Fig. 3.1
J2 IJV segment in transverse scanning plane. Sometimes there is a huge variation between IJV expiratory CSA (figure above) and inspiratory CSA (figure below) during normal breath. See the corresponding movie of breath dynamics (Movie 3.1)
Fig. 3.2
Schematic drawing of J2 IJV CSA variations during normal breath in a normal subject (i.e., a subject whose responses are congruent with the physiological data described in the chapter) (left side of the image) and in a subject with opposite behavior (right side of the image), during inspiration (Fig. 3.2a) and in the end-expiratory phase (Fig. 3.2b). See also Movie 3.2
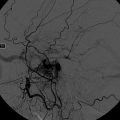
Fig. 3.3
Longitudinal scan of J1 IJV in B-mode and in color mode during normal breath. In B-mode (top picture), the two valve leaflets opening can be seen. In color mode (bottom picture), an orthodromic flow of IJV is evident with the posterior leaflet separating the orthodromic flow laminae from the valve sinus, where a minimal stasis with retrograde filling is normal
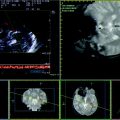
Fig. 3.4
Longitudinal scan of J1 IJV in B-mode and in color mode during the Valsalva maneuver. In B-mode (top left picture), it is well evident the quite perfect closeness of the valve leaflets with a minimal discontinuity (arrow) (see also Movie 3.3). In color mode, the three sequential images show from top to bottom right picture that the regurgitation jet progressively fills the prevalvular IJV segment with an increasing aliasing, as in the Movie 3.4
Fig. 3.5
Longitudinal scan of J1 IJV in color mode. In the above picture, the Doppler waveform is sampled during normal breath, near the valve plan, without evident reflux. In the picture below, the Doppler waveform is sampled during the straining phase of the Valsalva maneuver, eliciting a flow decrease near to zero
Another relevant item raised from this study is that the dynamic balance between venous outflow and arterial inflow is also dependent on the biomechanic status of the cerebrovascular system. Indeed in seated position, a significant reduction in the venous outflow pulsatility is found without changes in the pulsatility of the arterial inflow. This point could be explained by the increased compliance of the venous routes system (2.8-fold increase in the intracranial compliance index), i.e., by a decreased blood volume in this vessels in upright position in comparison with the supine position, according to the gravity [13].
3.2 Activation Tests
Either ultrasound or MRI studies on healthy volunteers using the phase contrast technique at the IJV level [14] confirmed the physiological data about the relation between the breath cycle and IJV flow parameters, both for size and for the measure of the blood flow.
During the inspiration, the intrathoracic pressure decreases, becoming more negative and reducing the resistance to outflow for the IJV, while during the expiration, the intrathoracic pressure increases, becoming less negative and increasing the resistance to the IJV outflow. Therefore, lacking diseases that can affect the central venous pressure and significant valve incontinence, it should be expected that IJV CSA progressively decreases during inspiration and increases during expiration. Moreover, confirming this relation between IJV CSA and the breath cycle, the application of an end-expiratory positive pressure can increase IJV CSA until a maximal value correspondent to a positive pressure of 12 cm H2O [15].
The more known and standardized activation test is the Valsalva maneuver, whose effects on the central venous pressure are well studied and demonstrated. The Valsalva maneuver defines a forced expiration against a closed glottis; during each phase, different changes occur in several parameters, as intrathoracic pressure, and consequently in venous outflow, cardiac output, arterial pressure, heart rate, and so on. The starting phase of a Valsalva maneuver involves the contraction of diaphragm and intercostal muscles, that make the intrathoracic pressure positive, though a compression of the thoracic great vessels and cardiac chambers. The association of venous compression and increased right atrial pressure increases the resistance to the cerebral venous outflow into the central veins. The transiently decreased cardiac filling causes a cardiac output reduction, but it is associated with a transient increase in aortic pressure because of the compression of the thoracic aorta causes (phase I).
In phase II, the aortic pressure progressively falls, following the fall in cardiac output, and the heart rate increases (Figs. 3.6, 3.7, 3.8, 3.9, 3.10, 3.11).