PRESEPTAL COMPARTMENT: BENIGN AND MALIGNANT TUMORS
KEY POINTS
- Imaging is not required in many patients with benign and malignant tumors of the preseptal compartment.
- Imaging when tumors are known to be present can be used to identify the extent of disease and predict the likely morbidity of curative treatment.
- Imaging can be used to identify possible sources of the tumor and complicating factors that will alter medical decision making in selected cases.
- Imaging findings can markedly alter medical decision making if a process other than a tumor is identified.
Any orbital mass or disease process may be approached by first establishing whether it is preseptal (Chapters 70 and 71) or postseptal (Chapters 57–60, 62, and 64). Preseptal problems most commonly arise from the skin, eyelids, lacrimal gland (Chapter 65), and nasolacrimal drainage apparatus (Chapter 68), all of which are components of the preseptal space. The vast majority of these problems do not come to imaging. This chapter considers preseptal benign and malignant tumors, which arise from sources other than the lacrimal gland and nasolacrimal drainage system, and those arising in this location that might spread across the orbital compartments and related spaces.
Tumors may be of local origin or related to systemic disease. Practically, the preseptal space is only infrequently secondarily involved in systemic malignancies such as lymphoma or metastatic disease. Primary benign and malignant tumors arise in the skin and eyelid with few due to secondary spread from conditions of the sinonasal region (Chapters 89 and 90), lacrimal gland (Chapter 66), and lacrimal drainage system (Chapter 69).
ANATOMIC AND DEVELOPMENTAL CONSIDERATIONS
Applied Anatomy
The relevant anatomy of the preseptal soft tissues, orbital septum, lacrimal gland, and nasolacrimal drainage system is discussed in detail in Chapter 44.
IMAGING APPROACH
Techniques and Relevant Aspects
The preseptal soft tissues are studied with computed tomography (CT) and magnetic resonance (MR) techniques described in detail in Chapters 44 and 45. Specific CT protocols by indications are detailed in Appendix A. Specific MR protocols by indications are outlined in Appendix B. Almost all studies to investigate potential preseptal tumors are done with contrast.
Pros and Cons
Masses of and around the preseptal soft tissues are studied primarily with CT, with magnetic resonance imaging (MRI) held in reserve for selected cases.
CT typically is used to identify bone changes and survey the surrounding soft tissues for a likely infiltrating mass. It is also used to determine whether the mass has extended to postseptal soft tissues or if there has been perineural spread to regional lymph nodes.
MRI helps to characterize masses and to search for possible perineural spread better than CT. It is also used to determine whether the mass has extended to postseptal soft tissues; in this regard, it may be better than CT, given that high-quality images are available. MR also helps determine if perineural spread or regional lymph nodes is present.
SPECIFIC DISEASE/CONDITION
Benign and Malignant Tumors and Their Mimics
Etiology
Primary tumors of the preseptal soft tissues are common. Epithelial skin malignancies are most common, with basal cell, squamous cell, and melanoma most common. Merkle cell cancer and angiosarcomas are relatively uncommon to rare.1,2 These epithelial malignancies may also come from dermal/ adnexal skin elements mainly arising from the eyelid and morphologically indistinguishable from other cancers on imaging studies. Lymphoma may arise primarily in the preseptal soft tissues but is more commonly an extension of tumor arising from the lacrimal gland, lacrimal drainage system, and postseptal orbital spaces. Sometimes, a sinonasal cancer will present with preseptal soft tissue swelling.
Primary and metastatic tumors and other conditions within bone such as fibrous dysplasias or the histiocytoses may spread to the preseptal soft tissues or mimic a preseptal condition (Figs. 44.69, 69.3, 69.4, and 70.1).
Prevalence and Epidemiology
Skin cancers are discussed in Chapter 24. Other tumors are relatively rare and sporadic occurrences.
Clinical Presentation
Epithelial skin lesions are clinically obvious. Subcutaneous nodules may be due to cancer but might also be benign conditions such as a dermoid cyst in a child or a retention cyst. Localization more medially suggests a sinonasal or nasolacrimal system origin (Chapters 67–69), and a superior lateral localization suggests a lacrimal gland or frontal bone or sinus origin (Chapters 65 and 66).
Some tumors cause secondary nasolacrimal obstruction and inflammation and present sometimes with bloody tearing (epiphora), epistaxis, medial canthal region pain, recurrent conjunctivitis, and nasolacrimal sac distension. This mimics the presentation of inflammatory disease.
Pathophysiology and Patterns of Disease
The general spread patterns of benign and malignant tumors that might affect the skin, lacrimal drainage system, and lacrimal gland are presented in Chapters 21, 23, and 24. Lymphoma is discussed in Chapter 27.
Tumors in the preseptal area arise from the nasolacrimal apparatus, the conjunctiva, the adjacent facial skin, or structures of the eyelids. The lesions by definition will be anterior to or involving attachments of the orbital septum and involving structures related to the eyelid such as the palpebral ligaments, tarsal plates, and the lacrimal sac (Fig. 44.69). Swelling of preseptal soft tissues and obliteration of fat compared to the opposite side may be obvious. It is important to search for subtle erosion of bone, especially along the orbital septum attachments. Spread of lesions to postseptal spaces may be direct, via vessels, or along nerves. Postseptal spread will be manifest as alterations of the usual appearance of postseptal intraconal and/or extraconal fat. If phlebothrombosis is present, it may progress to involve the major orbital veins; the veins will increase in size, and an intraluminal clot may become visible (Chapters 15 and 59). Edema of the intraorbital fat is a generic finding that may be seen in venous congestion, thrombosis, increased venous pressure associated with regional arteriovenous fistulas, inflammation, or tumor.
Manifestations and Findings
Computed Tomography and Magnetic Resonance Imaging
The general CT and MRI patterns of benign and malignant tumors that might affect the preseptal soft tissues are presented in Chapters 21, 23, and 24. Lymphoma is discussed in Chapter 27. MR might also identify pathology extrinsic to the preseptal soft tissues, either benign or malignant, that will explain the clinical findings.
CT does reasonably well at showing the deep extent of soft tissue masses. It may also be used to determine whether the mass has extended to postseptal soft tissues, although in some cases it might not be as good as a high-quality MRI in this regard (Figs. 24.19, 24.20, and 71.1–71.4).
CT is superb for showing bony erosion (Figs. 24.19C, 24.20D, and 71.3). Bone changes may be not be apparent on MRI since this is essentially cortical bone being demineralized. The earliest bone erosion in skin or other cancers may be of the anterior and posterior lacrimal crests, the posterior lacrimal crest being where the orbital septum attaches, and such erosion may produce only a subtle change. Erosion of the posterior lacrimal crest is an indicator of orbital septum involvement since that crest is a point of attachment of the orbital septum. MRI may show soft tissue involvement of the septum but can miss this bony erosion as a sign of early orbital septum invasion (Figs. 24.19C, 24.20D, 71.3, and 71.4).
MR can screen for perineural spread—V2 being at most risk—more definitively than CT (Figs. 24.19C and 24.20D).
CT and MRI might demonstrate metastatic adenopathy in facial, level 1, or other lymph node groups.
Differential Diagnosis
From Clinical Data
Distention of the lacrimal sac together with tearing and pain and inflammation in the medial canthal area strongly suggest a nasolacrimal drainage system origin. Signs and symptoms of sinonasal disease suggest that origin. Localization to the upper outer orbital margin suggests a lacrimal gland or frontal bone/ sinus origin.
Nasolacrimal tumors frequently cause obstruction and inflammation and present sometimes with bloody tearing (epiphora), epistaxis, medial canthal region pain, recurrent conjunctivitis, and nasolacrimal sac distension (Chapter 69). In this way, they mimic the presentation of preseptal inflammatory disease but usually not tumor. The presence of an obvious skin cancer or palpable, nontender mass in the medial canthus vicinity or a nasal cavity mass at the terminal end of the duct will confirm or at least help raise the index of suspicion for tumor.

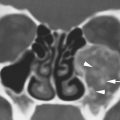
FIGURE 71.1. Magnetic resonance imaging (MRI) studies of two patients with preseptal low-flow vascular malformations. A, B: Patient 1 is a pediatric patient with a venolymphatic malformation (VLM). In (A), compared to the normal preseptal soft tissue structures of the eyelid (arrowhead) on the right, the VLM on the left (arrow) is obviously preseptal in location and involving the soft tissues of the eyelid, likely displacing the septum and tarsal plate posteriorly (white arrowheads). In (B), T2-weighted MRI demonstrates the VLM (arrow) to be contained within the preseptal soft tissues compared to those on the opposite side (arrowhead). C: Patient 2 is an adult with a VLM demonstrating the precision of MRI in evaluating preseptal versus postseptal locations of abnormal masses. On the patient’s left, the orbital septum is identified (black arrowhead). On the right, the VLM (arrow) is limited by a displaced and slightly thickened orbital septum (white arrowhead).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree