinoid segment of the internal carotid artery. It joins with the nerve on the opposite side within the suprasellar cistern to form the optic chiasm. The optic chiasm is found in a depression formed in the base of the hypothalamus. The chiasm is outlined superiorly by the optic and infundibular recesses of the third ventricle. The chiasm then splits, and the visual pathway continues posteriorly on each side as the optic tracts.
The optic tracts course posteriorly, juxtaposed to the inferior and lateral surface of the hypothalamus. The optic tract enters the brain along the mesial surface of the temporal lobe and terminates in the lateral geniculate body, the latter found at the junction between the rostral brain stem and thalamus (Fig. 44.2).
The lateral geniculate bodies are located at the junction of the thalamus and mesencephalon. Optic fibers leave the lateral geniculate bodies in the form of optic radiations, which sweep posteriorly around the trigone of the lateral ventricle. A portion of these nerve fibers dip downward into the mid- to inferior aspect of the temporal lobe as the Meyer loop. The remaining fibers stay within the superior aspect of the temporal lobe. Ultimately, they pass toward the calcarine fissure, terminating in the visual cortex.
IMAGING APPROACH
Techniques and Relevant Aspects
Specific protocols for computed tomography (CT) and magnetic resonance (MR) studies for investigating disorders of visual acuity and visual field deficits appear in Appendixes A and B. Evaluation of the posterior visual pathways will almost always be primarily by magnetic resonance imaging (MRI).
Diagnostic catheter angiography may be necessary in some instances to confirm the diagnosis of an aneurysm if it is equivocal on imaging.
Pros and Cons
Since these lesions will be intracranial and possibly intra-axial or caused by leptomeningeal pathology, MRI is used as the primary diagnostic tool. It must always be kept in mind that an MRI cannot exclude meningeal pathology. MRI or magnetic resonance angiography (MRA) can almost always confidently exclude causative structural compressive pathology and many intra-axial considerations. CT and computed tomographic angiography (CTA) are used selectively if better vessel or bone evaluation becomes necessary or for some reason when an MRI cannot be done. For example, as CTA can more confidently exclude an aneurysm, it may be the requested examination if a physician is particularly worried about a posterior communicating artery aneurysm, but aneurysms that impair vision are usually large enough to be detected by MRI/MRA.

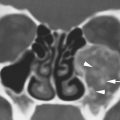
FIGURE 77.1. A patient treated for carotid artery aneurysm that required wrapping of the aneurysm. The patient then developed a vision field deficit and loss of vision. A: Contrast-enhanced T1-weighted (T1W) coronal image shows the “muslinoma” created by the wrapping material as an enhancing mass (arrow) extending to compress and envelop the optic chiasm (arrowhead). B: Contrast-enhanced T1W axial image shows the masslike portion (arrow) and a more infiltrative pattern extending to the optic chiasm (arrowhead).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree