Postoperative State, Stomach and Duodenum
Michael P. Federle, MD, FACR
Key Facts
Imaging
Billroth 1 (B1) procedure
Antrectomy with gastroduodenostomy
Billroth 2 (B2) procedure
Distal gastrectomy with gastrojejunostomy
Surgery for gastric cancer
May be some variant of B1 or B2, up to total gastrectomy
Complications include recurrent tumor and acute or chronic sequelae of surgery
Recurrent or new carcinoma
Local, lymph node, peritoneal, hematogenous
Bezoar formation
Conforms to shape of stomach, traps air within
Anastomotic leak
CT may detect indirect signs of leaks missed on UGI series (up to 50% of cases)
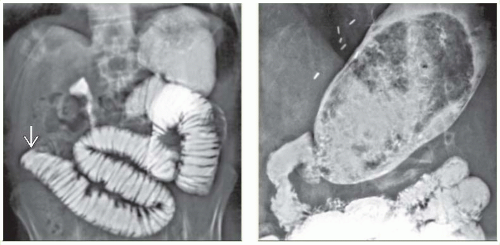
Duodenal stump leakage
Loculated collection of fluid in subhepatic space
Rarely diagnosed on UGI
Jejunogastric intussusception
Rare complication of B2 procedure
Afferent loop syndrome
Obstruction of afferent loop at or near anastomosis → dilation of duodenum
Diagnostic Checklist
Upper GI series is 1st-line test for detecting mechanical complications of gastric surgery
CT is optimal test for general surveillance for postoperative complications
PET/CT is optimal imaging test for surveillance of recurrent gastric carcinoma
Abscessogram may identify leak as source of infection
IMAGING
General Features
Many or most fluoroscopic exams of esophagus, stomach, and duodenum are now performed for patients who have surgically altered anatomy
Some procedures are so common they are discussed separately
Postoperative state, esophagus
Includes esophagectomy with gastric pull-through
Fundoplication complications
Bariatric surgery
Goal for evaluating remaining procedures
Define expected postoperative anatomy
Describe imaging approaches to evaluation of postoperative patients
Describe imaging and clinical findings for various complications
Surgical Procedures
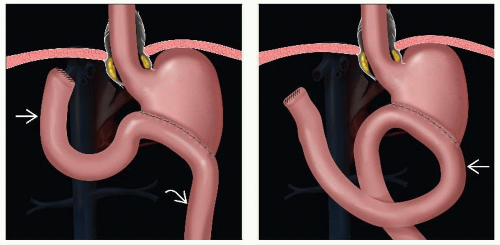
Billroth 1 (B1) procedure
Antrectomy with gastroduodenostomy
Polya variation: Entire excised end of gastric stump is used for anastomosis
Hofmeister: Only a portion (usually greater curvature portion) is used
Billroth 2 (B2) procedure
Distal gastrectomy with gastrojejunostomy
Stomach may be anastomosed to Roux limb or loop of jejunum
Anastomosis is side-to-side
Variable length of duodenum and jejunum forms proximal or afferent loop
Carries pancreaticobiliary secretions toward stomach
Distal or efferent loop carries food and fluid downstream
Isoperistaltic anastomosis (right-to-left)
Afferent limb 1st contacts lesser curve side of anastomosis; efferent limb contacts distal side
Antiperistaltic (left-to-right)
Opposite configuration
Duodenal stump is closed by sutures
Usually filled with gas bubble on postoperative CT
Located in subhepatic space
Anastomotic loop may be brought to gastric remnant in antecolic or retrocolic position
Antecolic: Results in longer afferent loop
Retrocolic: Shorter afferent loop; considered more “physiological” and usually preferred
Surgery for gastric cancer
Varies according to site and size of tumor
May be some variant of B1 or B2, up to total gastrectomy
Gastrectomy usually results in creation of esophagojejunal anastomosis
Usually involves extensive denervation of stomach
Alters gastric and intestinal motility and absorption
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree