Primary or metastatic spine tumors can present with pain and/or neurologic compromise depending on their location within the spinal axis. Metastases and multiple myeloma comprise most of these lesions. Management of spinal tumors includes surgical decompression with stabilization (neo), adjuvant chemotherapy and radiation therapy, curettage, bone grafting, bone marrow replacement, and palliative treatment with vertebral augmentation. Pre- and postoperative imaging plays a critical role in the diagnosis and management of patients with spinal tumors. This article reviews postoperative imaging of the spine, including imaging protocols, immediate and long-term routine imaging findings, and emergent findings in symptomatic patients.
Key points
- •
Postoperative imaging of patients with spinal tumors plays a vital role in their management.
- •
Advances in magnetic resonance imaging, CT, and nuclear medicine have optimized postoperative imaging in patients with spinal cancer.
- •
Understanding of imaging protocols, expected postoperative findings, postoperative complications, and the appearance of tumor residual/recurrence is crucial for radiologists.
Introduction
Spine tumors can be classified according to their location in the spine: extradural, intradural extramedullary, and intramedullary. Metastatic spinal tumors are the most common type of malignant lesions of the spine, accounting for an estimated 70% of all spinal tumors. Common primary cancers that spread to the spine are lung, prostate, and breast cancer. The spine is the third most common site for metastatic disease and is the most common site for osseous metastases. Metastases to the spine can involve the bone, epidural space, spinal cord, and leptomeninges. Approximately 95% of metastatic spinal lesions are extradural in location, consisting of pure epidural lesions and lesions arising from the vertebral bodies, spreading to the epidural space.
Most extradural tumors are metastatic, and the thoracic spine is the most commonly affected site. Multiple myeloma, lymphoma, and leukemia can also involve the spine and often present with multifocal or single-level extradural involvement. Primary malignant extradural tumors, such as osteosarcomas and Ewing sarcomas, are less common, as are primary nonmalignant entities, such as osteoid osteomas and aneurysmal bone cysts. Management of extradural tumors includes gross total or subtotal surgical resection for surgical decompression with stabilization, chemotherapy, radiation therapy, and bone grafting.
Intradural extramedullary spread of systemic cancer comprises approximately 5% to 6% of spinal metastases. Primary intradural extramedullary tumors comprise approximately 66% of all primary spinal tumors. The most common intradural extramedullary tumors are schwannomas, followed by meningiomas. These tumors are usually slow-growing tumors that are treated by surgical resection only if patients exhibit significant neurologic symptoms caused by cord compression. The location of the tumor (ie, ventral or dorsal to the spinal cord) determines the operative approach: anterior, lateral, or posterior.
Intramedullary metastases are rare and comprise 0.5% to 1% of spinal metastases. Primary intramedullary tumors include glial neoplasms, most commonly ependymomas and astrocytomas, and nonglial neoplasms, such as hemangioblastomas. These tumors are commonly treated with surgical resection. For ependymomas and astrocytomas, adjuvant radiation therapy may be used for lesions that undergo subtotal resection, and chemotherapy for failed radiation therapy or recurrence.
The treatment of spinal metastatic disease is multidisciplinary, dependent on patient presentation, and mostly palliative. Patients who present with pain without neurologic symptoms are treated primarily with site-directed radiation therapy and chemotherapy. Surgery is indicated for patients presenting with progressive neurologic deficits, neural compression due to retropulsed bone or epidural disease, spinal deformity or instability, and for treatment of radiation-resistant tumors. A variety of surgical methods are available to treat metastatic disease to the spine. Dorsal spinal decompression and stabilization is the standard surgical technique to treat thoracic and lumbar metastases. Cervical metastases are treated with ventral decompression with corpectomy, vertebral body replacement, and ventral, stable-angle plate osteosynthesis.
Introduction
Spine tumors can be classified according to their location in the spine: extradural, intradural extramedullary, and intramedullary. Metastatic spinal tumors are the most common type of malignant lesions of the spine, accounting for an estimated 70% of all spinal tumors. Common primary cancers that spread to the spine are lung, prostate, and breast cancer. The spine is the third most common site for metastatic disease and is the most common site for osseous metastases. Metastases to the spine can involve the bone, epidural space, spinal cord, and leptomeninges. Approximately 95% of metastatic spinal lesions are extradural in location, consisting of pure epidural lesions and lesions arising from the vertebral bodies, spreading to the epidural space.
Most extradural tumors are metastatic, and the thoracic spine is the most commonly affected site. Multiple myeloma, lymphoma, and leukemia can also involve the spine and often present with multifocal or single-level extradural involvement. Primary malignant extradural tumors, such as osteosarcomas and Ewing sarcomas, are less common, as are primary nonmalignant entities, such as osteoid osteomas and aneurysmal bone cysts. Management of extradural tumors includes gross total or subtotal surgical resection for surgical decompression with stabilization, chemotherapy, radiation therapy, and bone grafting.
Intradural extramedullary spread of systemic cancer comprises approximately 5% to 6% of spinal metastases. Primary intradural extramedullary tumors comprise approximately 66% of all primary spinal tumors. The most common intradural extramedullary tumors are schwannomas, followed by meningiomas. These tumors are usually slow-growing tumors that are treated by surgical resection only if patients exhibit significant neurologic symptoms caused by cord compression. The location of the tumor (ie, ventral or dorsal to the spinal cord) determines the operative approach: anterior, lateral, or posterior.
Intramedullary metastases are rare and comprise 0.5% to 1% of spinal metastases. Primary intramedullary tumors include glial neoplasms, most commonly ependymomas and astrocytomas, and nonglial neoplasms, such as hemangioblastomas. These tumors are commonly treated with surgical resection. For ependymomas and astrocytomas, adjuvant radiation therapy may be used for lesions that undergo subtotal resection, and chemotherapy for failed radiation therapy or recurrence.
The treatment of spinal metastatic disease is multidisciplinary, dependent on patient presentation, and mostly palliative. Patients who present with pain without neurologic symptoms are treated primarily with site-directed radiation therapy and chemotherapy. Surgery is indicated for patients presenting with progressive neurologic deficits, neural compression due to retropulsed bone or epidural disease, spinal deformity or instability, and for treatment of radiation-resistant tumors. A variety of surgical methods are available to treat metastatic disease to the spine. Dorsal spinal decompression and stabilization is the standard surgical technique to treat thoracic and lumbar metastases. Cervical metastases are treated with ventral decompression with corpectomy, vertebral body replacement, and ventral, stable-angle plate osteosynthesis.
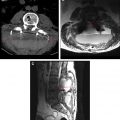
Indications for postoperative imaging
In the immediate postoperative period, imaging is performed to assess the extent of tumor resection. If surgical debulking of the tumor has been performed with the intention of subsequent radiation therapy or chemotherapy, an immediate follow-up magnetic resonance (MR) imaging is generally obtained to establish a baseline before therapy. Comparison with the preoperative imaging examination is a critical step in interpreting the postoperative study properly and in making distinctions between postoperative changes and the presence of residual neoplasm. Imaging evaluation is sometimes obtained on an emergent basis in symptomatic patients to assess for postsurgical complications. Common postsurgical complications in this patient population include hematoma, infection, ischemia, cerebrospinal fluid (CSF) leak, and malpositioning of hardware ( Table 1 ).
| Immediate | Routine |
|
| Emergent/symptomatic |
| |
| Long-term | Routine (4–6 mo) | Assess for tumor recurrence or progression |
| Emergent/symptomatic |
|
Long-term routine follow-up imaging is obtained 4 to 6 months after surgery in the asymptomatic patient to assess for tumor recurrence or progression of disease. Long-term imaging is also obtained in the symptomatic patient to assess for hardware malpositioning or failure and to assess for treatment-related complications, such as radiation therapy–related vertebral compression fractures, radiation myositis, and radiation myelitis.
Imaging protocols
MR Imaging
Following tumor resection, postsurgical inflammation and neovascularity may develop within 24 hours, causing enhancement. Early MR imaging is therefore necessary to establish an accurate baseline, allowing the radiologist to distinguish between tumoral and postsurgical enhancement.
Due to the oftentimes subtle nature of tumoral enhancement and the difficulty in identifying it in the background of postsurgical scarring, postcontrast sequences must be performed with reliable fat saturation. Frequency-selective fat-saturation methods depend on the different resonance frequencies of water and fat. To suppress the fat signal accurately, the magnetic field must be homogeneous. This suppression is not possible in postoperative spines with hardware or metallic debris. Therefore, an alternative method of fat saturation with short tau inversion recovery (STIR) is preferred. STIR imaging relies on the different relaxation times of tissues, using a 180° inversion pulse, allowing the longitudinal recovery of fat to reach a null point, and then applying a 90° radiofrequency pulse before echoing. However, STIR imaging also has its drawbacks, suffering from decreased signal-to-noise ratios, as well as increased scan times. Another method of obtaining fat suppression is achieved with the Dixon technique, which is a water-fat separation technique based on the different precessing velocities of water and fat. The Dixon method was previously hampered by field inhomogeneities. However, new variants, including the iterative decomposition of water and fat with echo asymmetry and least-squares estimation, have shown promise in separating water and fat while taking into account field inhomogeneities, resulting in optimal, uniform fat suppression with high signal-to-noise ratio and image quality.
Another challenge in imaging the postoperative spine is the susceptibility artifact caused by metallic hardware, which results in signal loss and geometric distortion, which can be compensated by thinner slices, smaller voxels, and excessive radiofrequency refocusing. New techniques using 3D volumetric fast spin-echo imaging are now used with isotropic voxels, which provide high signal-to-noise ratio and spatial resolution, with relatively short scan times, using parallel imaging and phased array coils and sequences obtained with long echo train lengths. Resultant blurring is compensated for by flip angle modulations during readout (CUBE, Volumetric ISotropic T2-weighted Acquisition, Sampling Perfection with Application optimized Contrasts using flip-angle Evolutions).
In addition, diffusion-weighted imaging (DWI) has been found to be a helpful adjunct to traditional sequences in spine imaging and may be particularly useful for postoperative tumor surveillance patients. DWI offers unique information on tissue characteristics by reflecting the motion of water molecules in tissues. In the initial postoperative period, fluid collections may be characterized with DWI. Abscesses with pus will generally demonstrate high signal on DWI with reduced apparent diffusion coefficient, whereas seromas will not. Furthermore, there has been research suggesting the utility of DWI in patients with osseous metastases. In the differentiation of acute benign osteoporotic compression fractures from pathologic compression fractures, T1 and T2 sequences are inadequate, often demonstrating similar signal intensities in both conditions. DWI has proven helpful in this distinction with hyperintense signal in acute pathologic compression fractures and hypointense signal in acute benign fractures. However, research on the utility of DWI in detecting vertebral metastases have yielded varying results with some studies demonstrating that it does not surpass traditional T1-weighted sequences and others demonstrating an advantage to adding the DWI sequence. Although more studies need to be performed on the use of DWI in the follow-up of treated vertebral metastases, there have been several small studies suggesting their usefulness with decreased signal intensity in lesions that have undergone successful therapy.
Computed Tomography
Computed tomography (CT) is the preferred imaging modality to evaluate spinal hardware for malpositioning and fracture. However, the metallic hardware produces significant artifact on CT. When spinal fixation hardware is present, imaging parameters should be optimized to minimize artifact. Imaging techniques, including dual-energy CT, are now available to minimize many of these artifacts and are discussed elsewhere in this issue.
Nuclear Medicine
Common indications for nuclear medicine in assessing the postoperative spine include spinal infection, pseudoarthrosis, and recurrence or progression of tumors. Radionuclides that can be used to diagnose spinal infections include 99 Technetium m -methylene diphosphonate, single-photon emission computed tomography (SPECT), 3-phase bone, 67 Gallium citrate, 111 Indium oxine–labeled leukocytes, and 18-F-fluoro-deoxy- d -glucose (FDG)-labeled positron emission tomographic (PET) scans.
With the advent of new cancer therapies, patients with metastatic disease are demonstrating longer lifespans than before, and new imaging modalities are needed to monitor vertebral metastases. Spinal FDG-PET/CT has demonstrated accuracy in the detection of metastases with increased tracer uptake reflecting the increased glucose metabolism in lesions. More importantly, it is becoming an emerging modality in assisting radiation therapy planning following surgical debulking due to its ability to delineate lesions despite overlying hardware. It has also been shown to monitor response to therapy effectively. Continued research is being performed with various radionuclides for PET imaging with increased specificity for certain cancers and seems promising.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree